OTITIS MEDIA WITH EFFUSION
Otitis media with effusion was first described by Politzer in 1884. It is an insidious condition, defined by the collection of nearly sterile, non-purulent effusion in the middle ear cleft behind an intact tympanic membrane without signs and symptoms of an acute infection. More commonly the effusion is thick and viscid but sometimes it may be thin and serous. OME is commonly seen in school-going children and is the most common cause of hearing impairment in children causing delayed speech and language development, learning and behavioural problems.
- The term “glue ear” is used when the effusion is thick and glue-like also called mucoid otitis media.
- The term “chronic OME” is used when the effusion persists for 3 months or longer.
EPIDEMIOLOGY.
- It usually occurs following respiratory tract infection and otalgia with an episode of acute otitis media.
- 90% of children usually have at least one episode of OME by the age of 4 years.
- It is more common in winter than in summer.
PREDISPOSING FACTORS.
- Young age
- Family history of otitis media
- Bottle feeding.
- Day care attendance
- Exposure to tobacco smoke
- Low socioeconomic level
PATHOGENESIS. Three main mechanisms are thought to be responsible.
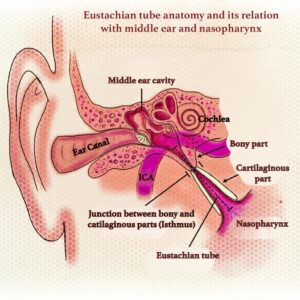
- The Eustachian tube and anterior mesotympanum are lined by ciliated, pseudostratified columnar respiratory epithelium which contains both goblet cells and mucus-secreting glands. Inflammation of both goblet cells and mucus-secreting glands causes production of a serous or mucus effusion which results in OME.
- Malfunctioning eustachian tube fails to aerate the middle ear causing negative pressure and hypoxia in the middle ear leading to passive transudation of fluid into middle ear. Excessive production of exudate and reduced drainage due to malfunctioning eustachian tube leads to collection of exudate in the middle ear.
- Biopsies of middle ear mucosa in these cases have confirmed increase in number of mucus or serous-secreting cells.
EFFECTS OF ACUTE AND CHRONIC TUBAL BLOCKAGE.
| Acute | Chronic |
| Eustachian tube blockage ↓ Resorption of air from the middle ear ↓ Development of negative pressure in the middle ear ↓ Retraction of the tympanic membrane ↓ Transudate in ME/haemorrhage (acute OME) |
Eustachian tube blockage/dysfunction ↓ OME (thin watery or mucoid discharge) ↓ Atelectatic ear/perforation ↓ Retraction pocket/cholesteatoma ↓ Erosion of the incudostapedial joint |
AETIOLOGY.
- Malfunctioning of eustachian tube. The causes are:
- Hypertrophy of adenoids.
- Chronic rhinitis and sinusitis.
- Chronic tonsillitis. Enlarged tonsils mechanically obstruct the movements of soft palate and interfere with the physiological opening of eustachian tube.
- Benign and malignant tumours of nasopharynx. This cause should always be excluded in unilateral serous otitis media in an adult.
- Disorders of tubal kinetics, particularly incompetence of the muscles opening the tube in cleft palate or palatal paralysis.
- Allergy. Seasonal or perennial allergy to inhalants or foodstuff is common in children. This not only obstructs eustachian tube by oedema but may also lead to increased secretory activity as middle ear mucosa acts as a shock organ in such cases. Allergic rhinitis reduces the immune competencies of the mucosal immune system of the upper respiratory tract and makes the middle ear more prone to infection. In addition, mucosal oedema present in allergic rhinitis, impairs the function of the ET.
- Unresolved otitis media. Inadequate antibiotic therapy in acute suppurative otitis media may inactivate infection but fail to resolve it completely. Low-grade infection lingers on. This acts as stimulus for mucosa to secrete more fluid. The number of goblet cells and mucous glands also increase. Recent increase in the incidence of this disease seems to be due to this factor.
- Viral infections. Various adeno and rhinoviruses of upper respiratory tract may invade middle ear mucosa and stimulate it to increased secretory activity.
CLINICAL FEATURES.
- Symptoms. The disease more commonly affects children below 4 years of age. The symptoms include:
- Hearing loss. OME is the leading cause of hearing loss in children and may only be the symptom. Deafness may not be appreciated by the parents and may be accidentally detected during school hearing screening or audiometric screening tests. Conductive hearing loss occurs when there is fluid in the middle ear, while sensorineural hearing loss can also occur due to passage of inflammatory mediators present in exudate into the inner ear through the round window membrane. Hearing loss rarely exceeds 35-40 dB.
- Delayed and defective speech. Prolonged middle ear effusion can lead defective speech, learning, cognitive abilities and behavioural problems.
- Mild earaches. Upper respiratory tract infections history with mild earaches.
- Feeling of pressure and fullness in the ear. Noises are heard in the ear when yawning, swallowing and sneezing.
- Otoscopic findings. Tympanic membrane is often retracted, dull and opaque with loss of light reflex. It may appear yellow, grey or bluish in colour (the so-called “blue drum”). Thin leash of blood vessels may be seen along the handle of malleus or at the periphery of tympanic membrane and differs from marked congestion of acute suppurative otitis media. Sometimes, it may appear full or with localized bulging in its posterior part due to effusion. Blackish coloured air fluid level may be seen when fluid is thin and tympanic membrane transparent. Mobility of the tympanic membrane is restricted. Often and due to the retraction of the eardrum, the handle of malleus looks shorter and horizontal with a prominent short process.

DIFFERENTIAL DIAGNOSIS.
- Hemotympanum (the dark-brown exudate behind the tympanic membrane on occasion lends this a bluish tinge)
- Chronic otitis media, evidenced by perforation, cholesteatoma flakes, and purulent exudate.
HEARING TESTS.
- Tuning fork tests show conductive hearing loss.
- Hearing loss. There is conductive hearing loss of 20– 40 dB. Sometimes, there is associated sensorineural hearing loss due to fluid pressing on the round window membrane. This disappears with evacuation of fluid.
- Impedance audiometry. It is the most useful cost-effective objective test for diagnosing OME in infants and children. Presence of fluid is indicated by reduced compliance and flat curve (type B) with a shift to negative side.
- X-ray mastoids. There is clouding of air cells due to fluid.
TREATMENT. The aim of treatment is removal of fluid and prevention of its recurrence.
- Medical
- Topical decongestants in the form of nasal drops, sprays or systemic decongestants help to relieve oedema of eustachian tube.
- Antiallergic measures. Antihistaminics or some- times steroids may be used in cases of allergy. If possible, allergen should be found and desensitization done. They are useful in cases of upper respiratory tract infections or unresolved acute suppurative otitis media.
- Middle ear aeration. Patient should repeatedly perform Valsalva manoeuvre. Sometimes, politzerization or eustachian tube catheterization has to be done. This helps to ventilate middle ear and promote drainage of fluid. Children can be given chewing gum to encourage repeated swallowing which opens the tube.
- Surgical. When fluid is thick and medical treatment alone does not help, fluid must be surgically removed.
- Surgical treatment of causative factor. Adenoidectomy, tonsillectomy and/or wash-out of maxillary antra may be required. This is usually done at the time of myringotomy. Enlarged adenoids may prevent resolution of MEE by physical obstruction of the ET orifice in the nasopharynx and serve as a reservoir for pathogens that can cause inflammation, thus disturbing ET function. This is why some otologists believe that children adenoidectomy is beneficial regardless of their size.
- Tympanotomy and cortical mastoidectomy. It is sometimes required for removal of loculated thick fluid or other associated pathology such as cholesterol granuloma.
- Incision and aspiration. It is the aspiration of fluid from the middle ear via an incision in the tympanic membrane. It is done to drain suppurative or non-suppurative effusion from the middle ear.
- Myringotomy and grommet insertion. Ventilation tube (grommet, pressure-equalizing tympanostomy tube) is also placed to provide drainage or ventilation in case of malfunctioning eustachian tube. Ventilation tubes of different materials are available. Teflon or medical-grade silicon are commonly used and are biocompatible. Titanium, gold or silver oxide-coated ventilation tubes are also used in order to inhibit biofilm formation.
Indications of Myringotomy:
- Acute suppurative otitis media – (i) Severe earache with bulging drum about to perforate, (ii) Persistent retraction of the tympanic membrane causing conductive deafness, (iii) Complications of acute otitis media, e.g. facial nerve paralysis, labyrinthitis or meningitis with the bulging tympanic membrane. (iv) Recurrent acute otitis media.
- Otitis media with effusion.
- Aero-otitis media (to drain fluid and “unlock” the eustachian tube).
- Patulous eustachian tube.
- Atelectatic ear (grommet is often inserted for long-term aeration).
- Hemotympanum

Anaesthesia of Myringotomy: General anaesthesia is routinely used in children and geriatric patients. Otherwise, myringotomy can be done under local anaesthesia or no anaesthesia at all.
Steps of operation of Myringotomy:
- First, beware of this illusion that it is the most common and simple operation.
- Clean wax and debris from the ear canal.
- Inspect for any perforations, retraction and retraction pockets, myringosclerosis, dehiscent jugular bulb and only then proceed with the operation.
- Always perform under the operating microscope.
- The preferred insertion site of the ventilation tube is anteroinferior quadrant (right ear at 5 o’clock, left ear at 7 o’clock) through a circumferential or radial incision. Insertion of the ventilation tube posterosuperiorly is not recommended because of the risk of damaging the ossicular chain. The ventilation tube is preferably placed in the anterosuperior quadrant for longer retention. Radial or circumferential incision does not influence the extrusion rate.
- The incision should cut through the entire thickness of tympanic membrane avoiding injury to ossicular chain, posterior meatal wall, jugular bulb or any other abnormal vascular anomalies (e.g. high jugular bulb, aberrant carotid artery or glomus tympanicum).
- Aspiration of middle ear fluid through the incision site before placing grommet should be avoided. It may encourage biofilm infection and tympanosclerosis (secondary to trauma and bleeding of the tympanic membrane).
Incision for Myringotomy
- Incision for drainage only – In acute infection wide circumferential incision in posteroinferior quadrant is preferred since drainage alone is the purpose. and prompt closure is desired. Circumferential incisions accumulates more epithelial debris leading to prompt closure of incision.
- Incision for grommet insertion – Radial incision in anteroinferior quadrant is preferred since it sections fewer fibres, runs parallel to most of the blood vessels irrigating the membrane and causes less scarring.
Incisions should not be made in the posterosuperior quadrant because epithelial migration is slowest in this quadrant leading to incidence of persistent perforation and can also can cause injury to incudostapedial joint and stapes. Incisions should not be made close to the umbo because of its close proximity to the promontory. Incision close to the annulus favours early extrusion of the tube.
Postoperative care of Myringotomy:
- Use of ear drops at the time of placement of grommet reduces the risk of its blockage with blood and mucus. It also reduces the chances of local infection during the early postoperative period.
- Avoid swimming and entry of water in the canal as long as grommet is in position.
- Daily cleaning of ear discharge from the canal in cases of acute suppurative otitis media. In serous otitis media, just leave a wad of cotton wool for 24–48 h.
Complications of Myringotomy include:
- The most common operative complication is the displacement of the ventilation tube into the middle ear (Attempts should be made to retrieve the tube, but failure to remove it seldom causes problems due to inert nature of grommet).
- Infection around the grommet leads to middle ear infection.
- Otorrhea may follow an acute upper respiratory tract infection.
- Granulation tissue may develop secondary to infection.
- Residual tympanic membrane perforation
- Pars tensa atrophy and retraction
- Blockage due to blood or secretions.
- Tympanosclerosis is the most common structural complication.

BIOFILM.
Bacteria forms biofilm in order to protect its cells from action of immune system of the host, antibodies and antibiotics. They secrete complex polysaccharides and form a layer which permits diffusion of nutrients into the bacterial cells and exit to bacterial excretory products. Biofilms are responsible for bacterial resistance and persistence of infection. Biofilms are implicated in chronic otitis media with effusion, chronic rhinosinusitis, and tonsil and adenoid infections. They also form on grommets, stents and catheters kept for a long time. Biofilm formation can be prevented by antibiotic-coated tubes and stents and an early removal of tubes and stents, if no longer required.
SEQUELAE OF CHRONIC SECRETORY OTITIS MEDIA.
- Atrophic tympanic membrane and atelectasis of the middle ear. In prolonged effusions, there is dissolution of fibrous layer of tympanic membrane. It becomes thin and atrophic and retracts into the middle ear.
- Ossicular necrosis. Most commonly, long process of incus gets necrosed. Sometimes, stapes superstructure also gets necrosed. This increases the conductive hearing loss to more than 50 dB.
- Tympanosclerosis. Hyalinized collagen with chalky deposits may be seen in tympanic membrane, around the ossicles or their joints, leading to their fixation.
- Retraction pockets and cholesteatoma. Thin atrophic part of pars tensa may get invaginated to form retraction pockets or cholesteatoma. Similar pockets may be seen in the attic region.
- Cholesterol granuloma. The term describe a foreign body, giant cell reaction to cholesterol crystals, and hemosiderin derived from ruptured erythrocytes. The tympanic membrane appear blue in color due to hemosiderin crystals. Cholesterol granuloma arise due to stasis of secretions in middle ear and mastoid from obstructed drainage and insufficient aeration of middle ear cleft. It causes conductive hearing loss. Treatment is mastoidectomy. Ventilation tube can be placed in early stages. A cholesterol granuloma should be differentiated from glomus tumour (causes bone erosion) and heamotympanum (history of trauma).
 ———— End of the chapter ————
———— End of the chapter ————
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hans Behrbohm, Tadeus Nawka. Textbook of Ear, Nose, and Throat Diseases with Head and Neck Surgery.
- Salah Mansour, Jacques Magnan, Karen Nicolas, Hassan Haidar. Textbook of Middle Ear Diseases Advances in Diagnosis and Management.
- Gordon B. Hughes, Myles L. Pensak, H. B. Broidy, Textbook of Clinical Otology.
- Mario Sanna, Textbook of Color Atlas of Endo-Otoscopy Examination–Diagnosis–Treatment.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
