Causes of Facial Nerve Paralysis
The cause may be central or peripheral. The peripheral lesion may involve the nerve in its intracranial, intratemporal or extratemporal parts. Peripheral lesions are more common and about two-thirds of them are of the idiopathic variety.
Table: Causes of facial nerve palsy
|
Congenital facial palsy |
Moulding of head during labour , Forceps delivery, cephalopelvic disproportion, Dystrophia myotonica, Moebius syndrome (bilateral facial nerve palsy often associated with unilateral or bilateral palsy of the abducens nerve ) |
|
Central |
Brain abscess, Pontine gliomas, Poliomyelitis, Multiple sclerosis |
|
Intracranial part |
Acoustic neuroma, Meningioma, Congenital cholesteatoma, Metastatic carcinoma, Meningitis |
|
Intratemporal part |
Idiopathic – Bell palsy, Melkersson syndrome, familial, Autoimmune syndrome, Temporal arteritis, Thrombotic thrombocytopenic purpura, Polyarteritis nodosa, Landry–Guillain–Barré syndrome (ascending paralysis), Multiple sclerosis, Myasthenia gravis, multiple sclerosis, myasthenia gravis and sarcoidosis Infections – Acute suppurative otitis media, Chronic suppurative otitis media, Herpes zoster (Ramsay Hunt syndrome), Malignant otitis externa, Chicken pox, Encephalitis Poliomyelitis (type I) Mumps, Syphilis, Tuberculosis, Lyme disease, Infectious mononucleosis (glandular fever), Leprosy, Malaria, Botulism, Mucormycosis, encephalitis, polio. Trauma – (i) Accidental: Fractures of temporal bone, Basal skull fracture. (ii) Surgical: Mastoidectomy and stapedectomy. Neoplasms – Malignancies of external and middle ear, Glomus tumour, VIIth nerve tumour, Metastasis to temporal bone (from cancer of breast, bronchus, prostate), Jugular paraganglioma, Tympanic paraganglioma, Scleroma, Meningioma, Haemangioblastoma, Neurofibromatosis II. |
|
Extracranial part |
Malignancy of parotid, Accidental injury in parotid region, Neonatal facial injury (obstetrical forceps), Facial injuries, Penetrating injury to middle ear, Altitude paralysis (barotrauma), Scuba diving (barotrauma), Lightning |
|
Iatrogenic |
Post-Immunization, Facial Or Dental Surgery Including Parotid Or Masseteric Surgery, Facelift Surgery, Tumour Resection, Resection Of Acoustic Neuromas, Embolization, Mandibular block anaesthesia |
|
Systemic |
Diabetes Mellitus, Hypothyroidism, Uraemia, Polyarteritis Nodosa, Wegener’s Granulomatosis, Sarcoidosis, Leprosy, Leukaemia, Demyelinating Disease, Pregnancy, Hypertension, Acute Porphyria |
|
Toxic |
Thalidomide Tetanus, Diphtheria, Carbon Monoxide, Ethylene Glycol, Alcohol, Arsenic, Carbon Monoxide, Misoprostol, Thalidomide, Anti-Tetanus Serum Vaccine for Rabies |
A. IDIOPATHIC
- Bell’s Palsy is an idiopathic, acute onset peripheral facial palsy. The term idiopathic palsy is reserved for cases of facial palsy that have signs and symptoms consistent with the palsy and in which a diligent search for other causes yields negative results.
Minimum diagnostic criteria for labelling bell’s palsy.
- Paralysis or paresis of all muscle groups on one side of the face
- Sudden onset
- Absence of signs of central nervous system disease
- Absence of signs of ear or CPA disease
Incidence.
- 60 %- 75 % of facial palsy is Bell’s type
- Any age group may be affected though incidence rises with increasing age. A positive family history is present in 6–8% of patients.
- Recurrence is seen in 7 to 12% of patients; however, recurrence should heighten suspicion for another aetiology, such as a tumour involving the facial nerve.
- Risk of Bell’s palsy is high in diabetic patients (with microvascular angiopathy) and in pregnant women in 3rd trimester (retention of fluid leading to oedema or compression within Fallopian canal).
- Bell’s palsy is recurrent in 4.5–15% of patients
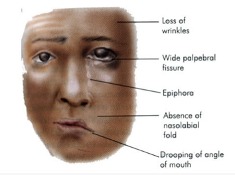
Diagram showing Facial paralysis of left side
Aetiology
- Viral Infection. Although frequently called idiopathic facial paralysis, a viral aetiology is the most likely cause; numerous studies have identified herpes simplex virus type 1 (HSV-1), herpes sim- plex virus type 2 (HSV-2), varicella zoster virus (VZV), human herpesvirus, influenza B, adenovirus, Coxsackie virus and Epstein–Barr virus (EBV) as the causative agents.
- Vascular Ischaemia. Primary ischaemia is induced by cold or emotional stress. Secondary ischaemia is an extension of primary ischaemia in which fluid exudation, oedema leads to compression of microcirculation of the nerve.
- Hereditary. There may also be an inherited tendency toward developing Bell’s palsy.
- Autoimmune Disorder: Changes in T-lymphocyte have been observed in cases of facial palsy.
Sign and symptoms. Abrupt in onset, and patient may notice the asymmetry when wake up in the morning or while drinking or eating.
- Patient is unable to open or close his eye on the affected side. If he attempts to close his eye, eyeball turns up and out (Bell’s phenomenon).
- Facial asymmetry.
- Epiphora.
- Drooling of saliva from the angle of mouth.
- Pain in the ear (otalgia) may precede or accompany the nerve paralysis.
- Some complain of noise intolerance (stapedial paralysis) or loss of taste (involvement of chorda tympani).
Diagnosis. It is usually clinical.
- Rule out all other known causes of peripheral facial paralysis.
- Nerve excitability tests. Can bedaily or on alternate days to monitor nerve degeneration.
- Topodiagnosis tests. To know the cause and the site of lesion.
Treatment.
(i) General management
- Reassurance and psychological support.
- Relief of earache by analgesics.
- Eye care. Protection of the eye is the most urgent consideration in facial palsy. Due to incomplete closure of eye, tear film from the cornea evaporates causing dryness, exposure keratitis and corneal ulcer.
- Frequent use of eye drops (containing hydroxypropyl cellulose, hydroxypropyl methylcellulose or polyvinyl) frequently during the daytime, whilst at night, eye should be taped closed after putting thicker ointments containing petroleum, mineral oil or lanolin.
- Corneal protection with lubrication and patching.
- Use of large-lens sunglasses.
- Patients having long-term facial nerve palsy are advised to close their eye manually using a finger as well as attempting to stretch the upper lid in order to prevent shortening caused by unopposed action of levator palpebrae superioris muscle.
- Temporary tarsorrhaphy may also be indicated. Eye closure can also be improved by using gold-weight implant sutured to the tarsal plate deep to levator palpebrae muscle.
- Physiotherapy or massage of the facial muscles is encouraged.
(ii) Medical management
Steroids. Prednisolone is the drug of choice. If patient reports within 1 week, the adult dose of prednisolone is 1 mg/kg/day divided into morning and evening doses for 5 days. The patient is called for follow-up on the fifth day. If paralysis is incomplete or is recovering, dose is tapered during the next 5 days. If paralysis remains complete, the same dose is continued for another 10 days and thereafter tapered in next 5 days (total of 20 days). Steroids can be combined with acyclovir for Herpes zoster oticus or Bell’s palsy. The usual recommended oral regime is prednisone 1mg/kg/day for 10 days and oral acyclovir (400mg five times daily) for 10 days or valacyclovir (500 mg, three times a day). Contraindications to use of steroids include pregnancy, diabetes, hypertension, peptic ulcer, pulmonary tuberculosis and glaucoma. Steroids have been found useful to prevent incidence of synkinesis, crocodile tears and to shorten the recovery time of facial paralysis.
(iii) Surgical Treatment. Facial nerve decompression of vertical and tympanic segments or whole of the fallopian canal. It improves the micro-circulation and relieve pressure of the nerve. Prognosis. The degree of facial nerve damage determines the extent of recovery. Normal facial function is usually recovered in 1-3 months in 2/3rd of patients.80- 90% of the patients recover fully. 10-15% may show residual muscle weakness due to nerve degeneration. Better prognosis is seen in incomplete Bell’s palsy and in those patients who start recovering within 3 weeks of onset. Recurrent facial palsy may not recover fully. Poor prognosis is seen if paralysis is complete at onset, age >60 years and in patients with absent stapedius reflex, postauricular pain, dry eye, abolished taste sensation.
2. Melkersson-Rosenthal Syndrome
It is also an idiopathic rare neurological disorder. Predominately in the second decade of life. It is characterised by a triad of relapsing and increasingly severe facial paralysis, swelling of lips ( cheilitis) and fissuring of the tongue.
Causes : Genetic factors, dietary factors/ allergens, associated with Crohn’s disease.
B. INFECTIONS
1. Otitis media. Facial nerve paralysis can occur as a complication in both acute and chronic otitis media.
- Acute otitis media. Inflammation of middle ear may cause direct infection through bony canal dehiscence. It is treated by systemic antibiotics.
- Chronic otitis media. Cholesteatoma or granulation tissue erode the bony canal by osteitis and inflammatory oedema leading to compression of the facial nerve. Treatment is urgent exploration of the middle ear and mastoid.
2. Malignant otitis externa (Necrotizing otitis externa).
It is an severely progressive necrotizing Pseudomonas infection of the ear canal. Infection may rapidly spread to entire temporal bone and jugular foramen causing involvement cranial nerves (IX, X, XI, and XII) and may lead to skull base osteomyelitis. It is usually seen in immunocompromised patients, particularly the elderly diabetics, and in patients on long steroid therapy or chemotherapy. Facial paralysis is commonly seen. In an elderly diabetic patient with severe otalgia and granulation tissue in the external ear canal at its cartilaginous–bony junction is a cardinal sign of skull base osteomyelitis and should not be underestimated.

Spread.
- Anteriorly, infection may spread to the skull base at the most vulnerable portion of the external canal, the osseocartilaginous junction, and proceed to infiltrate the parotid gland and facial nerve by way of the fissures of Santorini.
- Inferiorly, traversing the tympanomastoid suture and fissures of Santorini provides access to the infratemporal fossa and jugular foramen, placing cranial nerves IX, X, and XI at risk for injury. Proximal injury results from involvement of the main trunk at the stylomastoid foramen via direct extension from the external auditory canal.
- Medially, infection may spread to the marrow spaces of the skull and eventually the petrous apex, placing cranial nerves V and VI at risk.
- Posteriorly, by direct extension into the pneumatized spaces of the mastoid, where the vertical segment is at risk.
Pathogenesis. Normally, cerumen provides protective function in controlling the pH that prevents maceration and excessive bacterial colonization. It is proposed that these protective features of cerumen are absent among patients with diabetes, permitting bacterial overgrowth and increased susceptibility to tissue invasion. Diabetic microangiopathy results in ischemic, nutritionally deficient, devitalized tissue. The infective process produces exotoxins and enzymes like elastase which digests vessel wall. Impaired local and systemic immune systems lack the ability to control local infection, permitting progression of uncomplicated otitis externa to a fulminate, systemic invasive infection.
Symptoms.
- Penetrating excruciating earache which is continuous and severe in nature and commonly out of proportion to the clinical examination findings.
- Persistent ear discharge not relieving on multiple courses of medications. Discharge is initially mucopurulent and later becomes foul smelling purulent and blood tinged.
- Both CHL and SNHL can occur
- Facial paralysis.
- Headache
- Vertigo
Signs.
- Granulation tissue seen protruding into the EAC from the bony-cartilaginous junction
- Sagging of posterior meatal wall.
- Tympanic membrane. May be normal.
- Pinna. Tenderness is present and doughy on palpation.
- Mastoid tenderness
- Multiple cranial nerves (IX, X, XI, XII) involvement is seen in late stages.
Investigations.
- Culture sensitivity by ear swab.
- CT scans help to evaluate the extent of bony involvement but MRI provides more details regarding soft-tissue disease and can also evaluate the patency of the dural sinuses if combined with magnetic resonance angiography,
- Gallium-67 bone scan helps in confirming the diagnosis and follow-up of the patient. It is taken up by monocytes and reticuloendothelial cells, and is indicative of soft tissue infection. It can be repeated every 3 weeks to monitor the disease and response to treatment.
Differential diagnosis
- Diffuse otitis externa. There is absence of excruciating pain and presence of granulations in the ear canal.
Treatment.
Long-term administration of parental antibiotics, in combination with daily extensive debridement of necrotic and granulation tissue and vigilant management of diabetes and other compromising medical conditions. Surgical management is currently not indicated, diagnostic biopsies can be done to rule out malignancy. Anti-pseudomonas antibiotics should be given for minimum 2-3 months. Antibiotics found effective are:
- Gentamicin combined with ticarcillin.
- Third-generation cephalosporins. e.g. ceftriaxone 1–2 g/day i.v. or ceftazidime 1–2 g/day i.v. are usually combined with an aminoglycoside.
- Quinolones (ciprofloxacin, ofloxacin and levofloxacin) are also effective and can be given orally. They can be combined with rifampin.
- Ciprofloxacin (750mg orally twice per day) seems to be the antibiotic of choice for maintainence and prolonged treatment for a minimum of 3 months to 1 year may be required, to avoid relapse.
- In case there is resistance to ciprofloxacin, antipseudomonal β-lactam agents (ceftazidime, piperacillin, imipenem) with or without combination of aminoglycoside can also be used. Aspergillus infection if found need systemic antifungal treatment.
3. Herpes Zoster oticus (Ramsay–Hunt Syndrome)
It is an acute peripheral facial neuropathy associated with a typical erythematous vesicular rash of the skin of the ear canal, auricle or mucous membrane of oropharynx. It is caused by the reactivation of Varicella Zoster virus (VZV) in the geniculate ganglion of the patient who had chickenpox earlier during his/ her lifetime. It results in facial nerve paralysis. The syndrome is more common in old age>60 years and is extremely rare in children less than 6 years. Patients should avoid contact with newborns, pregnant women, immunocompromised patients as VZV can be found in the blisters and tears of patients of ramsay hunt syndrome, at least until all the blisters change to scabs.

Vesicles, red rash and blisters on pinna. Ramsay Hunt Syndrome
Clinical features.
- Vesicles, red rash and blisters in or around the EAC on affected side facial nerve palsy. It can also be on the ipsilateral neck, face, roof of the mouth, lips, or dorsal tongue.
- Excruciating (severe) otalgia
- Loss of taste perception in the anterior two-thirds of the tongue, dry mouth and eyes.
- Anaesthesia of face, giddiness and hearing impairment due to involvement of Vth and VIIIth nerves.
- Tinnitus, vertigo and a sensorineural hearing loss
Complications.
- Post herpetic neuralgia
- Eye damage (blurred vision) may occur
- Hearing loss & facial weakness may be permanent
Prognosis. The prognosis for Ramsay Hunt is worse than idiopathic facial palsy. Persistent weakness is observed in 30–50% of patients and only 10% recover completely after complete loss of function without treatment.
Prevention. Children are vaccinated against chickenpox, reduces their chances of getting infection
Treatment
- The recommended regime is prednisone 1mg/kg/day for 5 days then tapered for 10 days, and intravenous acyclovir (250 mg three times daily). The combination of steroids and acyclovir also seems to reduce otalgia, vertigo and post-herpetic neuralgia.
- Painkillers(opioids)
- Oral acyclovir 800mg 5 times a day for 7-10 day.
- Surgical decompression of the facial nerve has no role.
4. Guillain–Barré syndrome (acute inflammatory demyelinating polyradiculoneuropathy) is a rare autoimmune disorder. The most prominent feature is ascending symmetrical muscular weakness that is typically seen 2–3 weeks after an upper respiratory infection. Facial nerve paralysis may develop and is often bilateral.. The intravenous immunoglobulin infusion is the most effective treatment.Steroids have been shown to have no beneficial effect and may even delay recovery. Treatment also involves respiratory support and passive physiotherapy
5. Epstein–Barr infection (infectious mononucleosis) is clinically characterized by generalized lymphadenopathy, fever and sore throat and may be associated with facial nerve palsy. The presence of at least 10% of atypical lymphocytes on peripheral tests and positive serology will confirm the diagnosis. Forty percent of the EBV-associated facial nerve palsy cases are bilateral.
C. TRAUMATIC FACIAL PARALYSIS
1. Fractures of Temporal Bone
Temporal bone is very thick and hard structure located in the base of the skull. Skull base has multiple foramina, increasing susceptiblity to traumatic injury. Temporal bone contains important structures like facial nerve, labyrinth, CN VIII, ossicles, carotid artery, jugular vein etc. Any or all structures can get involve in fractures of temporal bone.
Aetiology.
- Motor vehicle accident
- Fall from height
- Physical assaults
- Gunshot wound
- Any trauma causing head, maxillofacial and spine injuries.
Types of fractures.
Its depends on the direction of fracture with respect to the long axis of petrous temporal bone
- Longitudinal. Runs parallel to long axis of petrous temporal bone. Starts at squamous part of temporal bone to end at foramen lacerum
- Transverse. Runs perpendicular to the petrous temporal bone. Starts at foramen magnum or jugular foramen towards the foramen spinosum
- Mixed (oblique). Having one or more features of both above fractures.
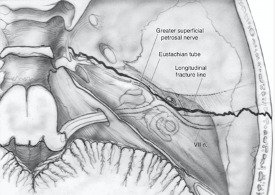
A longitudinal fracture runs along the axis of petrous pyramid. Typically, it starts at the squamous part of temporal bone, runs through the roof of the external ear canal and middle ear towards the petrous apex and to the foramen lacerum.
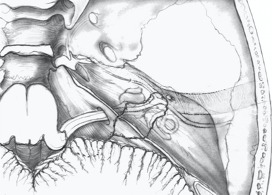
Transverse fracture. It runs across the axis of petrous. Typically, it begins at the foramen magnum, passes through occipital bone, jugular fossa and petrous pyramid, ending in the middle cranial fossa. It may pass medial, lateral or through the labyrinth.
Further complications that should be considered are CSF leak, meningitis, meningocoele from tegmen involvement, and vascular injury to the carotid canal or jugular fossa. Delayed complications can include labyrinthine ossificans and post-traumatic cholesteatoma.
Cause of facial nerve paralysis
- Oedema.
- Stretching
- Intraneural hemorrhage.
- Compression by a bony spicule.
- Dehiscence of nerve.
- Transection of nerve.
Investigations.
High-definition CT
- Type and direction of fracture
- Involvement of otic capsule
- Any associated complications.
Treatment of facial nerve paralysis
It depends upon time of onset of facial palsy following injury.
- Delayed onset paralysis. Treatment is same as Bell palsy and palsy almost always recovers.
- Immediate onset paralysis. Require urgent exploration.
- Facial nerve decompression
- Re-Anastomosis Of Cut Ends
- Cable Nerve Graft.
Table: Differences In Longitudinal and Transverse Fractures of Temporal Bones
| Longitudinal | Transverse | |
| Incidence | Seen in 80% cases | Seen in 20% cases, but more common in children |
| Type of injury | Parietal blow, lateral blow over mastoid region | Occipital or frontal blow |
| Fracture line | Runs parallel to long axis of petrous temporal bone.Starts at squamous part of temporal bone toend at foramen lacerum | Runs perpendicular to the petrous temporal bone. Starts from foramen magum or jugular foramen towards the foramen spinosum |
| Injury to external and middle ear | present | Absent |
| Bleeding from ear | Common, due to injury to tegmen andtympanic membrane | Absent because tympanic membrane is intact. |
| Haemotympanum | Absent | Haemotympanum may be seen |
| Cerebrospinal fluid otorrhoea | Present, often mixed with blood and usually it is temporary. | Absent or unmanifested |
| Structures injured | Tympanic membrane , ossicles and tegmen | Labyrinth or CN VIII |
| Type of Hearing loss | Conductive, SNHL can also occur due to concussion but is not common. | Sensorineural |
| Vertigo | Less often; due to concussion | Severe, due to injury to labyrinth or CN VIII |
| Incidence of Facial paralysis | Seen in 20% cases, delayed onset. | Seen in 50% cases. Immediate onset. |
| Site of injury | Nerve is injured in tympanic segment, distal to geniculate ganglion | Injury to nerve in meatal or labyrinthine segment proximal to geniculate ganglion. |
| Skull base foramen | Ovale | Spinosum, lacerum |
D. IATROGENIC INJURY
- Ear or Mastoid Surgery
Facial nerve can get injured during middle ear or mastoid surgery. The most common site of injury during middle ear or mastoid surgery is the distal tympanic segment including the second genu, followed by the mastoid segment. The incidence of facial nerve palsy has been reported to be between 0.6% and 3.6%.
Treatment.
- Facial nerve injury recognized during surgery, exploration with decompression of proximal and distal segments of the nerve should be undertaken.
- Facial palsy in seen immediately after surgery and if the nerve was identified or was not at risk during the operation, a few hours of observation will usually allow for any local anaesthetic-induced weakness to clear. The possibility of a tight mastoid dressing over an exposed nerve should also be considered and it is wise to remove the pack. If the paralysis is incomplete, the patient should be started on oral steroids and observed clinically. In cases of progression to full paralysis, exploration should be considered.
- In rare cases, a delayed palsy is observed a few days after uneventful middle ear surgery. The aetiology is unclear, although reactivation of HSV or VZV is postulated as the underlying mechanism. Combined use of prednisone and acyclovir should be considered and the overall prognosis appears to be good.
Operative injuries to facial nerve can be avoided if attention is paid to the following:
- Knowledge of the course of facial nerve.
- Identification of surgical landmarks of the facial nerve.
- Chances of variations and anomalies of the facial nerve.
- Always work along the course of nerve and never across it.
- Use diamond burr while working close to nerve.
- Ensure constant irrigation while drilling in order to avoid thermal injury.
- Gently handle the nerve if it is exposed. Avoid any pressure of instruments on the nerve.
- Granulation tissue penetrating the nerve should not be removed.
- Always work using operating microscope under magnification
- Use intraoperative facial nerve monitor if available.
2. Parotid Surgery
Facial nerve can get injured in parotid surgery or sometimes it is deliberately excised in malignant tumours. Use of facial nerve monitor during parotid surgery helps in avoiding injury to facial nerve and at the end of the surgery the main trunk should be stimulated to confirm continuity.
3. Facial Nerve trauma
Surgical exploration and repair is advisable within 3 days if the patient is both medically and neurologically stable. Nerve stimulator is used to identify the distal segments of facial nerve branches.
4. Gunshot injuries
Facial nerve injury is seen in about 50%, and vertical segment being the mostcommonly affected.
Treatment. Urgent surgical exploration is required, as delay makes the nerve difficult to identify due to formation of granulation tissue. Reanimation surgeries like interval cable grafting is done if a segment of the nerve has been destroyed. Open mastoidectomy with a meatoplasty (to remove fragments of skin and bullet) should be done as there is a high risk of infection due to bony damage and subsequent cholesteatoma formation.
E. NEOPLASMS
1. Intratemporal Neoplasms
- Facial nerve schwannomas. It is a benign, slow growing tumour which occurs anywhere along the course of the facial nerve from the cerebellopontine angle to the branching of nerve in the parotid gland.It arises from Schwann cells within the nerve sheath.The presenting symptoms can be progressive or sudden onset or recurrent facial weakness and usually depends on the segment involved.MRI with gadolinium is mainstay for diagnosis and will show an enhancing (usually fusiform) lesion at the site of involvement.Management options are:
- Observation with serial scanning.
- Radiotherapy (stereotactic or fractionated).
- Surgery. Excision and nerve grafting and is usually reserved for tumours that have failed radiation treatment.
- Almost all intratemporal Neoplasms results in facial paralysis.
2. Tumours of Parotid
Facial paralysis is seen parotid gland tumours. Presence of facial palsy is mostly seen malignant tumours.
F. SYSTEMIC DISEASES AND FACIAL PARALYSIS
Sometimes peripheral facial paralysis is seen systemic diseases. Exclude Diabetes Mellitus, Hypothyroidism, Uraemia, Polyarteritis Nodosa, Wegener’s Granulomatosis, Sarcoidosis, Leprosy, Leukaemia, Demyelinating Disease, Pregnancy, Hypertension Acute Porphyria.
G. CONGENITAL FACIAL PALSY is clinically defined as facial palsy of 7thcranial nerve present at birth and shortly thereafter. It results because of relatively superficial position of the extracranial facial nerve in infants. Congenital Facial palsy of developmental origin is associated with anomalies of pinna and EAC such as microtia and atresia. Acquired causes of facial palsy include perinatal trauma, intrapartum compression
H. BILATERAL CONCURRENT FACIAL PARALYSIS. It is associated with Guillain-Barré syndrome, sarcoidosis, sickle cell disease, acute leukaemia, bulbar palsy, leprosy, cerebral lymphoma, Lyme disease, rabies, infectious mononucleosis and Moebius syndrome.
I. RECURRENT FACIAL PALSY RECURRENT FACIAL PALSY is seen in Bell palsy (3–10% cases), Melkersson syndrome, diabetes, sarcoidosis and tumours. Recurrent palsy on the same side may be caused by a tumour in 30% of cases. In contrast to recurrent ipsilateral facial paralysis, contralateral recurrence is almost always benign.
J. INFLAMMATORY DISORDERS OF FACIAL NERVE.
- Sarcoidosis is an autoimmune systemic disease. It is characterized by non-caseating granulomata formation in the lungs and occurs in 3rd–4thdecade of life. Facial nerve palsy which can develop alone or with uveitis and parotitis as a part of Heerfordt’s disease (Triad of uveoparotid fever). Palsy is often bilateral, sudden and resolve spontaneously. Elevated angiotensin converting enzyme titre and hypercalcemia helps to confirm the diagnosis. Treatment. Systemic corticosteroids.
- Lyme disease. It is a vector-borne (spirochete Borrelia burgdorferi), multisystem inflammatory disease involving skin, nervous system, heart and joints. Transmitted to humans by the bite of ticks. Clinical features are acute facial nerve palsy, which is usually unilateral but can be bilateral especially in children, recovers within few weeks to months. Flu-like symptoms. Erythema migrans. Treatment. Doxycycline or amoxicillin for 14–21 days in patients having facial nerve palsy. Doxycycline is contraindicated in patients below 8 years and in pregnant women.
——————– End of the chapter ——————–
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Susan Standring, Gray’s Anatomy.
- Ganong’s Review of Medical Physiology.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
