Types of Hearing Loss: Hearing loss is defined as an impairment of hearing. The severity of hearing loss/impairment hearing may vary from mild to moderate or profound. Deafness means little or no hearing at all.
Classification of Hearing Loss
Table – WHO grading of degree of hearing loss. WHO in 1980, recommended grading on the basis of pure tone audiogram taking the average of the hearing threshold in frequencies – 500, 1000 and 2000 Hertz in the better ear.
| Degree of hearing loss | Hearing threshold in better ear (average of 500, 1000 and 2000 Hz) |
| Not significant | 0-25 dB |
| Mild | 26-30 dB |
| Moderate | 41-55 dB |
| Moderate severe | 56-70 dB |
| Severe | 71-91 dB |
| Profound | Above 91 dB |
| Total |
Hearing loss can be of any of these types –
- Conductive hearing loss
- Sensorineural hearing loss
- Mixed hearing loss
- Non-organic/ Functional hearing loss
- Central hearing loss
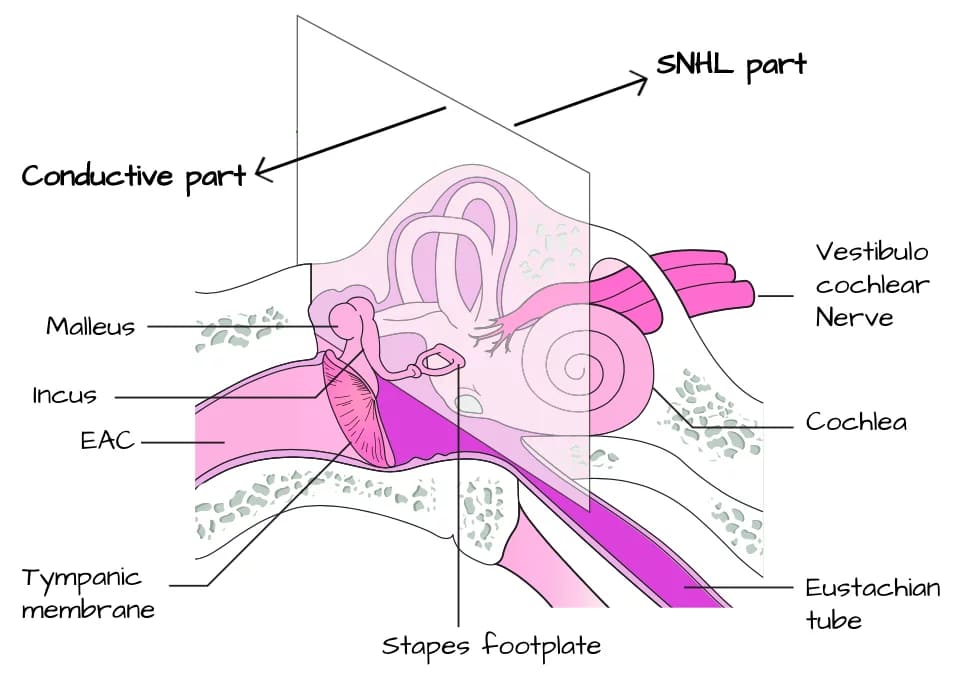
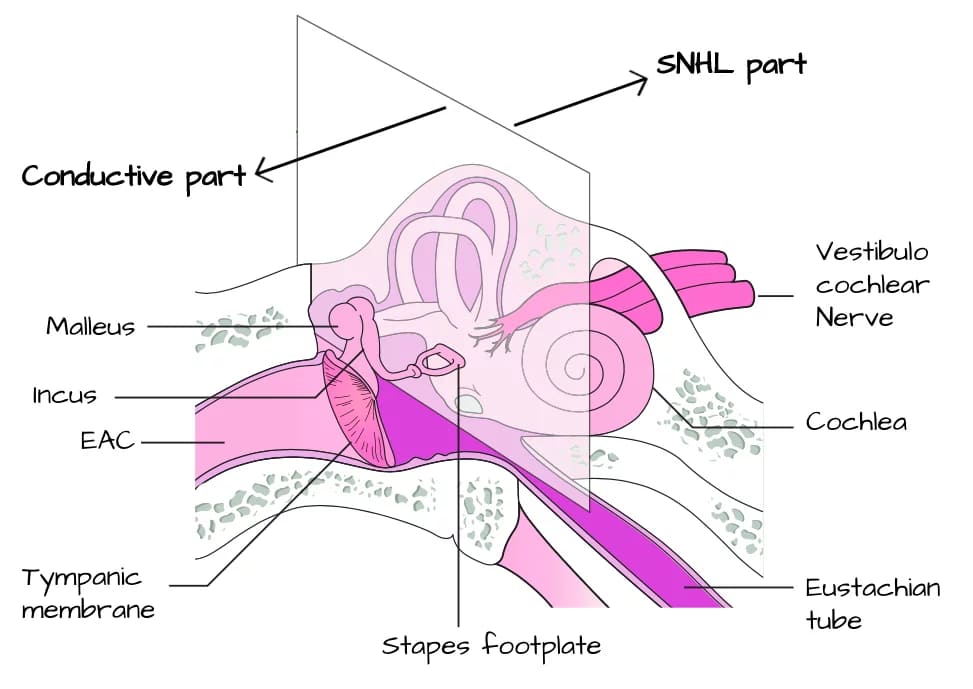
- Conductive Hearing Loss. It is caused by an obstruction in the passage of sound waves at any point from external ear till cochlea (stapediovestibular joint). Thus, the cause may lie in the external ear (obstructions), tympanic membrane (perforation), middle ear (fluid), ossicles (fixation or disruption) or the eustachian tube (obstruction).
- Sensorineural Hearing Loss. It results from lesions of the cochlea (sensory type) or VIIIth nerve and its central connections (neural type). The term retrocochlear is used when hearing loss is due to lesions of the VIIIth nerve, and central deafness is used when it is due to lesions of central auditory connections.
- Mixed Hearing Loss. In this type, elements of both conductive and sensorineural deafness are present in the same ear. There is an air-bone gap indicating conductive loss and also there is impairment of bone conduction indicating a sensorineural loss. Mixed hearing loss is seen in some cases of otosclerosis and chronic suppurative otitis media.
- Functional Hearing Loss. Functional hearing loss is the exaggeration or feigning of hearing impairment. Many terms have been used to describe this type of hearing “impairment,” including nonorganic hearing loss, pseudo-hyperacusis, malingering, factitious hearing loss, and so on. In many cases of functional hearing loss, particularly in adults, an organic hearing sensitivity loss exists but is willfully exaggerated. In other cases, often secondary to trauma, the entire hearing loss will be willfully feigned. Because there may be some organicity to the hearing loss, it is probably best considered as an exaggerated hearing loss or a functional overlay to an organic loss.
- Central Hearing loss. The patients with the central auditory pathology have difficulty in hearing a distorted, unclear speech and also when there is some background noise like in a party. They have normal pure-tone hearing thresholds and other hearing tests but cannot follow instructions. These problems are due to poor processing of the auditory cues in the higher auditory pathways.
Assessment of Hearing loss: While assessing the auditory function it is important to find out
- Type of hearing loss (conductive, sensorineural or mixed).
- Degree of hearing loss (mild, moderate, moderately severe, severe, profound or total).
- Site of the lesion. In conductive, the lesion may be at the external ear, tympanic membrane, middle ear, ossicles or eustachian tube. Clinical examination and tympanometry can be helpful to find the site of such lesions. In sensorineural, find out whether the lesion is cochlear, retrocochlear or central. Special tests of hearing will be required to differentiate these types.
- Cause of hearing loss. The cause may be a congenital, traumatic, infective, neoplastic, degenerative, metabolic, ototoxic, vascular or autoimmune process. A detailed history and laboratory investigations are required.
A. CONDUCTIVE HEARING LOSS
There is obstruction of the passage of sound waves at any point from external ear till cochlea (stapediovestibular joint) causing conductive hearing loss.
The characteristics of conductive hearing loss are:
- Negative Rinne test, i.e. BC > AC.
- Weber lateralized to poorer ear.
- Normal absolute bone conduction.
- Low frequencies affected more.
- Loss is not more than 60 dB.
- Speech discrimination is good, best for hearing aid amplification.
- Hearing loss is partial and never complete because bone conduction is intact.
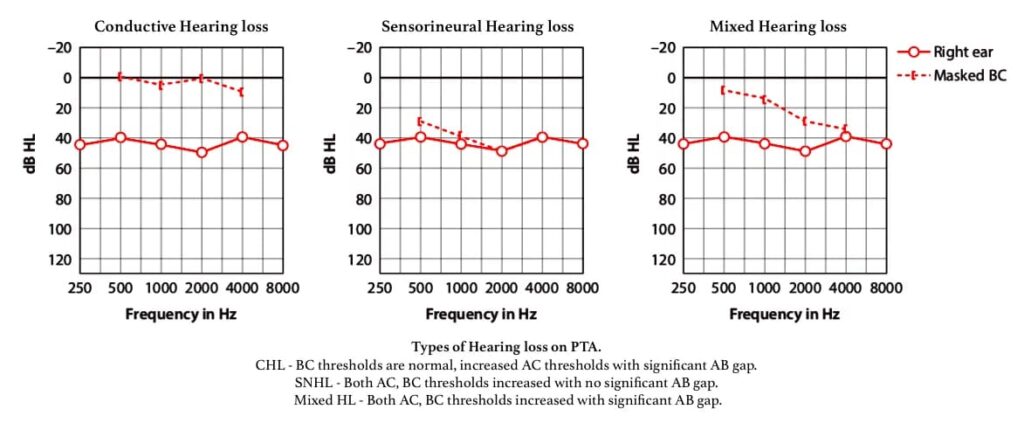
The characteristics of conductive hearing loss on PTA:
- Difference of more than 10dB between AC and BC thresholds at any frequency.
- BC thresholds are generally at normal hearing levels (equal or better than 20dBHL) in cases of conductive hearing loss.
- BC thresholds are raised above 20 dB HL and there is a significant ABG, this is referred to as a ‘mixed’ hearing loss.
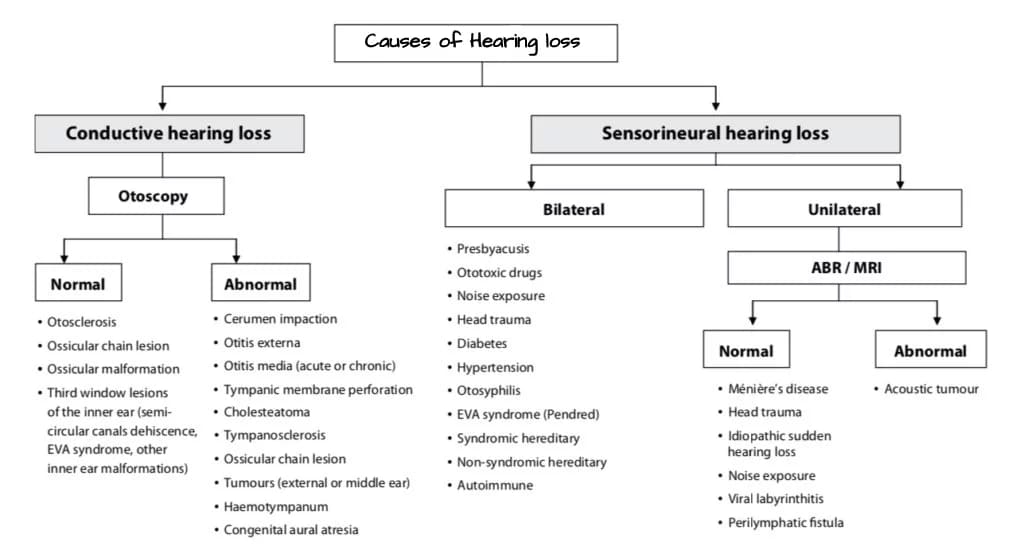
Causes of conductive hearing loss:
| Congenital causes | Acquired causes |
– Meatal atresia – Fixation of stapes footplate (Most common) – Fixation of malleus head – Ossicular discontinuity – Congenital cholesteatoma – Aplasia of the oval or round window |
External ear: Any obstruction in the ear canal, e.g. wax, stenosis, benign or malignant tumour, foreign body, furuncle. Middle ear: – Tympanic membrane perforation – Fluid in the middle ear (acute otitis media, serous otitis media or haemotympanum). – Ear ossicles, e.g. disruption, erosion and fixation of ear ossicles (otosclerosis, trauma). – Eustachian tube obstruction as in retracted tympanic membrane. |
Management of conductive hearing loss:
- Removal of canal obstructions, e.g. impacted wax, foreign body, osteoma or exostosis, keratotic mass, benign or malignant tumours, or meatal atresia.
- Hearing aid. Is used in cases, where surgery is not possible, refused or has failed.
- Surgery for conductive hearing loss – (i) Myringotomy with or without grommet insertion for removal of middle ear fluid, (ii) Tympanoplasty. (iii) Myringoplasty, (iv) Ossiculoplasty.
Surgical Options:
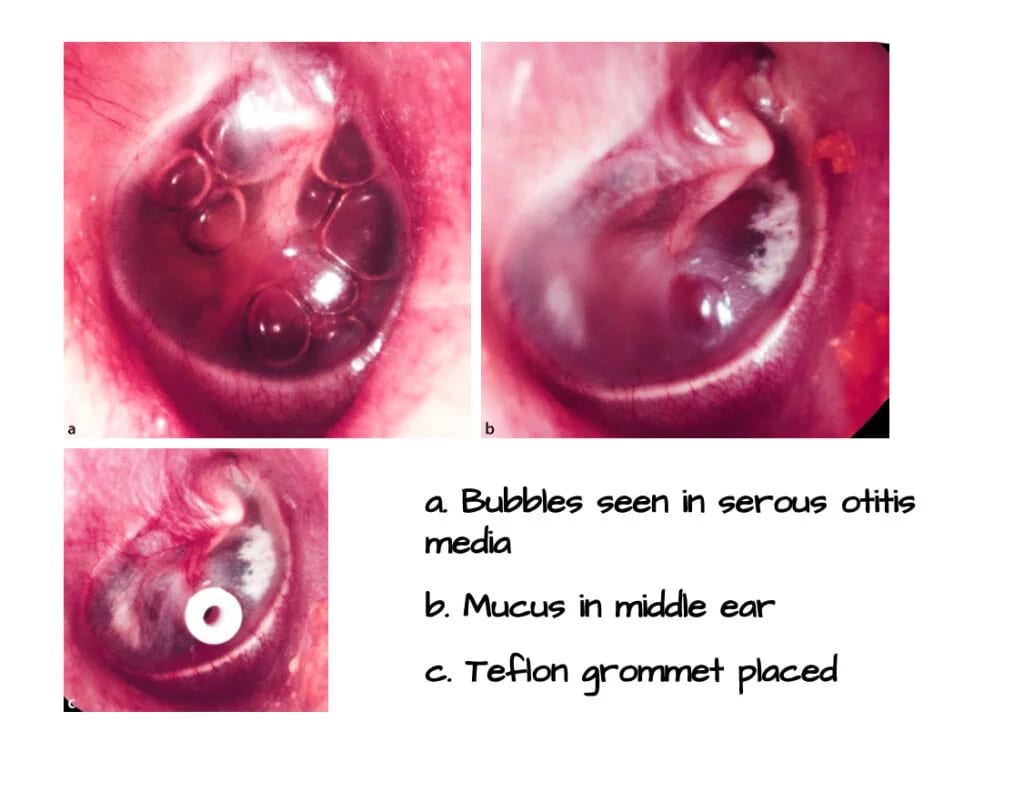
(i) Myringotomy.
It is the aspiration of fluid from the middle ear via an incision in the tympanic membrane. It is done to drain suppurative or non-suppurative effusion from the middle ear. Ventilation tube (grommet, pressure-equalizing tympanostomy tube) is also placed to provide drainage or ventilation in case of malfunctioning eustachian tube.
Ventilation tubes of different materials are available. Teflon or medical-grade silicon are commonly used and are biocompatible. Titanium, gold or silver oxide-coated ventilation tubes are also used in order to inhibit biofilm formation.
Indications of Myringotomy:
- Acute suppurative otitis media – (i) Severe earache with bulging drum about to perforate, (ii) Persistent retraction of the tympanic membrane causing conductive deafness, (iii) Complications of acute otitis media, e.g. facial nerve paralysis, labyrinthitis or meningitis with the bulging tympanic membrane. (iv) Recurrent acute otitis media.
- Otitis media with effusion.
- Aero-otitis media (to drain fluid and “unlock” the eustachian tube).
- Patulous eustachian tube.
- Atelectatic ear (grommet is often inserted for long-term aeration).
- Hemotympanum
Anaesthesia of Myringotomy: General anaesthesia is routinely used in children and geriatric patients. Otherwise, myringotomy can be done under local anaesthesia or no anaesthesia at all.
Steps of operation of Myringotomy:
- First, beware of this illusion that it is the most common and simple operation.
- Clean wax and debris from the ear canal.
- Always perform under the operating microscope.
- The preferred insertion site of the ventilation tube is anteroinferior quadrant (right ear at 5 o’clock, left ear at 7 o’clock) through a circumferential or radial incision. Insertion of the ventilation tube posterosuperiorly is not recommended because of the risk of damaging the ossicular chain. The ventilation tube is preferably placed in the anterosuperior quadrant for longer retention. Radial or circumferential incision does not influence the extrusion rate.
- The incision should cut through the entire thickness of tympanic membrane avoiding injury to ossicular chain, posterior meatal wall, jugular bulb or any other abnormal vascular anomalies (e.g. high jugular bulb, aberrant carotid artery or glomus tympanicum).
- Aspiration of middle ear fluid through the incision site before placing grommet should be avoided. It may encourage biofilm infection and tympanosclerosis (secondary to trauma and bleeding of the tympanic membrane).
Postoperative care of Myringotomy:
- Use of ear drops at the time of placement of grommet reduces the risk of its blockage with blood and mucus. It also reduces the chances of local infection during the early postoperative period.
- Avoid swimming and entry of water in the canal as long as grommet is in position.
- Daily cleaning of ear discharge from the canal in cases of acute suppurative otitis media. In serous otitis media, just leave a wad of cotton wool for 24–48 h.
Complications of Myringotomy include:
- The most common operative complication is the displacement of the ventilation tube into the middle ear (Attempts should be made to retrieve the tube, but failure to remove it seldom causes problems due to inert nature of grommet).
- Infection around the grommet leads to middle ear infection.
- Otorrhea may follow an acute upper respiratory tract infection.
- Granulation tissue may develop secondary to infection.
- Residual tympanic membrane perforation
- Pars tensa atrophy and retraction
- Blockage due to blood or secretions.
- Tympanosclerosis is the most common structural complication.
(ii) Tympanoplasty
It is an operation to (i) eradicate the disease from the middle ear and (ii) to reconstruct the hearing mechanism with or without mastoid surgery, with or without tympanic membrane grafting. When the operation is limited to repair of tympanic membrane it is known as myringoplasty. When the operation is limited to the reconstruction of the ossicular chain it is known as ossiculoplasty. When the operation involves both procedures it is known as tympanoplasty. This procedure can be combined with either an intact canal wall (ICW) or a canal-wall-down (CWD) mastoidectomy to eradicate the disease from the mastoid area.
Effects of tympanic membrane perforation on hearing.
- It removes transformer mechanism (larger the size of perforation, lesser the transformer ratio). Total perforation results in a loss of 40 to 45 dB.
- It removes sound protection from the round window (sound to reach both oval and round windows at the same time, thus cancelling the resultant movements of the perilymph).
Interrupted ossicular chain does not have much effect on the hearing in cases of large perforation. But interrupted ossicular chain behind an intact tympanic membrane results in maximum conductive hearing loss of 60 dB. It is because the vibrations of the ossicular chain are not reaching the oval window and secondly both oval and round windows are protected from sound due to intact tympanic membrane.
The Aim of tympanoplasty is to restore and achieve:
- Dry ear and hearing improvement by the closure of any tympanic membrane perforation by grafting and/ or ossicular reconstruction.
- Sound-pressure transformation mechanism for the oval window by giving an intact tympanic membrane and connecting it with stapes footplate either via an intact or a reconstructed intact ossicular chain.
- Sound protection (acoustic separation between two windows) for the round window by constructing a closed and air-containing middle ear.
Indications: Tympanic membrane perforations and associated hearing loss, with or without middle ear pathology such as tympanosclerosis.
Contraindications
- ASOM
- Actively discharging ear
- Otitis externa
- Complicated CSOM
- Uncontrolled cholesteatoma
- Only hearing ear
- Eustachian tube blocked
- Malignant tumours of the outer/middle ear
- Unusual infections such as malignant otitis externa
- Poor general health
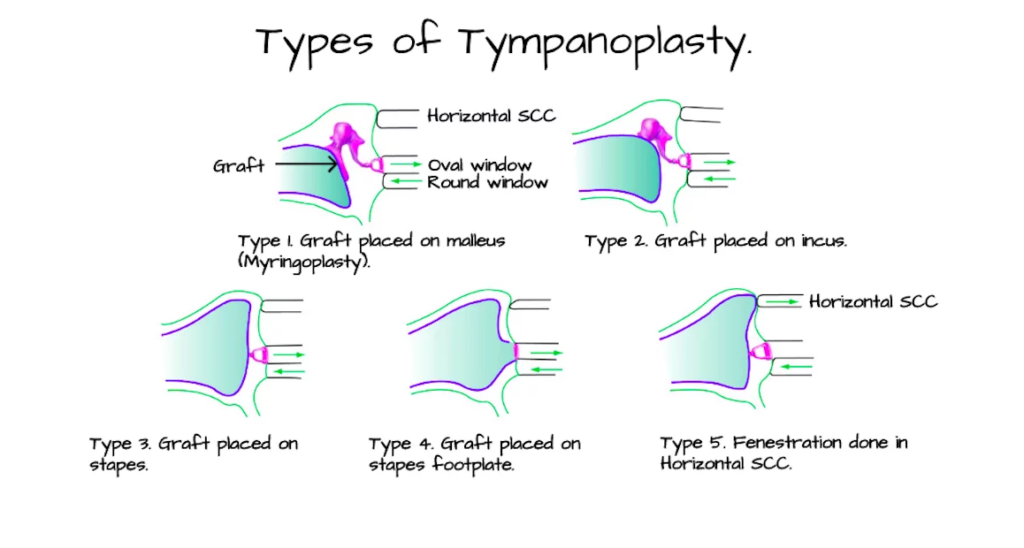
Types of Tympanoplasty. Wullstein classified tympanoplasty into five types.
| Type I | There is only perforation in the tympanic membrane which is repaired with a graft and ossicular status is checked. |
| Type II | Defect is perforation of tympanic membrane with erosion of malleus. Graft is placed on the incus or remnant of malleus. |
| Type III | Malleus and incus are absent. Graft is placed directly on the stapes head. It is also called myringostapediopexy or columella tympanoplasty. |
| Type IV | Only the footplate of stapes is present. It is exposed to the external ear, and graft is placed between the oval and round windows. A narrow middle ear (cavum minor) is thus created to have an air pocket around the round window. A mucosa-lined space extends from the eustachian tube to the round window. Sound waves in this case act directly on the footplate while the round window has been shielded. |
| Type V | Stapes footplate is fixed but round window is functioning. In such cases, another window is created on horizontal semicircular canal and covered with a graft. Also called fenestration operation. |
Anaesthesia. General anaesthesia is preferred for all chronic ear surgery procedures.
Tympanoplasty approaches.
1. Endomeatal or Transcanal Approach. This approach is used for small posterior perforations and when the size of the ear canal is large. It avoids postauricular incision scar mark and mastoid dressing in the postoperative period. It is used in
- Exploratory tympanotomy to find cause for conductive hearing loss
- Inlay myringoplasty
- Ossicular reconstruction.
Steps:
- Margins of perforation is denuded.
- Tympanomeatal flap (posterior meatal canal skin) is elevated using Rosen’s incision in continuity with tympanic membrane, after dislocating the annulus from the sulcus
- The middle ear and ossicular chain are inspected and repaired as necessary.
- Posterosuperior over-hang of bony meatus if present should be removed in order to see stapes
- The middle ear is then packed with gelfoam.
- The graft is placed medial to the tympanic membrane remnant, or tympanic annulus, and the manubrium of the malleus.
- Then tympanomeatal flap is returned to its original position and the medial aspect of the ear canal is packed with gelfoam impregnated in antibiotic ointment

Rosen’s incision : It consists of two parts: (i) a small vertical incision at 12 o’clock position near the annulus and (ii) a curvilinear incision starting at 6 o’clock position to meet the first incision in the posterosuperior region of the canals, 5–7 mm away from the annulus.
2. Endaural Approach. It is rarely used today due to the visibility of the scar and limitation of exposure posteriorly. It is used for:
- Excision of osteomas or exostosis of the ear canal.
- Large tympanic membrane perforations.
- Attic cholesteatomas with limited extension into the antrum.
- Modified radical mastoidectomy where the disease is limited to attic, antrum and part of the mastoid.
Endaural approach consists of two parts:
(i) Lempert 1st incision. It is semi circumferential incision, made along the entire posterior half of the ear canal at the bony-cartilaginous junction of the posterior meatal wall from 12 o’clock to 6 o’clock position.
(ii) Lempert 2nd incision. Starts from the first incision at 12 o’clock and then passes vertically upwards in a curvilinear fashion between the tragus and the root of helix. It passes through the incisura terminalis and thus does not cut the cartilage. Both mastoid and external canal surgery can be done.

3. Postaural (or Wilde’s) Incision. It is the most preferred approach for large perforations especially perforation located anteriorly and when canal size is small. The incision starts from the highest attachment of the pinna, follows the curve of retroauricular groove, lying 1 cm behind it, and ends at the mastoid tip.
In infants and children, up to 2 years of age, who have not yet developed a mastoid tip and the facial nerve lies exposed near its exit, and the incision, therefore, is slanting posteriorly, avoiding lower part of the mastoid. Some surgeons prefer to make the postaural incision in the sulcus (retroauricular groove). It has a disadvantage of poor visualization of the anterior sulcus may result in improper graft placement and failure of the procedure.
Postaural incision is used for:
- Cortical mastoidectomy.
- Modified radical and radical mastoidectomy.
- Tympanoplasty: when perforation extends anterior to handle of malleus.
- Exposure of CN VII in vertical segment.
- Surgery of endolymphatic sac.

Grafting material. Temporalis fascia or the perichondrium from the patient are most commonly used graft materials. Homografts such as dura, vein, fascia or cadaver tympanic membrane are also sometimes used.
Graft placement techniques. There are two tympanoplasty grafting techniques, underlay and overlay. Both techniques give excellent results provided they are properly performed by experienced surgeons.
- Underlay technique – The graft is placed medial to the inner mucosal layer of the tympanic membrane remnant (or fibrous annulus) and manubrium of the malleus. It is stabilized by gelfoam in the middle ear. It is comparatively easy to perform. Disadvantages associated are graft medialization and reduction of middle ear space. Nitrous oxide gas should be avoided during placement of graft because it diffuses into the middle ear and can displace the graft.
- Overlay technique – The graft is placed lateral to the middle fibrous layer of the tympanic membrane remnant (or fibrous annulus) and medial to manubrium of the malleus. The graft is placed after carefully removing the outer epithelial layer of tympanic membrane remnant. Overlay technique has more complications such as the formation of epithelial pearl (due to failure to completely remove the squamous epithelium of the ear canal or TM remnant), anterior sulcus blunting, formation of granulation tissue and graft lateralization. It is technically more demanding procedure.
Complications of tympanoplasty:
- Intra operative Bleeding (due to high and uncovered jugular bulb)
- Facial nerve palsy
- Wound infection/ Perichondritis
- Wound Hematoma
- Chorda Tympani Nerve Injury
- Graft failure
- Sensorineural Hearing Loss/ Dizziness
(iii) Myringoplasty: Myringoplasty can be defined as the surgical repair of the tympanic membrane without any other work in middle ear or mastoid.
History
- 1640s Artificial animal-based plugs were used.
- Cotton wool – Yearsley described an artificial eardrum consisting of moistened cotton wool.
- Toynbee describes an artificial eardrum comprising a gutta-percha disc and a silver wire.
- William Wilde and Roosa advocated the use of cautery to the remnant tympanic membrane to encourage healing. Silver nitrate and trichloracetic acid were commonly used agents.
- Blake first described the paper patch on its own in 1887.
- Joynt (1919) combined cautery with the use of a paper patch overlying the perforation.
- In 1878 Berthold described technique of using full-thickness skin graft, describing this alongside ‘freshening’ or excision of the perforation edges to ‘render these parts into a wound’; he also coined the term ‘myringoplasty’.
- Ely described a similar technique but his work was not published until a year later in 1879.
- Until the 1950s with Wullstein’s split skin graft and Zollner’s pedicled skin graft that higher rates of successful repair were being reported.
- Wullstein in 1956 classified tympanoplasty, with myringoplasty being classified as a Type I tympanoplasty.
Indications of myringoplasty: The three principal indications for myringoplasty are
- Recurrent otorrhea
- Hearing loss due to a chronic perforation.
- Desire to swim without having to waterproof the ear.
Contraindications of myringoplasty:
- Cholesteatoma
- ASOM
- Contralateral dead ear.
- Eustachian tube dysfunction
- Medically Unfit
- Actively discharging ear
- Otitis externa
- Complicated CSOM
- Eustachian tube blocked
- Malignant tumours of the outer/middle ear
- Unusual infections such as malignant otitis externa
- Poor general health
Complications of myringoplasty:
- lntraoperative Bleeding (due to high and uncovered jugular bulb)
- Myringitis can occur
- Wound lnfection/ Perichondritis
- Wound Hematoma
- Injury to chorda tympani
- Graft failure
- Sensorineural Hearing Loss/ Dizziness
(iv) Ossiculoplasty: Ossiculpolasty is the reconstruction of the ossicular chain. Ossicles are important for the transmission of sound from the tympanic membrane to the labyrinth. Ossicular chain discontinuity or fixation (congenital or acquired) causes conductive hearing loss. The aim of ossiculoplasty is to surgically rebuild a sound conducting chain.
Classification of ossicular defects:
Austin– Kartush is the most accepted classification which applies to situations without intact incus. It helps to define pre-operative ossicular status to facilitate meaningful analysis of surgical outcomes. Austin proposed it in 1971 with four categories, and later it was modified by Kartush in 1994 with the addition of three further categories.
| TABLE: Austin classification | |||
| Group | Ossicular status | Abbreviation | Prevalence (%) |
| A | Malleus handle and stapes superstructure present | M+ S+ | 60 |
| B | Malleus handle present, stapes superstructure absent | M+ S− | 23 |
| C | Malleus handle absent, stapes superstructure present | M− S+ | 8 |
| D | Malleus handle and stapes superstructure absent | M− S− | 8 |
| TABLE: Modifications by Kartush | |
| Group | Ossicular status |
| O | Intact ossicular chain |
| E | Ossicular head fixation |
| F | Stapes fixation |
Ideally, ossiculoplasty should be done in a dry, stable well-ventilated middle ear, with an intact tympanic membrane, without any middle ear infection or cholesteatoma. Kartush devised a Middle Ear Risk Index (MERI) which helps in the stratification of risk factors by giving a score of 0–16. It gives an idea preoperatively about successful outcome following surgery.
| TABLE: Middle Ear Risk Index 2001 | |
| Otologic factor | Maximum score |
| Otorrhoea | 3 |
| Perforation | 1 |
| Cholesteatoma | 2 |
| Ossicular status | 4 |
| Middle ear granulation | 2 |
| Previous surgery | 2 |
| Smoking | 2 |
Different types of prosthesis with different materials can be used to replace ossicles depending on the ossicular defects. Autografts, allografts and homografts can be used to bridge the gap. Low-tension with a short prosthesis results in better sound transmission and low risk of displacement than high-tension with a long prosthesis.
| TABLE: Materials used for ossicular reconstruction | ||
| Type of graft | Material | Remarks |
| Autograft | – Incus, head of malleus – Cortical bone from mastoid |
– Risk of harbouring disease – Low cost – Easily available |
| Allograft | – Plastipore (polyethylene sponge) – Hydroxyapatite (HA) implants – Titanium implants – Glass isomer – Teflon prosthesis – HA (50%) + Titanium (50%) – HA + Silicon (flex-HA) – HA + Polyethylene (HAPEX) |
– Readymade Easy to store and use – Costly Likely to be extruded |
| Homograft | – Preserved ossicles only – Ossicles with tympanic membrane |
– Difficult to procure – Risk of disease transmission |
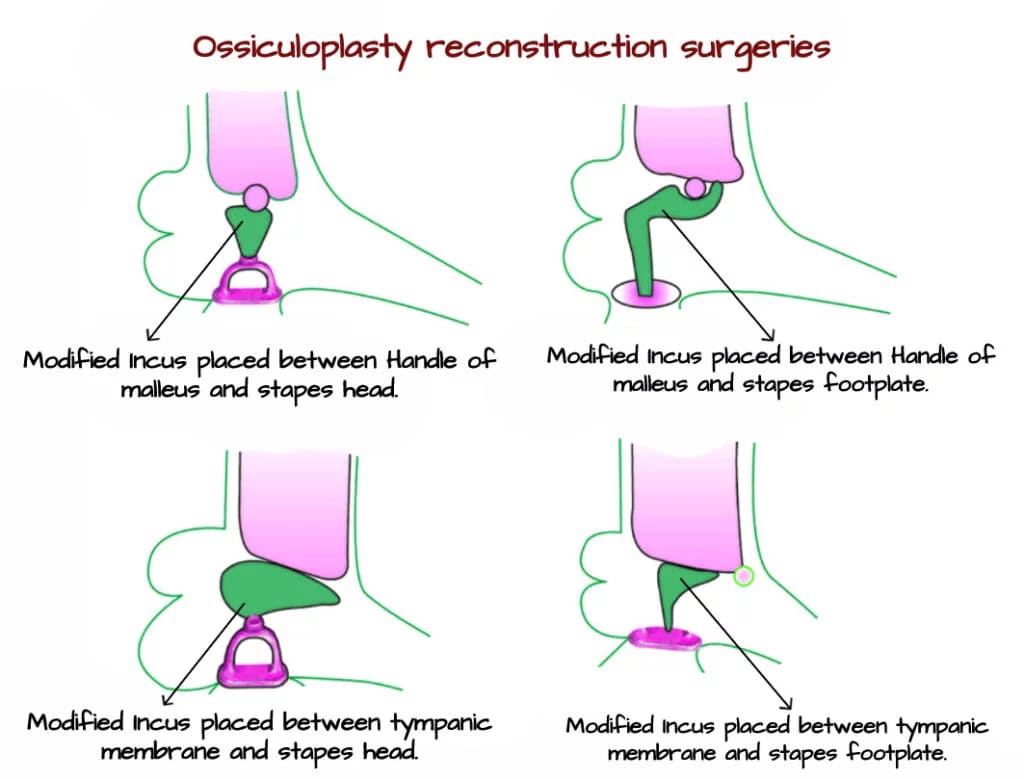
TABLE: Surgical options to correct specific defects.
| S No. | Ossicular defect | Surgical Options for Correction | Important points |
| 1. | Eroded long process of the incus | A. Bridging With Autologous Tissue with cortical bone – harvested from the mastoid or external auditory canal – or cartilage B. Incus Prosthesis C. Bone Cement/Bone Pate: The use of bone cement to reconstruct the long process of the incus is a more recent development and has been shown to give good hearing results at least in the short term. Care must be taken when applying bone cement to avoid spillage onto the stapes footplate or unintended fixation to the posterior canal wall. |
It is most common ossicular chain defect.Early attempts to restore hearing in cases of ISJ separation included stapediopexy where the tympanic membrane is brought into direct contact with the stapes head.There is disadvantage of losing the amplification and dampening functions of the ossicular chain. |
| 2. | Eroded incus with malleus and stapes present (Austin–Kartush type A) | A. Autologous Ossicles Interposition Placing the body of the incus on the stapes head with the short process directed towards the malleus handle and medial to it. B. Partial Ossicular Replacement Prosthesis: 1. Stapes to malleus prosthesis – Advantages Preservation of the catenary lever mechanism of the tympanic membrane. Placing the prosthesis medial to the handle of the malleus may also reduce the rate of extrusion. Drawback Inefficient energy transfer vector of force is never perfectly in the line of the stapes 2. Stapes to tympanic membrane prosthesis – Disadvantage Catenary lever mechanism is lost Prosthesis may be unstable. |
In cases where the incus is partially or completely eroded and anatomical reconstruction of the ossicular chain is not possible, there are several alternative options for restoring hearing when the malleus handle and stapes superstructure remain intact. |
| 3. | Malleus present, stapes absent (Austin–Kartush type B) | A. Homograft Ossicle Homograft incus has been used extensively for this purpose with most reports describing the long process resting on the footplate and a sculpted notch at the opposite end to accommodate the malleus handle. B. Total Ossicular Replacement Prosthesis The strut in TORPs is longer to reach the stapes footplate, and the medial end of the prosthesis is often flattened to rest on the footplate rather than cupped. Some TORP are shaped specifically to accommodate the malleus handle with a notch or groove, whereas others have a flat disc leaving both footplate-to-malleus and footplate-to-tympanic membrane options open. One of the challenges of this type of reconstruction is the tendency for prosthesis displacement. Stability may be improved with a cartilage ‘shoe’ or a specially designed footplate prosthesis. |
When the stapes superstructure is absent, mechanical coupling between the stapes footplate and the tympanic mem-brane or malleus handle must be achieved. This type of reconstruction is inherently less stable due to the distance that must be bridged and the absence of a fixed attachment point on the stapes footplate. |
| 4. | Malleus absent, stapes present (Austin–Kartush type C) | A. Stapes to tympanic membrane prosthesis – Disadvantage Catenary lever mechanism is lost Prosthesis may be unstable. B. Neo Malleus – Recreate the malleus handle, either with autologous material or with a prosthesis. C. Malleus replacement prosthesis |
Absence of the malleus handle to be a major independent prognostic factor resulting in poorer hearing outcomes following reconstruction. This is partly due to the loss of the amplification produced by the tympanic membrane– malleus handle complex, and loss of a solid point of fixation for any reconstructed assembly. |
| 5. | Malleus and stapes absent (Austin–Kartush type D) | It may be managed with a combination of the above techniques and will require reconstruction with autologous tissue, ossicle interposition or TORP. The reconstruction may be footplate-to-tympanic membrane, or alternatively a neo–malleus or malleus replacement prosthesis may be used to improve stability. | This is the most challenging ossicular defect and is likely to lead to the poorest outcomes. |
B. SENSORINEURAL HEARING LOSS: Sensorineural hearing loss (SNHL) occurs when there is failure in the cochlear transduction (change in mechanical energy into electrical energy) process from going to neural impulses of the eighth nerve. It occurs due to damage or impairement in cochlea (sensory) or eighth cranial nerve (retrocochlear) and its central connections (central deafness). This causes reduction in the sensitivity of the cochlear receptor cells.
The characteristics of sensorineural hearing loss are:
- A positive Rinne test, i.e. AC > BC.
- Weber lateralized to the better ear.
- Bone conduction reduced on Schwabach and absolute bone conduction tests.
- There is poor speech discrimination which means that the patient is able to hear the speech but not able to understand it.
- There is difficulty in hearing in the presence of noise.
- Recruitment phenomenon (abnormal loudness growth) may be present.
- Hearing loss may range from minimal to total and is usually permanent.
- Usually treated with hearing aids or implants. Options for medical or surgical interventions are very limited.
The characteristics of sensorineural hearing loss on PTA:
- AC and BC thresholds being within 10dB of each other.
- High frequencies are mostly involved.
- Loss may exceed 60 dB, generally complete hearing loss.
AETIOLOGY
Congenital. Congenital SN hearing loss may be due to inner ear anomaly or pre-natal/perinatal damage to hearing apparatus.

TABLE: Syndromes associated with SNHL (Congenital)
| S No | Syndrome | Features | Type of hearing loss | Onset (Congenital/ delayed) | Type of inheritance |
| 1. | Waardenburg syndrome | • White forelock • Heterochromia iridis • Vitiligo • Dystopia canthorum |
Unilateral or bilateral SNHL | Congenital | AD |
| 2. | Usher syndrome | • Retinitis pigmentosa • Night blindness |
SNHL | Delayed | AR |
| 3. | Jervell and Lange- Nielson syndrome | • Repeated syncopal attacks • Prolonged QT interval in ECG |
SNHL | Congenital | AR |
| 4. | Pendred syndrome | • Goitre (nontoxic) usually evident before puberty • Perchlorate discharge test shows defect in organic binding of iodine |
SNHL | Congenital | AR |
| 5. | Alport syndrome | • Hereditary progressive glomerulonephritis • Corneal dystrophy |
Progressive SNHL | Delayed | AD or X-linked |
| 7. | Crouzon syndrome (craniofacial dysostosis) | • Frog eyes (exophthalmos with divergent squint) • Hypertelorism • Parrot-beak nose • Mandibular prognathism • Premature closure of cranial sutures with mental retardation |
Conductive or mixed | Congenital | AD |
| 9. | Klippel-Feil syndrome | • Short neck • Fused cervical vertebrae • Spina bifida • Atresia of ear canal |
SNHL or mixed | Congenital | AR |
| 10. | Wildervanck syndrome | • Klippel-Feil syndrome • SNHL • CN VI Paralysis |
SNHL | Congenital | X-linked |
| 11. | Branchio-oto-renal syndrome | • Branchial fistulas/cysts • Malformed pinnae with preauricular pits or sinuses • Renal abnormalities |
Conductive or mixed | Congenital | AD |
| 12. | Stickler syndrome | • Small jaw • Cleft palate (Pierre-Robin sequence) • Myopia ≥ retinal detachment • Cataract • Juvenile onset arthritis |
Conductive or SNHL | Delayed | AD |
| 13. | Van der Hoeve syndrome | • Osteogenesis imperfecta with history of fractures • Blue sclera • Hearing loss (delayed onset) |
Conductive, SNHL or mixed (like otosclerosis) | Delayed | AD |
| 14. | Pierre-Robin sequencea | • Micrognathia • Glossoptosis • Cleft palate • Often part of Stickler syndrome |
SNHL / Conductive loss | AD | |
| 15. | Goldenhar syndrome (Facio- auriculo-vertebral dysplasia) or (oculo- auriculo-vertebral [OAV] syndrome) | • Facial asymmetry • Low set ears, atresia of ear canal • Cardiac abnormalities • Preauricular tags/pits • Hemivertebrae in cervical region • Epibulbar dermoid • Coloboma of upper lid |
Mixed or conductive | Congenital | AD or sporadic Extra chromosome Multifactorial (genetic and environmental) |
Acquired causes of SNHL. It develops later in life. It can be genetic type or non-genetic type. The genetic type may affect only hearing part (non-syndromic), or be a part of a syndrome affecting other systems of the body as well (syndromic).
Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss Types of Hearing Loss
Common causes of acquired SNHL include:
- Infections of labyrinth—viral, bacterial or spirochaetal
- Noise-induced hearing loss
- Ototoxic drugs
- Presbycusis
- Sudden hearing loss
- Meniere’s disease Refer to page no.
- Acoustic neuroma Refer to page no.
- Trauma to labyrinth or VIIIth nerve.
- Familial progressive SNHL
- Systemic disorders, e.g. diabetes, hypothyroidism, kidney disease, autoimmune disorders, multiple sclerosis, blood dyscrasias.
| S No. | Causes of Bilateral SNHL | Causes of Unilateral SNHL |
| 1. | Presbycusis | CSOM |
| 2. | Meniere’s disease | Mumps |
| 3. | Otosclerosis | Herpes zoster oticus |
| 4. | Noise-induced hearing loss | Acoustic neuroma |
———— End of the chapter ————
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
