Table: Diseases of External Ear
| Congenital disorders | Pinna – Microtia, Macrotia, Bat ear, Coloboma, Deformities of Ear Lobule. EAC – Congenital Atresia, Collaural fistula. |
| Infection and Inflammatory disorders. | Pinna – Perichondritis, Relapsing Polychondritis, Wrinkler’s Nodule. EAC – Furuncle, Diffuse Acute Otitis Externa, Otomycosis, Haemorrhagic otitis externa, Herpes Zoster Oticus, Aural polyps, Acquired atresia of EAC. Tympanic Membrane – Retraction, Retraction Pockets and Atelectasis, Myringitis, Atrophic Tympanic Membrane, Tympanosclerosis, Perforations. |
| Non-inflammatory disorders | Pre-auricular appendage (tags), Preauricular pit, Preauricular Sinus, Keloid of Auricle, Gouty Tophi. |
| Trauma | Pinna – Haematoma of the Auricle, Auricular Pseudocyst, Lacerations, Avulsion of Pinna, Frostbite. EAC – External canal trauma. Tympanic Membrane – Traumatic rupture of tympanic membrane, |
| Bony lesions | Exostosis, Keratosis Obturans, Cholesteatoma of External Auditory Canal, Malignant (Necrotizing) Otitis Externa, Skull base osteomyelitis. |
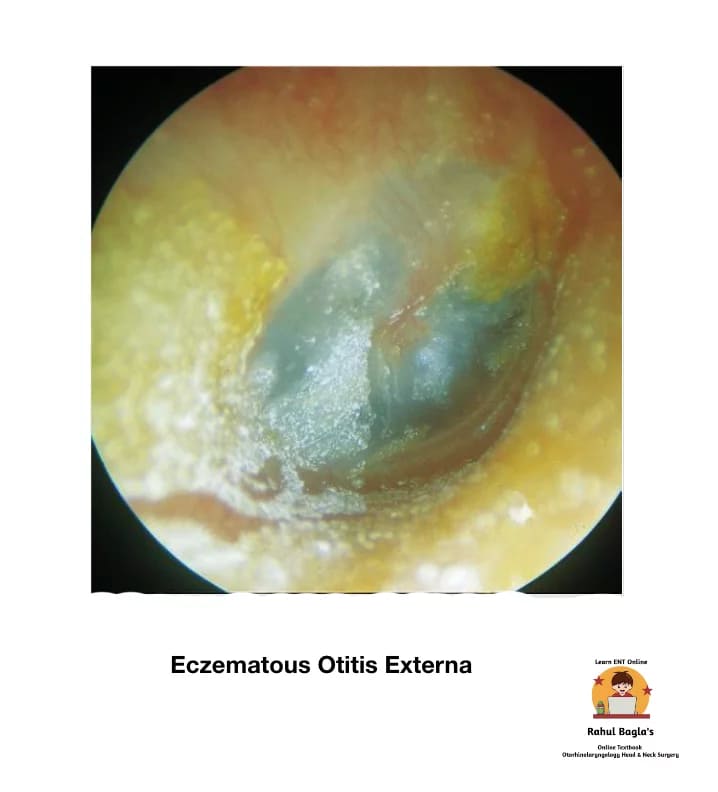
| Reactive dermatological disorders | Eczematous Otitis Externa, Neurodermatitis, Seborrhoeic Otitis Externa. |
| Miscellaneous | Impacted Wax or Cerumen. |
CONGENITAL DISORDERS
Congenital disorders of Pinna
(i) Microtia means small-sized pinna. It may be unilateral or bilateral with hearing loss. Peanut ear is a form of microtia. Anotia means absence of pinna.
(ii) Macrotia. Large pinna.
(iii) Bat ear (Syn. Lop-Ear, Protruding Ear) means abnormally protruded ear. Concha is large with poorly formed antihelix and scapha. Surgical correction is advisable only after 6th birthday of the child.
(iv) Coloboma. A transverse cleft is seen in the middle of the pinna.
(v) Deformities of Ear Lobule. There may be absence of lobule, large lobule, bifid lobule or an attached lobule.
Treatment options:
- Surgical correction/ otoplasty procedures.
- Prosthetic ear.
- Hearing Aid. (BAHA, Bilateral BTE or Body worn)
- Speech therapy.
Congenital disorders of External Auditory Canal
(i) Congenital Atresia (absence of passage) of EAC may be congenital and acquired. Congenital atresia of the meatus may occur alone (as a result of failure of canalisation of the ectodermal core that fills the dorsal part of the first branchial cleft) or more commonly, it may occur in association with microtia.

As re-canalization of EAC starts from the deeper part near the tympanic membrane and progresses outwards, at times the deeper meatus is developed while the outer canal is obliterated with fibrous tissue or bone. Atresia may be associated with abnormalities of the middle ear, internal ear and other structures.
Types of atresia
- Solid atresia occurs with a fibrous tissue alone or with both fibrous as well as bony material. The solid atresia may be blunt or tapering in shape, and produce a funnel-shaped medial aspect to the lumen of the ear canal. Surgery is challenging.
- Membranous atresia: The skin of the ear canal is covered with a skin, that separates the ear canal into a medial and lateral segment. The skin of the medial segment may at times desquamate, collect keratin and even become erosive (to form external canal cholesteatoma).
Investigations
- Examine thoroughly to detect any other associated anomaly.
- Hearing tests.
- CT scan is needed to detect the bony and soft-tissue part of the external ear and differentiate solid from membranous atresia.
Management.
Hearing rehabilitation: BAHA, Cochlear implant.
Surgical: Atresiaplasty can reduce conductive hearing loss to 25 dB. Cosmesis can be achieved with a prosthesis or other surgical techniques.
(ii) Collaural fistula or cervico-aural fistula is a rare abnormality of the first branchial cleft. The fistula has one opening in the neck just below and behind the angle of mandible and the other opening in the external canal or the middle ear. The track of the fistula passes, close to the facial nerve and through the parotid gland. The definitive treatment is surgical exploration and excision.
INFECTIONS OR INFLAMMATORY DISORDERS
Infections Or Inflammatory Disorders Of Pinna
(i) Perichondritis is an inflammation of perichondrium

Causes:
- Results from the extension of an infection from cellulitis, diffuse otitis externa, furuncle of the meatus or ‘high’ piercing of the cartilaginous area of the auricle.
- Infection may be secondary to lacerations, untreated haematoma, frostbite, burns, chemical injury or surgical incisions.
Causative micro-organisms:
- Gram-positive: Pseudomonas, staphylococcus aureus.
- Gram-negatives: Proteus, enterococcusand Escherichia coli.
- Mixed flora
Pathology: The cartilage gets its blood supply from perichondrium. Whenever serous fluid accumulates between the cartilage and perichondrium (due to trauma/ inflammation), the perichondrium is lifted from the cartilage. Avascular necrosis, fibrosis, intense infiltration with polymorphonuclear leukocytes, thickening of the perichondrium and destruction of the cartilage by phagocytes are usual pathological findings. The lobule, which contains no cartilage, is spared.
Symptoms:
- Red, hot, stiff and painful pinna movement.
- Pyrexia and malaise.
- Cauliflower ear deformity may occur because of extensive destruction of cartilage.
- Rare complications of perichondritis include fatal septicaemia, subacute bacterial endocarditis and necrotizing fasciitis of the neck.
Signs:
- Tenderness
- Fluctuation, if pus is present.
Prevention :
- Avoid tight head bandages during ear surgery
- Avoid ear piercing in cartilaginous pinna.
- Drain haematomas under aseptic conditions.
- Burn injuries should be managed with prophylactic antibiotics against Gram-negative bacteria, daily dressings and the removal of eschars and crusts.
Treatment:
- Systemic antibiotics, particularly against P. aeruginosa
- Local application of 4% aluminium acetate compresses.
- Abscess must be aspirated and irrigation with an antibiotic solution.
- Culture and sensitivity of the pus should be obtained.
- The incision is made in the natural fold and devitalized cartilage is removed. A fenestrated polyethylene tube/catheter may be placed in the subperiosteal tunnels on either side of the cartilage. The necrosed cartilage needs to be debrided in non-responsive case.
- Total chondrectomy is done if the entire area is involved.
(ii) Relapsing Polychondritis. It is a rare autoimmune disorder and is characterized by severe, episodic and progressive inflammatory condition involving cartilaginous structures throughout the body especially ears (most common), nose and laryngotracheobronchial tree.

Symptoms
- Sudden onset otalgia
- Inability to sleep on affected side
- Floppy ear
- Decreased hearing
The whole auricle excluding ear lobe is red and tender. Canal stenosis may be present. The mainstay of treatment is high doses of systemic corticosteroid therapy.
(iii) Chondrodermatitis Nodularis Chronica Helicis (Wrinkler’s Nodule). It is an intensely painful benign inflammatory process which presents with small and tender solitary nodules of the helix and sometimes antihelix of the pinna. The nodules are round in shape, with well-defined margins, and usually pale, grey, or slightly erythematous. Usually seen in elderly men above 40-50 years of age. There is inability to sleep on affected side. Suggested aetiology are exposure to sunlight, trauma or pressure over pinna during sleep.

Treatment.
Medical. Topical steroids and adhesive padding bandaging.
Surgical. Complete excision of nodule with its skin and immediately involved cartilage.
Infections Or Inflammatory Disorders Of External Auditory Canal
(i) Furuncle/ Boil/ Deep folliculitis (Localized acute otitis externa): It is an infection around the hair follicle (usually seen in the cartilaginous part of the meatus ) that turns into a pustule and progresses to form a local abscess. Furuncle may occur as a single lesion or may spread to involve surrounding structures (cellulitis).

Pre-disposing factors: Scratching the canal with contaminated sticks or metallic objects, trauma to EAC, immune-compromised patients (diabetes), allergy, hereditary, use of improper size of ear moulds of hearing aids and stethoscope.
Symptoms:
- Excruciating pain and tenderness which are out of proportion to the size of the furuncle.
- Pain in the ear during chewing and movements of the pinna.
- If canal is stenosed there is conductive hearing loss and feeling of ear blockage.
- Purulent discharge is sometimes seen.
Signs:
- Tragal sign is positive (Tenderness present over tragus).
- EAC will be oedematous making otoscopic examination difficult.
- Swelling over the mastoid with obliteration of the retroauricular groove.
- Periauricular lymph nodes may also be enlarged and tender.
- Otoscopic examination may be difficult if canal is severely oedematous.
Complication : Repeated infection may cause permanent scarring and fibrosis of EAC & lead to stenosis of meatus.
Treatment:.
- When there is no abscess, the patient can be managed with hot fomentation, systemic/oral antibiotics and analgesics.
- A small ear pack of 10% ichthammol glycerine alleviates pain, reduces oedema and has antiseptic action. Intranasal mupirocin ointment can be prescribed.
- If abscess has formed, incision and drainage is required
- In recurrent furunculosis, diabetic status should be evaluated, and the patient’s nasal vestibules and fingers need to be checked for staphylococci. The pathogenic strain may even colonize in nostrils and even perineum.
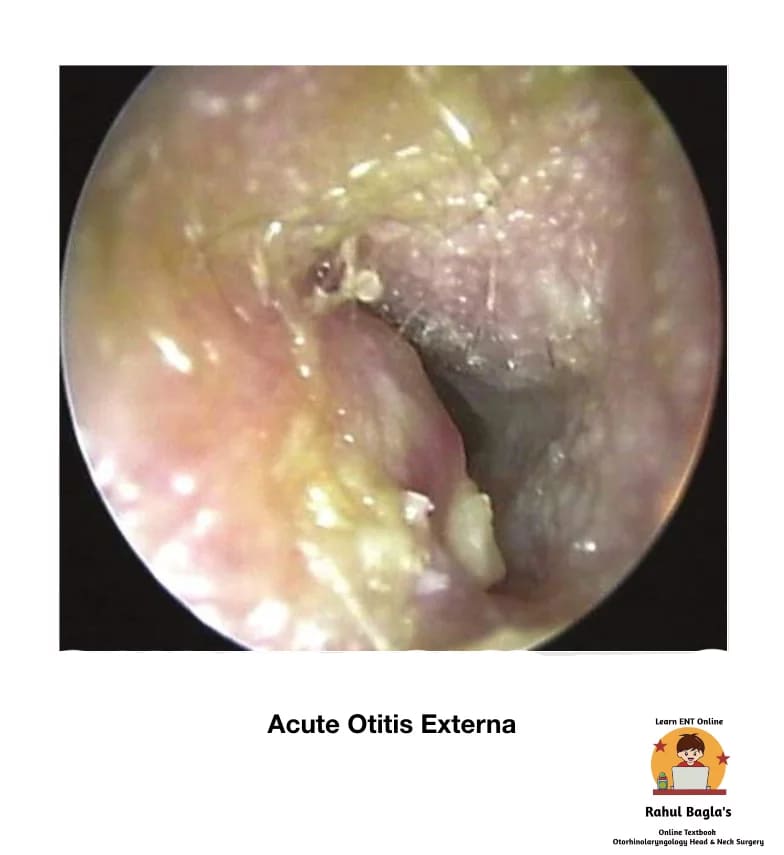
(ii) Diffuse Acute Otitis Externa (Swimmer’s ear)
It is a generalized inflammation of the meatal skin and subcutaneous tissue of the external auditory canal. The infection may further spread to involve the pinna and epidermal layer of the tympanic membrane.
Etiology.
- Anatomical: Narrow external auditory meatus (hereditary, iatrogenic, exostoses, trauma). EAC obstruction due to keratosis obturans, wax, foreign body, hearing aid, in-ear headphones.
- Allergic: Atopy, non-atopic allergy, exposure to topical ear drops.
- Trauma: Ear probing, skin maceration (bathing or irrigation), laceration, radiotherapy.
- Bacterial: Staphylococcus aureus, Pseudomonas pyocyaneus, Bacillus proteus and Escherichia coli. However, most cases are of mixed infection. Warm & humid environment favours the growth of bacteria.
- Dermatological: Eczema, seborrheic dermatitis, psoriasis.
- Immune compromised states (diabetics).
Clinical features.
Diffuse otitis externa is a clinical diagnosis made from these symptoms and signs: pain, itching, oedema and erythema of EAC with purulent otorrhoea and debris in the meatus.
Acute phase: The patients experiences a hot, burning sensation in the ear. This pain is aggravated on jaw movements. A thin serous discharge oozes out, which later becomes thick and purulent. The meatal lining becomes inflamed and swollen. Conductive deafness may occur due to collection of debris, discharge and swelling of the meatus. In severe cases, local lymph nodes are enlarged and tender. There may be cellulitis of the surrounding tissues.
Chronic phase: The patient complains of irritation and a strong desire to itch in the ear. The habit of itching increases chances of acute exacerbations and recurrent infection. The discharge is scanty and may get dried up to form crusts. The thick and swollen meatal skin may show scaling and fissuring. Rarely, the meatal skin becomes hypertrophic and lead to meatal stenosis (chronic stenotic otitis externa).
Pathology of diffuse otitis externa
| Stage | ||
| 1 | Pre-inflammatory | There is disruption of the protective lipid/acid balance (normal pH 4–5). Stratum corneum is oedematous, sebaceous and apocrine glands gets blocked producing features like aural fullness and itching. |
| 2 | Acute inflammatory | Further oedema, obliteration of the lumen and increase in pain. In the severe stages, cervical lymphadenopathy may be seen. |
| 3 | Chronic inflammatory | By definition, chronic otitis externa occurs after 6 months. It is characterised by thickening of the skin of ear canal. |
Treatment.
- Aural toilet: Regular and thorough removal of all exudate and debris.
- A wick soaked in an antibiotic-steroid preparation is inserted in the ear canal and the patient is instructed to keep it moist by instilling the ear drops twice or thrice a day. The wick must be changed every day (for 2-3 days) and then it is substituted by ear drops.
- Steroid drops relieve oedema, erythema and prevent itching.
- A wick of mild astringent like aluminium acetate (8%) or silver nitrate (3%) can be used to form a protective coagulum and dry-up oozing meatus.
- Ear pack with 10% ichthammol glycerine provides splintage and reduces pain. Hygroscopic action of glycerine reduces oedema, while ichthammol is mildly antiseptic.
- Analgesics are prescribed for pain relief.
- Broad-spectrum systemic antibiotics for treating complications.
Outcomes and complications.
- A mild case of otitis externa resolves spontaneously because the epithelial barrier gets re-developed, pilo-apocrine units produce normal secretions and the pH of the canal returns to normal.
- However, in cases where inflammation is progressing at a faster rate than repair, the condition of the patient deteriorates. There is increase in intensity of pain, otorrhoea and oedema of the canal occurs.
- Due to the rich lymphatic drainage of the area, lymphadenopathy often occurs and soft-tissue infection can progress leading to perichondritis, chondritis, cellulitis, parotitis and/or erysipelas.
- In the immunocompromised host, malignant otitis externa (periostitis/ osteomyelitis of the skull base) can develop.
(iii) Otomycosis. It is a superficial mycotic infection of the external ear canal. Otomycosis is suspected if the patients with otitis externa fail to respond to topical antibiotic/steroid drops.
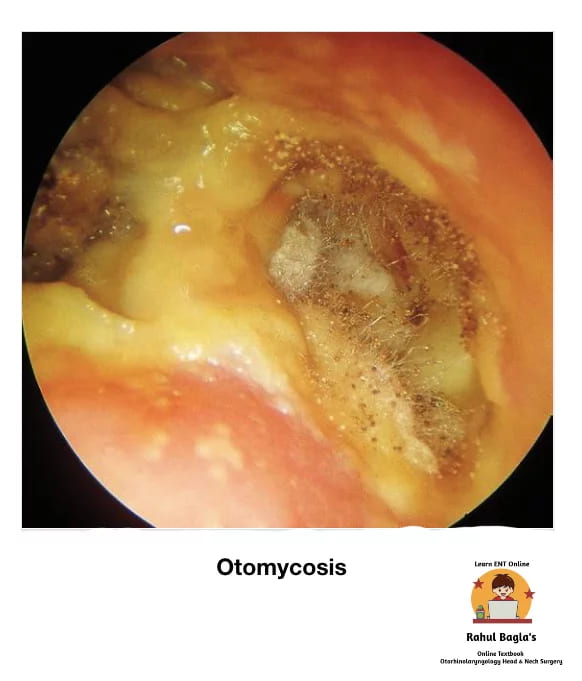
Predisposing factors:
- Hot and humid climate of tropical and subtropical countries.
- Secondary fungal growth to prolonged topical antibiotics.
- Diabetes & other immune-compromised status.
- Swimming.
Causative micro-organisms:
- Aspergillus niger : commonest, black- headed filamentous growth.
- Aspergillus fumigatus: Pale blue or green in colour.
- Candida albicans: white or creamy deposit.
- Actinomycosis.
- Dermatophytes.
Clinical features: The patient complains of itching, irritation, discomfort or severe pain in the ear (mainly in aspergillus flavus infection). The meatal skin appears red and oedematous. Other features are watery discharge with a musty odour, ear blockage, decreased hearing. The fungal mass may appear white, brown or black looks like awet piece of filter paper or sheets.
Investigations:
- Culture sensitivity and fungal smear.
- Blood sugar for diabetes.
Treatment:
- Cleaning/debridement of the ear canal by syringing, suction or mopping.
- Keeping ear canal dry is a paramount step in management.
- Antifungal drops for one week (nystatin, clotrimazole and povidone-iodine)
- Anti-histaminic ear drops to relieve itching
- Anti-inflammatory analgesics
- 2% salicylic acid in alcohol to remove the superficial epidermal layer along with fungal mycelium growing in this layer.
- Treat underlying cause e.g. diabetes.
- In cases of resistant otomycosis, fungal infection elsewhere in the body must be excluded and treated with systemic antibiotics.
(iv) Haemorrhagic otitis externa may develop as a post-influenza complication. The patient complains of severe pain in the ear and there is formation of blood-filled haemorrhagic bullae on the tympanic membrane and deep meatal walls. If bullae rupture, there may be blood-stained discharge.
Treatment : Analgesics and antibiotics
(v) Herpes Zoster Oticus. It is a viral infection involving geniculate ganglion of the facial nerve. It is characterized by the appearance of vesicles on the tympanic membrane, deep meatus, concha and retroauricular sulcus. It is caused by the re-activation of the latent Varicella Zoster virus in the geniculate ganglion. It may involve VIIth (more often) and the VIIIth cranial nerves. The syndrome is more common in old age >60 years.

Herpes zoster oticus
Clinical features:
- Anaesthesia of face, giddiness and hearing impairment due to involvement of Vth and VIIIth nerves.
- Excruciating (severe) otalgia.
- Vesicles in EAC on affected side Facial nerve palsy (LMN type).
- Tinnitus, vertigo and a sensorineural hearing loss.
Complications:
- Post herpetic neuralgia.
- Eye damage (blurred vision) may occur.
- Hearing loss & facial weakness may be permanent.
Prognosis. The prognosis for Ramsay Hunt is worse than idiopathic facial palsy. Persistent weakness is observed in 30–50% of patients. Only 10% recover completely after complete loss of function without treatment.
Prevention. Children are vaccinated against chickenpox, reduces their chances of getting infection
Treatment:
- The recommended regime is prednisone 1mg/kg/day for 5 days then tapered for 10 days, and intravenous acyclovir (250 mg three times daily). The combination of steroids and acyclovir also seems to reduce otalgia, vertigo and post-herpetic neuralgia.
- Oral acyclovir 800mg 5 times a day for 7-10 day.
- Surgical decompression is not indicated.
(vi) Aural polyps. Aural polyps are well-circumscribed, soft, fleshy masses frequently found in the EAC. They are inflammatory in nature and generally arises from the middle ear and suggestive of active disease in the middle ear. Polyps may also result from secondary to chronic inflammation due to a foreign body (i.e. grommet) in the middle ear. Additionally, polyps may be seen as a manifestation of myringitis, malignant otitis externa, or other neoplastic or inflammatory lesion. Histopathologic examination can be done if the cause of a polyp is unknown. Polyp has an epithelial lining that differentiates it from granulation tissue.
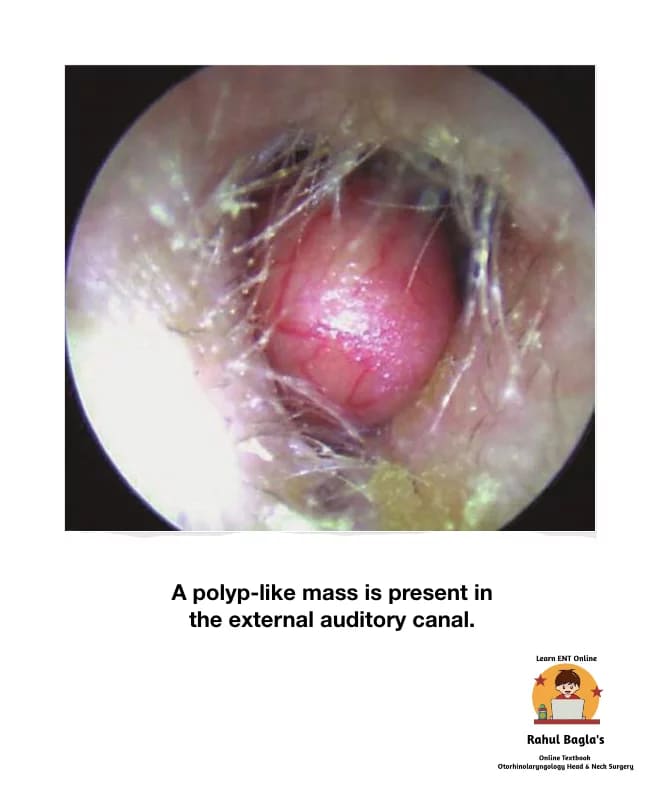
Differential diagnosis
Neoplastic and granulomatous conditions such as tuberculosis, syphilis, xanthomatosis and eosinophilic granuloma.
Investigations
CT scan is advisable if polyp is not responding to medical treatment or if cholesteatoma is suspected.
Management
Gentle aural toilet and use of antibiotic steroid containing topical ear drops will reduce the inflammatory response. It decreases the size of polyp and allows access for examination. Cauterization with silver nitrate can also be done. Biopsy can be done on polyps of uncertain origin, to rule out malignancy. Polypectomy should be performed if the polyp persists, if necessary under anaesthesia. Polyps must not be removed or avulsed blindly as they may be adherent to the stapes superstructure, dehiscent facial nerve, or cholesteatoma overlying a labyrinthine fistula.
(vii) Acquired atresia of EAC. Atresia is defined as the absence or closure of EAC.
It is caused by the following processes:
- Inflammation
- Chronic otitis externa
- Reactive dermatological disorders (i.e. eczematous otitis externa)
- Chronic suppurative otitis media
- Trauma
- Open injury (lacerations, gunshot injury)
- Fracture mandible
- Facial injury
- Fracture of the tympanic plate
- Burns. It can be thermal, chemical, electrical or post-irradiation.
- Surgery. Any meatal approach surgery (i.e. tympanoplasty)
Treatment:
Medical
- Topical ear drops (corticosteroid and antibiotic preparation)
- Regular atraumatic aural toilet may prevent the need for surgical intervention.
- Cauterization with silver nitrate or trichloroacetic acid of granulation tissue.
Surgical
Meatoplasty is done by removing the fibrous tissue by elevating it from the ear canal bone, the fibrous annulus and lamina propria of the tympanic membrane, through an endaural or retroarticular approach. It can be combined with tympanoplasty especially in solid cases.
Infections Or Inflammatory Disorders Of Tympanic Membrane
(i) Retraction, Retraction Pockets and Atelectasis of Tympanic Membrane. Retraction of the tympanic membrane is a common finding in both children and adults. TM appears dull and lustreless. Middle ear negative pressure develops due to eustachian tube blockage results in retraction or retraction pockets in tympanic membrane. A deep retraction pocket may collect keratin debris and form a cholesteatoma.

Stages of retraction of Pars Tensa
- Stage I. Tympanic membrane is retracted but does not contact the incus. Cone of light is absent or interrupted.
- Stage II. Tympanic membrane is retracted on long process of incus.
- Stage III. Also called middle ear atelectasis. Tympanic membrane lie on the promontory. But moves on seigalization or Valsalva manoeuvre.
- Stage IV. Also called adhesive otitis media. Tympanic membrane gets adherent to the promontory and does not moves on seigalization or Valsalva manoeuvre.
Stages of retraction of Pars Flaccida
- Stage I. The pars flaccida is dimpled and more retracted than normal but not adherent to the malleus.
- Stage II. The retraction is adherent to the neck of the malleus.
- Stage III. Partial erosion of the bony attic wall
- Stage IV. Definitive Erosion of bony attic wall
(ii) Myringitis. It is inflammation of the tympanic membrane.
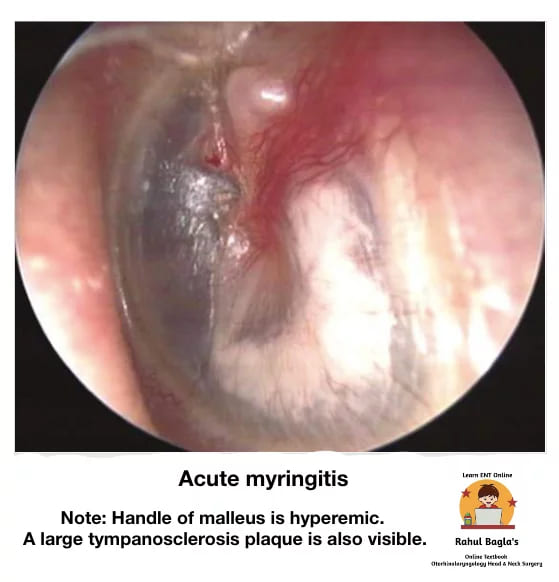
Types of myringitis:
- Acute bullous myringitis
- Granular chronic myringitis.
(i) Acute bullous myringitis. It is an acute painful inflammatory condition characterized by the presence of bullae (single or multiple) or vesicles on the tympanic membrane and adjacent bony part of the meatus. Causative organisms are similar to those seen in acute otitis media. The bullae develop between the middle fibrous and outer squamous layer of the TM.
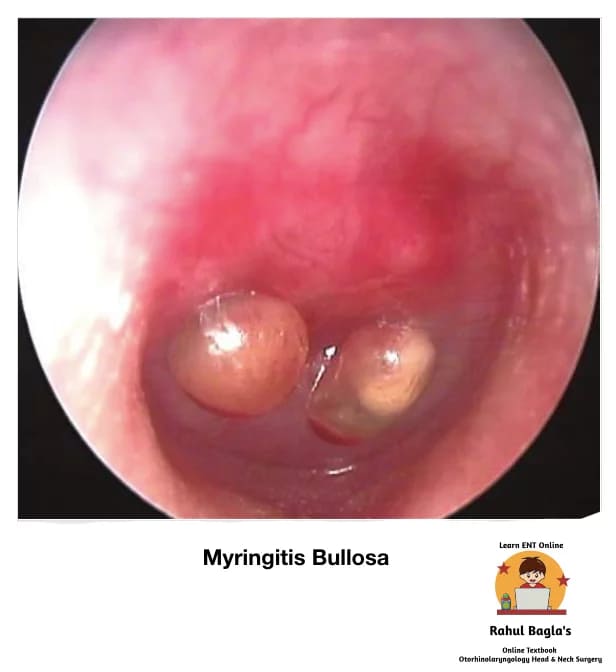
Presentation
- Sudden-onset severe unilateral otalgia, often along with upper respiratory tract infection.
- Scanty serosanguinous ear discharge following rupture of the bulla
- Hearing loss is transient and recovers fully. Conductive hearing loss is very common. Mixed or sensorineural hearing loss is also well documented.
- Fullness in ears
Treatment
- It is a self-limiting disease.
- Management same as for AOM.
- Symptomatic treatments described include analgesia, warm compresses and incision of bullae.
(ii) Granular chronic myringitis. It is a chronic inflammatory disorder characterized by the presence of nonspecific granulations following deepithelialization of the outer (epithelial) layer of the tympanic membrane (TM) and there is no middle ear disease.
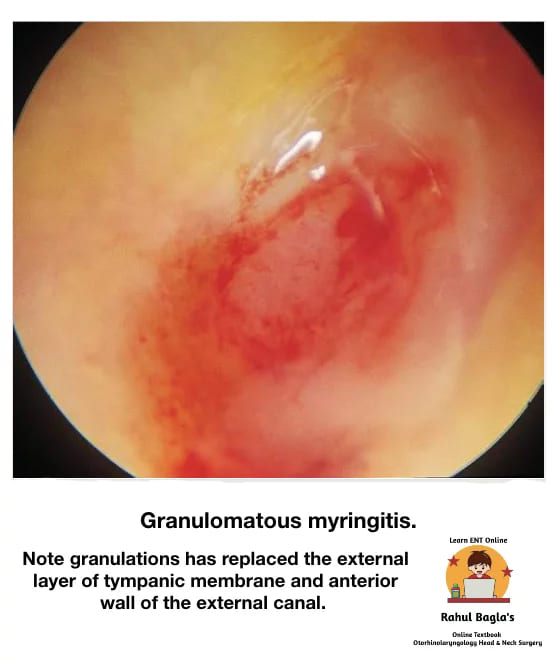
Aetiology. Unknown.
Possible causes are:
- Injury to outer layer of TM may impair epithelialization and promote granulation tissue formation.
- Eustachian tube blockage.
- External ear infection.
Presentation
- Persistent or recurrent painless ear discharge, which can be foul smelling.
- Itching or fullness of ears.
- Mild conductive hearing loss.
- Some patients may not have symptoms at all.
On examination.
- Granulation tissue/ polyp is present replacing normal squamous epithelium. It may be localized or diffused. Most commonly seen in posterosuperior region. It may also involve adjacent bony part of the meatus.
- Thickened TM.
Management
- Topical antibiotic and antifungals, often with a steroid/ anti-inflammatory agent.
- Topical antiseptic agents (i.e. acetic acid)
- Dilute vinegar solution is an effective simple alternative to topical antibiotic drops.
- Silver nitrate cauterization of granulation tissue.
(iii) Atrophic Tympanic Membrane. It is thinning of the pars tensa of TM due to absence of middle fibrous layer making it weak and prone to retraction and reperforation. It may also remain stable for many years. It is usually circular in outline and sometimes called replacement membrane. It can occur in the following conditions:
- Long-standing serous otitis media. Enzymes present in the middle ear effusion causes loss of middle fibrous and elastic layers of TM.
- It is also end result of natural healing of tympanic membrane perforation as it heals only by epithelial and mucosal layers without the middle fibrous layer.
(iv) Tympanosclerosis. It develops in the middle fibrous layer of the tympanic membrane between the outer epidermis and inner mucosal epithelium of the tympanic membrane.
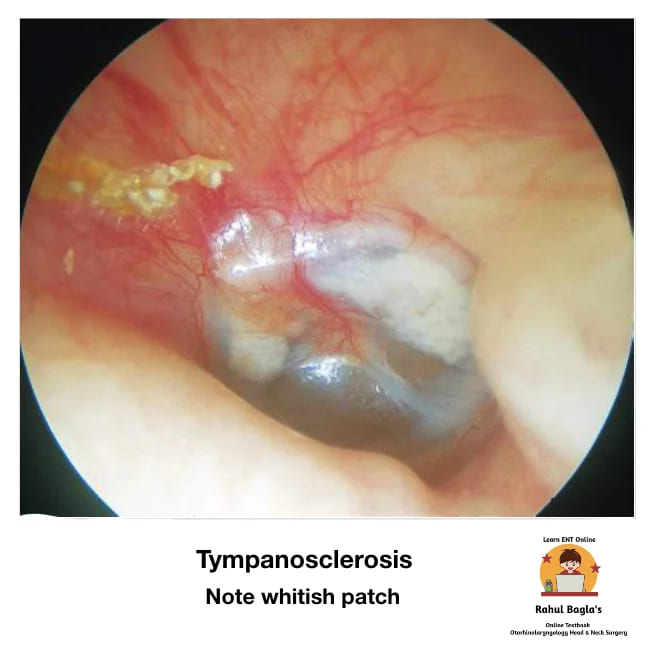
It is characterized by hyaline degeneration and later on calcification of the tympanic membrane and the middle ear mucosa. The hyaline deposits consist of acellular material seen as chalky white plaques and white nodular deposits. It mostly affects only tympanic membrane (myringosclerosis) and rarely results in significant hearing loss. Middle ear tympanosclerosis may involve ligaments, joints of ossicles, middle ear cleft and can cause ossicular fixation and result in more severe degrees of conductive hearing loss.
(v) Perforations. They may be central, attic or marginal and are associated with chronic otitis media.
NON- INFLAMMATORY DISORDERS
(i) Pre-auricular appendage (tags) consists of skin and fat that appear on an imaginary line drawn from tragus to the angle of mandible. A few pieces of cartilage may be present and called accessory auricle.
Treatment. Simple excision may be done after 1 years of age to improve facial symmetry and cosmesis.
(ii) Preauricular pit is a bilateral depression present anterior to crus of helix or above the tragus. Usually asymptomatic, if infected symptoms are pain, swelling and ear discharge.
Treatment : Antibiotics if infected and then complete excision can be done.
(iii) Preauricular Sinus. Preauricular sinus is an epithelial track extending medially to end blindly. It may open in EAC, parotid gland or in the region of collaural fistula. There is incomplete fusion of tubercles. Repeated infection causes purulent discharge and later abscess formation is treated by surgical excision of the whole track. Sinogram/ fistulogram may be advised to know the extent of tract.
(iv) Keloid of Auricle. Keloids are benign, hypertrophic, fibrous lesions which often invade adjacent normal area causing cosmetic deformities. They usually develop as a result of ear piercing, trauma or surgery. Common sites are ear lobule or helix.
Treatment options.
- Triamcinolone injection locally for small and fresh keloids gives good results.
- For larger and more mature ones, surgical excision is required. Intralesional corticosteroid injection can be given intraoperatively and repeated after every 4 to 6 weeks for a minimum three times in order to minimize the risk of recurrence.
- Excision with KTP-532, CO2 Laser.
- Pre and postoperative low dose radiation may avoid recurrence. but there is risk of radiation-induced malignancy.
(v) Gouty Tophi
It is generally seen in patients suffering from hyperuricemia. Patient present with small subcutaneous nodule due to deposition of uric acid crystals. Most common is site helix, Nodules appears as moderately painful, salmon-pink in colour. A whitish, chalky substance consisting of sodium biurate comes out on compression.
Treatment : Anti-inflammatory analgesics for pain relief and correction of abnormality in uric acid metabolism
TRAUMA
Trauma of Pinna
(i) Haematoma of the Auricle.
Aetiology.
- Blunt trauma. Commonly seen in wrestling, boxing and rugby players.
- Rarely, Hypertensive or patients with severe coagulopathies develop spontaneous haematomas.
Pathogenesis. Shearing between auricular cartilage and its perichondrium leads to formation of potential space, where blood fills following the rupture of small vessels. It usually occurs on the anterior (lateral) surface of the pinna. following blunt trauma. Later, entry of chondroblasts forms granulation tissue resulting into new cartilage formation.
Outcome. Breeches in perichondrium leads to cartilage buckling of cartilage forming Cauliflower ear/ pugilistic or boxer’s ear deformity (which is hyperplastic proliferation of cartilage following repeated trauma and inflammation).
Treatment
Aspiration. Prompt treatment in first 48 hrs. Evacuation of haematoma and removal of granulations with pressure dressing and antibiotic coverage, avoids high recurrence rate. Incision and drainage to be done if re-aspirations fails.
Techniques of aspiration
- Anterior approach. Two incisions are made, first along inferior border of the helix along the scapha, second in antihelical fold, or along conchal fold, as required. The flap is elevated, taking care of posterior skin. The flap is then returned and sutured after aspiration and curettage.
- Posterior approach. Mainly for cosmesis. A 5mm window of cartilage is removed, on the posterior aspect, taking care not to perforate the anterior skin. Closure is not required.
Other treatment method.
- Injection of sclerosants, such as OK-432.
- Steroids.
- streptomycin with hyaluronidase.
- triamcinolone or even fibrin glue can also be used, although two or three treatments per ear are often required.
(ii) Auricular Pseudocyst (Benign Idiopathic Cystic Chondromalacia).
It is an intracartilaginous cystic collection, containing viscous, straw-coloured, sterile fluid and devoid of any epithelial lining. It is painless and asymptomatic. Usually with no history of preceding trauma.
Treatment. Same as hematoma auricle but, curettage is not required as no granulation tissue is present here.
(iii) Lacerations.
Aetiology. Same as external canal trauma
Treatment.
- Measures to avoid any deformity.
- Inj. TT as prophylaxis
- Course of broad-spectrum antibiotics for 1 week.
- Aspiration of blood in case of hematoma formation.
- Incision and drainage if required.
- Wound debridement to remove necrotic tissue.
- The perichondrium is stitched with absorbable sutures and skin with nonabsorbable sutures. Avoid stripping of perichondrium from cartilage as it may lead to avascular necrosis. Suturing with or without free and or pedicled flap.
(iv) Avulsion of Pinna. Primary correction is generally successful if pinna is still attached to the head by a small pedicle. Completely avulsed pinna can be reimplanted in selected cases by the microvascular techniques; in others, the skin of the avulsed segment of pinna is removed and the cartilage implanted under the postauricular skin for later reconstruction.Prosthesis in cases of avulsion of pinna.
(v) Frostbite. Aetiology. Exposure to extreme cold.
Pathogenesis. Extreme cold cause ice crystals and obstruction of vessels leading to erythema and oedema, bullae formation, necrosis of skin and subcutaneous tissue and complete necrosis with loss of the affected part.
Signs. Pinna initially may appear red but later turns blue depending upon duration of exposure.
Treatment.
- Tissue warming via circulating warm water or warmed moistened dressings at a temperature of 38–42 °C.
- Local application of 1% silver sulfadiazine soaks for superficial infection.
- Analgesics for pain.
- Systemic antibiotics directed against Pseudomonas aeruginosa and Staphylococcus aureus for secondary infection.
- Protection of bullae from rupture.
- Surgical debridement of necrotic tissue should be delayed until a reliable line of demarcation develops.
Trauma Of External Auditory Canal
(i) External canal trauma.
Aetiology
- Injury with blunt or sharp object.
- Physical assault.
- Fall from height.
- Road traffic accident.
- Sports injury.
Treatment
- Minor injuries (injury byscratching the ear with sharp or blunt objects like hair pins, needles or matchstick or unskilled instrumentation by the physician) or abrasions usually requires no treatment and heal spontaneously.
- If blood is coming out of meatus, suspect injury in ear canal, tympanic membrane.
- Extreme bleeding may indicate an associated jugular bulb tear.
- If trismus is there, suspect temporal bone and mandible (trismus) fractures. Any meatal soft tissue should be left alone pending imaging to exclude herniation of brain/meninges. The goal of treatment is to achieve a skin-lined meatus of sufficient diameter to prevent stenosis of the ear canal.
- CSF leaks close spontaneously, requires conservative management. Surgical intervention is via a middle fossa approach if required.
Trauma Of Tympanic Membrane
(i) Traumatic rupture of tympanic membrane. Traumatic perforation may result from blunt or penetrating injuries as well as rapid changes in barometric pressure. Common causes are:
- Penetrating injury due to a hair pin, matchstick or unskilled instrumentation to remove wax or foreign body.
- Rapid changes in barometric pressure, e.g. a slap or a kiss on the ear, forceful Valsalva manoeuvre or a sudden implosive blast (pressure wave).
- Pressure by a fluid column, e.g. diving, aquatic sports or forceful syringing.
- Foreign bodies such as button batteries, other caustic substances, insects.
- Temporal bone fracture.
- Thermal injuries, commonly seen in welders and those struck by lightning.
Signs. On examination, there is perforation and congestion of tympanic membrane with inverted margins. Blood clots may also be seen.
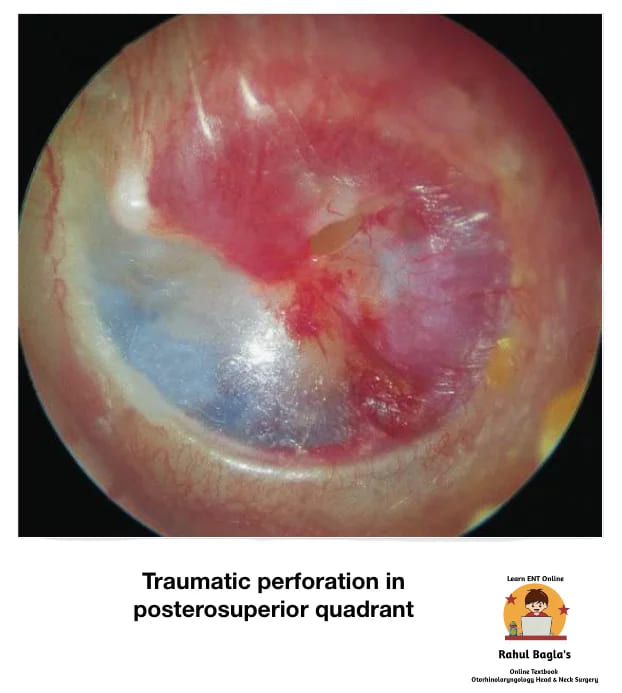
Symptoms
- Decreased hearing, mainly conductive.
- Pain in ear
- Tinnitus
- Headache
- Occasionally vertigo
Management.
- Pure tone audiometry is advised for type and degree of hearing loss.
- No ear drops is advised and no attempt to clean ear should be made.
- Antibiotics, decongestants is advised and symptomatic treatment should be given.
- Button batteries should always be removed as a matter of urgency.
- Prophylactic antibiotics can be advised to avoid infection.
Spontaneous healing takes 1-3 months. Therefore formal repair is advisable only after 3 months. Options are:
- Cauterization of margins of perforation with trichloroacetic acid or silver nitrate.
- Edges of perforation repositioned and splinted under operating microscope.
- Paper patches or gel foam is also used surgically.
- Myringoplasty
- In case of facial paralysis or subluxation of stapes (vertigo and nystagmus) and sensorineural hearing loss, needs urgent exploration.
BONY LESIONS
(i) Exostosis. An exostosis of EAC is a benign bony growth of periosteal compact bone. It presents as smooth, sessile, hemispherical swelling in the deep part of the canal, close to the tympanic membrane. They are usually multiple, usually three in numbers, and are bilateral, commonly arising from the anterior and posterior walls of EAC. It is usually seen incidentally while examining a asymptomatic patient, but there may be a history of recurrent otitis externa, chronic infection, wax and debris accumulation and conductive hearing loss. Males are affected three times more than females.

It needs to be differentiated from osteoma, sometimes called synonym of exostosis, which is generally a unilateral, solitary, discrete, pedunculated mass, arising from the lateral part of the bony EAC.
High-resolution computed tomography (CT) scan is choice of investigation for exostosis.
Aetiology.
- Chronic entry of cold water in the ear, commonly seen among divers and swimmers.
- Repeated episodes of otitis externa.
Symptoms.
- Usually asymptomatic and diagnosed as an incidental finding.
- Blocked sensation and itching because of the wax collection.
- Conductive hearing loss.
Management options.
- In the majority of small and asymptomatic cases, no treatment is required.
- Avoidance of cold water with a recommendation to use earplugs.
- Aural toilet
- Topical application of steroid, antibiotic, antifungal or combination ear drops, may be necessary to treat inflammation or infection.
- Surgery. It is usually required for cases refractory to medical treatment or large sized exostosis causing repeated infection or conductive hearing loss. Meatoplasty procedure via a postaural, endaural or permeatal approach is done to restore normal size of the canal. with careful elevation and preservation of skin overlying the exostoses. The bone of exostoses is removed by high-speed drill, with preservation of skin above the exostosis. Avoid damage to the tympanic membrane and facial nerve.
(ii) Keratosis Obturans. Is due to failure of epithelial migration in TM causing accumulation of a pearly white mass of desquamated keratin in the bony part of EAC. It is associated with osteitis and granulation tissue formation causing extensive bony erosion leading to gross widening or ballooning of canal to the point at which facial nerve can also get involved. KO can occur both in normal ears or in ears having plugs of keratin. Intracranial complications are not seen.
Pathophysiology. Normally, epithelium from surface of tympanic membrane migrates onto the posterior meatal wall. In KO there is grossly abnormal migration pathway of epithelium or obstruction to migration caused by wax causing accumulation of large keratin plugs in bony part of EAC.
Aetiology.
- Unknown.
- Hyperaemia of skin and
- Irritability of epidermis.
Clinical features. Presenting Symptoms may be
- Acute severe otalgia.
- Marked conductive hearing loss, occasionally bilateral.
- Tinnitus.
- Sometimes ear discharge.
- Facial palsy LMN type is also seen.
- TM is not involved.
- It is commonly seen in young age.
- 90% of patients have a past history of bronchiectasis or sinusitis.
On examination
- Pearly white mass of keratin material.
- Gross widening or ballooning of bony meatus.
- Ulceration and even granuloma formation.
- Tympanic membrane shows moderate degrees of thickening.
Treatment.
- Local debridement of the plug by syringing or instrumentation in LA/GA.
- Waxolytic agents (2% sodium bicarbonate) to soften the mass.
- Periodic check-up and cleaning in follow-up with acetic acid solution or keratolytic agent such as 2% salicylic acid in alcohol may reduce accumulation of debris.
- Meatoplasty with skin grafting is effective treatment in cases of repeated canal occlusion and severe otalgia.
(iii) Cholesteatoma of External Auditory Canal. Cholesteatoma of the EAC is similar to keratosis obturans as both shows keratin debris in the canal. However, they are distinct clinical entities. It can be acquired secondary to trauma, surgery or chronic inflammation or may arise spontaneously. The lesion is typically in the floor of the EAC. it should also be differentiated from exostosis. A probe is used to palpate the mass. If its consistency is tender and soft, cholesteatoma is diagnosed.
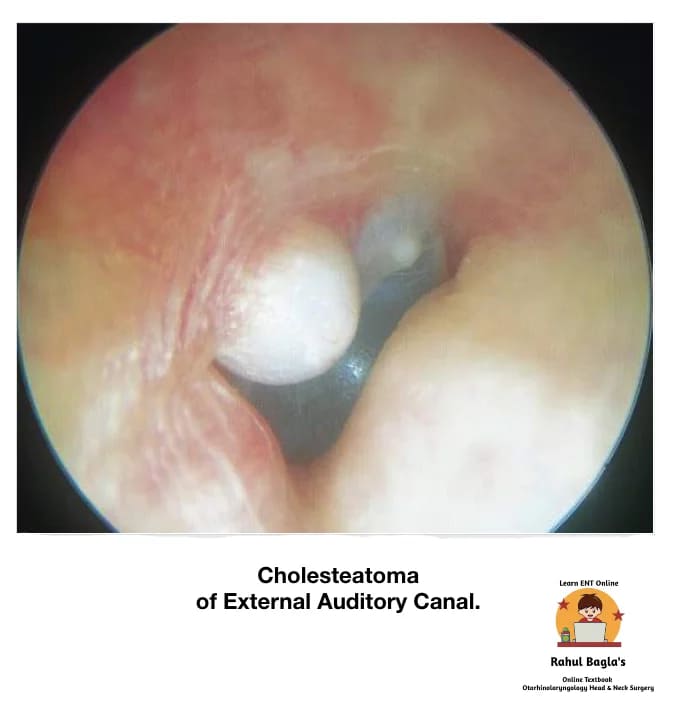
Aetiology.
- Uncertain
- Infection of abnormal bone exposed in EAC which later on sequests leading to epithelial migration on to this bony abnormality and the cholesteatoma is formed.
Clinical features.
- Chronic otorrhoea with dull pain or itching;
- Feeling of blockage
- Tympanic membrane being normal.
- No associated hearing impairment.
- Usually unilateral.
- Mostly seen in older patients.
Granulations associated with sequestrated bone need histological examination to differentiate it from carcinoma, necrotizing otitis externa and a benign sequestrum.
Differential diagnosis.
- Skull base osteomyelitis (SBO)
- Squamous cell carcinoma.
Treatment.
- If the extent of the cholesteatoma erosion is visible – Conservative management.
- If the extent of the cholesteatoma erosion is not visible – Removal of necrotic bone and cholesteatoma and repair of the defect using temporalis fascia.
- Disease involving the mastoid may warrant tympanomastoidectomy to remove involved bone and repair associated defects.
(iv) Malignant (Necrotizing) Otitis Externa. It is an severely progressive necrotizing Pseudomonas infection of the ear canal. Infection may rapidly spread to entire temporal bone and jugular foramen causing involvement cranial nerves (IX, X, XI, and XII) and may lead to skull base osteomyelitis. It is usually seen in immunocompromised patients, particularly the elderly diabetics, and in patients on long steroid therapy or chemotherapy. Facial paralysis is commonly seen. In an elderly diabetic patient with severe otalgia and granulation tissue in the external ear canal at its cartilaginous–bony junction is a cardinal sign of skull base osteomyelitis and should not be underestimated.
In an elderly diabetic patient with severe otalgia and granulation tissue in the external ear canal at its cartilaginous–bony junction is a cardinal sign of skull base osteomyelitis and should not be underestimated.
Spread.
- Anteriorly, infection may spread to the skull base at the most vulnerable portion of the external canal, the osseocartilaginous junction, and proceed to infiltrate the parotid gland and facial nerve by way of the fissures of Santorini.
- Inferiorly, traversing the tympanomastoid suture and fissures of Santorini provides access to the infratemporal fossa and jugular foramen, placing cranial nerves IX, X, and XI at risk for injury. Proximal injury results from involvement of the main trunk at the stylomastoid foramen via direct extension from the external auditory canal.
- Medially, infection may spread to the marrow spaces of the skull and eventually the petrous apex, placing cranial nerves V and VI at risk.
- Posteriorly, by direct extension into the pneumatized spaces of the mastoid, where the vertical segment is at risk.
Pathogenesis. Normally, cerumen provides protective function in controlling the pH that prevents maceration and excessive bacterial colonization. It is proposed that these protective features of cerumen are absent among patients with diabetes, permitting bacterial overgrowth and increased susceptibility to tissue invasion. Diabetic microangiopathy results in ischemic, nutritionally deficient, devitalized tissue. The infective process produces exotoxins and enzymes like elastase which digests vessel wall. Impaired local and systemic immune systems lack the ability to control local infection, permitting progression of uncomplicated otitis externa to a fulminate, systemic invasive infection.
Symptoms.
- Penetrating excruciating earache which is continuous and severe in nature and commonly out of proportion to the clinical examination findings.
- Persistent ear discharge not relieving on multiple courses of medications. Discharge is initially mucopurulent and later becomes foul smelling purulent and blood tinged.
- Both CHL and SNHL can occur
- Facial paralysis.
- Headache
- Vertigo
Signs.
- Granulation tissue seen protruding into the EAC from the bony-cartilaginous junction
- Sagging of posterior meatal wall.
- Tympanic membrane. May be normal.
- Pinna. Tenderness is present and doughy on palpation.
- Mastoid tenderness
- Multiple cranial nerves (IX, X, XI, XII) involvement is seen in late stages.
Investigations.
- Culture sensitivity by ear swab.
- CT scans help to evaluate the extent of bony involvement but MRI provides more details regarding soft-tissue disease and can also evaluate the patency of the dural sinuses if combined with magnetic resonance angiography,
- Gallium-67 bone scan helps in confirming the diagnosis and follow-up of the patient. It is taken up by monocytes and reticuloendothelial cells, and is indicative of soft tissue infection. It can be repeated every 3 weeks to monitor the disease and response to treatment.
Differential diagnosis
- Diffuse otitis externa. There is absence of excruciating pain and presence of granulations in the ear canal.
Treatment.
Long-term administration of parental antibiotics, in combination with daily extensive debridement of necrotic and granulation tissue and vigilant management of diabetes and other compromising medical conditions. Surgical management is currently not indicated, diagnostic biopsies can be done to rule out malignancy. Anti-pseudomonas antibiotics should be given for minimum 2-3 months. Antibiotics found effective are:
- Gentamicin combined with ticarcillin.
- Third-generation cephalosporins. e.g. ceftriaxone 1–2 g/day i.v. or ceftazidime 1–2 g/day i.v. are usually combined with an aminoglycoside.
- Quinolones (ciprofloxacin, ofloxacin and levofloxacin) are also effective and can be given orally. They can be combined with rifampin.
- Ciprofloxacin (750mg orally twice per day) seems to be the antibiotic of choice for maintainence and prolonged treatment for a minimum of 3 months to 1 year may be required, to avoid relapse.
- In case there is resistance to ciprofloxacin, antipseudomonal β-lactam agents (ceftazidime, piperacillin, imipenem) with or without combination of aminoglycoside can also be used. Aspergillus infection if found need systemic antifungal treatment.
(v) Skull base osteomyelitis (SBO) typically presents in an immune-compromised host with severe otalgia and unilateral otorrhea. There may be invasion of local structures and necrosis of skin, cartilage and bone. Cranial nerve palsies may ensue with involvement of the petrous apex, typically the facial nerve but the trigeminal, abducens and lower cranial nerves may also be affected. Pseudomonas aeruginosa is by far the most common pathogenic micro-organism, although other pathogens have been identified.
Chronic inflammation may cause progressive soft tissue stenosis of the EAC and result in a false fundus. This may cause a conductive hearing loss, but the chronic otorrhea may cease.
Investigations.
Cross-sectional imaging of the skull base is helpful in achieving diagnosis and monitoring progress in SBO. High-resolution CT can demonstrate bone erosion, although magnetic resonance imaging (MRI) is more sensitive to detect skull base inflammation and cranial nerve involvement.
No changes are specific for SBO, so radionucleotide investigations may be helpful:
- Technetium 99m bone scintigraphy is sensitive in detecting bony involvement and is therefore used for diagnostic purposes.
- Gallium 67 scintigraphy is used to monitor the response to treatment. Biopsy of any granulations or sequestrum is mandatory to exclude a (true) malignancy.
A CT scan can be helpful to exclude middle-ear pathology in a patient with an obstructed tympanic membrane.
Management.
Fluoroquinolones (particularly ciprofloxacin) are the treatment of choice, with a high cure rate when used for prolonged periods. Antimicrobial resistance to ciprofloxacin is emerging and must be suspected in patients with deteriorating clinical features (such as new cranial nerve palsies) or rising inflammatory markers. Hyperbaric oxygen has been used with some benefit as an adjuvant to antimicrobials, but a Cochrane review found no randomized controlled trials to support this treatment
REACTIVE DERMATOLOGICAL DISORDERS
Pathology: Epidermis of the skin of EAC is susceptible to the same dermatologic conditions seen elsewhere in the body. As the skin is very thin and present in almost closed space it gives most annoying symptoms. Usually, all these disorders will respond to local care and removal of allergic factors. Systemic steroids can be given in severe inflammatory disease.
(i) Eczematous Otitis Externa. It is allergic dermatitis and hypersensitivity reaction due to topical ear drops (chloromycetin or neomycin etc), infective organisms, jewellery or cosmetic products. It is marked by severe chronic itching, redness, vesicle formation, oozing, crusting, fissuring even stenosis of canal may be present. Treatment is removal of allergic factors (ear drops) causing sensitivity and use of antihistaminics with application of steroid cream and prophylactic antibiotics.
(ii) Neurodermatitis (lichen simplex chronicus). It is a neurological disorder characterized by chronic and compulsory itching due to psychological factors. Otitis externa may occur due to repeated scratching. The aetiology is unknown, but insect bite and stress may trigger this condition. Treatment: Psychotherapy and bandage to ear to avoid compulsive itching.
(iii) Seborrhoeic Otitis Externa. It is very common clinical condition and may remain unnoticed to many patients. It is usually associated with seborrhoeic capitis. It is believed to be triggered by excessive growth of “yeast like fungi” called Malassezia that lives harmlessly on the skin, or an hypersensitivity reaction by the skin’s immune system to this yeast. Affected areas can be itchy, sore, greasy yellow scales may be present. Treatment is aural toilet, application of ointment containing salicylic acid and sulphur, and treating the scalp condition.
MISCELLANEOUS CONDITIONS
(i) Impacted Wax or Cerumen. The outer third hair-bearing canal skin is lined by the sebaceous glands and the modified apocrine ceruminous glands. The sebaceous glands secretes an oily material (sebum) from the breakdown of their fat-containing cells, while ceruminous glands secretes fluid (cerumen) rich in lipids and pigment granules which are commonly excreted in the base of the hair follicles. The mixture of desquamated cells, cerumen, sebum, shed hair, keratin and dirt forms wax.
There are two types of human ear wax, wet and dry forms. Dry wax lacks cerumen and it usually yellow or grey in colour and hard in consistency, on the other hand wet wax is brown in colour and soft and sticky in consistency.
Wax is protective in nature and its functions are
- Lubricates and cleans the canal.
- Traps dirt and microbes by virtue of its antimicrobial properties.
- Bacteriostatic and fungistatic due to its acidic ph.
Normally, there is a self-cleaning action of ear canal, dry wax migrates down the hair and moves out of the ear canal by movements of the jaw. Certain other factors like narrow and tortuous ear canal, stiff hair or obstructive lesion of the canal, e.g. exostosis, may favour retention of wax. It may dry up and form a hard impacted mass.
Clinical features.
Usually there is wax plugs present, occluding the ear canal which is sometimes incidental, symptomless finding. Patient presents with sense of heaviness and blocked ear associated with decreased hearing. Complete occlusion of the ear canal may lead to a hearing loss upto 40 dB. Other common symptoms are itching, earache, tinnitus and cough. Granuloma (wax granuloma) can form due to ulceration of impacted wax present for a long time.
Indications for wax removal includes ear symptoms which need examination of ear canal or tympanic membrane, such as ear discharge, otalgia and hearing loss.
Treatment
- Wax softening agents. In young children or if there is hard impacted wax, softening agents like 5% sodium bicarbonate, olive oil, hydrogen peroxide, liquid paraffin and commercial agents such as 2% paradichlorobenzene are frequently used to helps wax removal by syringing or instruments.
- Syringing and irrigation method. It is the most common procedure used for wax removal in clinical setting. Syringe containing water at body temperature is directed along the postero-superior wall of the meatus. Pressure of water deep to wax expels wax out of the canal. Mopping is done with cotton pledget following the procedure to make ear dry. It is performed after taking a complete history (past history of ear discharge or an existing perforation) and ear examination. Patient may complain of intense pain and giddiness. Contraindications are otitis externa, history of ear discharge, temporal bone fracture, Vegetable foreign body and uncooperative patients especially young children.Complications of syringing are traumatic perforation, vasovagal attack, Impaction of foreign body, vertigo because stimulation of labyrinth
- Removal under direct vision. It is done with the aid of a headlight, microscope or endoscope, with ear probes or suction tips. It also helps in wax removal from attic and open mastoid cavities.
Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear Diseases of External Ear
———— End of the chapter ————
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Susan Standring, Gray’s Anatomy.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
