Impedance Audiometry. Impedance audiometry is an objective test used to assess middle ear function and mobility of the tympanic membrane. The word ‘impedance’ means resistance to the flow of acoustic energy, expressed in ohms. and compliance is expressed in cubic centimetre of air. It provides valuable otological and neurological information about the nature and site of a lesion. The middle ear functions as the ‘impedance matching device’. Any pathology in the middle ear may cause impedance mismatching and vary the amount of sound reflected back from the tympanic membrane leading to conductive deafness. Impedance audiometry measures the efficiency of the middle ear to perform this function.
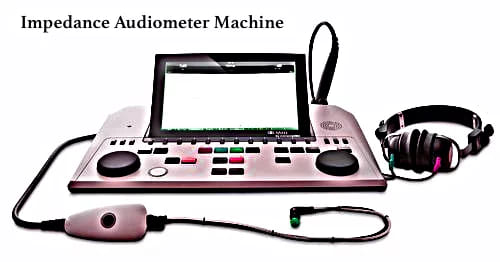
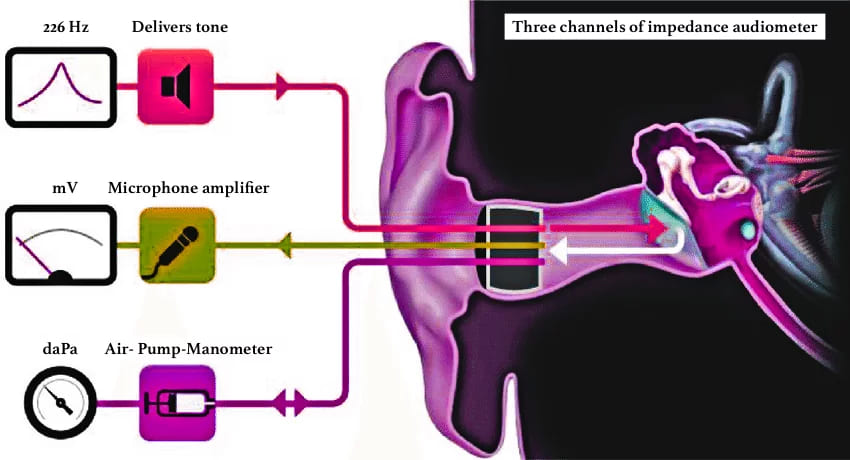
Impedance audiometer consists of a handheld probe which is hermetically sealed into the external auditory meatus forming a leak-free seal from the probe tip to the eardrum and has three channels: (i) first channel delivers a tone of 220 or 226 Hz, (ii) the second channel allows the reflected sound from the tympanic membrane to pass through a microphone amplifier assembly for processing (iii) the third channel is attached to air- pump-manometer system to bring about changes in air pressure in the ear canal from positive to normal and then negative(+300 to -600 mm of water pressure).
It includes:
(i) Tympanometry
(ii) Eustachian tube function test
(iii) Acoustic/ stapedial reflex measurements
(i) TYMPANOMETRY. (one of the acoustic immittance tests) is the measurement of the change of impedance in the middle ear due to varying air pressure in the sealed external auditory meatus. A non-compliant/ stiff tympanic membrane tends to reflect back more sound energy as compared to a compliant TM. This reflected sound pressure is measured at the tip of the probe and charted in the graphical form of with impedance of the middle ear/compliance of TM on Y-axis and the air pressure on X-axis, called the tympanogram.
Impedance Audiometry. Impedance Audiometry. Impedance Audiometry. Impedance Audiometry. Impedance Audiometry. Impedance Audiometry. Impedance Audiometry. Impedance Audiometry.
| Impedance is the opposition/ resistance to the flow of energy, admittance is the ease of movement with which the flow of energy occurs. For ease of measurement most clinical impedance audiometers measure the acoustic admittance. Admittance is reciprocal of impedance just like compliance is the reciprocal of stiffness. |
Procedure:
1. Otoscopy is done to exclude scarring or perforation in the tympanic membrane
2. Remove wax /discharge, if present and choose a well-fitted ear probe tip to create an air tight seal.
3. Mild sedation may be used in un-cooperative patients and children.
4. A probe is inserted in the ear. Increase the pressure to +200 mm of H2O. Reduce the pressure serially to 100, 50, 0 up to 400 mm of H2O to test the compliance at various pressure. Draw a graph with pressure on the X-axis and compliance on the Y-axis. The normal middle ear pressure is ± 25 mm of H2O but for practical purposes ± 100 mm of H2O is taken as normal.
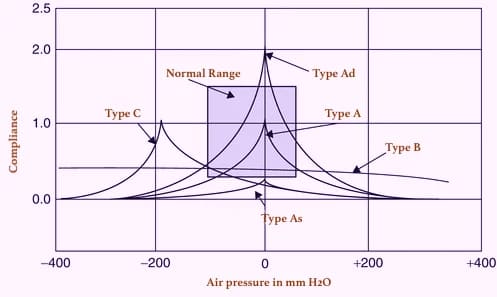
Types of tympanogram:
| Type A | Normal tympanogram (the peak is near zero pressure) |
| Type As | Compliance is lower at or near ambient air (zero) pressure. Hypo-mobile admittance is observed in otosclerosis, tympanosclerosis or malleus fixation. |
| Type Ad | High compliance at or near ambient pressure. Hypermobile admittance is observed in discontinuity of ossicular chain or thin, flaccid tympanic membrane. |
| Type B | A flat or dome-shaped graph. No change is seen in compliance with changes in pressure. This curve is seen in middle ear fluid, adhesive otitis media, thick or perforated TM, or grommet in situ. |
| Type C | Maximum compliance occurs with negative pressure in excess of 100 mm H2O. Seen in retracted tympanic membrane, fluid in middle ear. |
| Type D | A notched graph, seen in scarred and flaccid TM |
| Type E | An undulating graph, seen when 8000 Hz sound is presented . This is seen in thick grafts after myringoplasty or in any mass. |
(ii) EUSTACHIAN TUBE (ET) FUNCTION TEST. Tympanometry can be used to assess eustachian tube function and confirm the integrity of the auditory system. Eustachian tube dysfunction plays a dominant role in the pathogenesis of suppurative and non-suppurative otitis media. The prognosis and treatment of both types of otitis media are dependent upon the eustachian tube function. Tests which can be done are: (a) William’s test (b) Toynbee’s test (c) Acoustic immittance.
(a) William’s test. is done in an intact tympanic membrane. The impedance audiometer is programmed to measure the middle ear pressure in three conditions (i) the middle ear pressure at the beginning of the test (resting pressure), (ii) after swallowing (with the nose pinched and mouth closed) and (iii) after performing Valsalva.
Inference:
- Normal ET function: Middle ear pressure is same as atmospheric pressure at rest, during swallowing or Valsalva.
- Impaired ET function: Pressure becomes negative during swallowing. It does not become positive on Valsalva or vice versa.
- Grossly impaired ET function. Pressure does not change at all in either of the situations.
(b) Toynbee’s test. is done in patients having a perforation in the tympanic membrane or grommet-in -situ. The test is similar to William’s test where negative or positive pressure (−250 or +250 mm H2O) is created in the middle ear and the person is asked to swallow five times in 20 seconds. The test is carried out for a fixed duration of time, e.g., 40 seconds (minimum) or 160 seconds (maximum). The ability to equilibrate the pressure with every act of swallowing indicates whether the patient is having normal tubal function or not.
(c) Acoustic immittance can also measure the physical volume of air between the probe tip and the tympanic membrane. Normally it is up to 1.0 mL in children and 2 mL in adults. Any increase in volume >2 mL in children and >2.5 mL in adults indicate perforation of the tympanic membrane (because middle ear volume is added up to the volume of the external ear canal). This has also been used to find patency of the ventilation tube.
(iii) ACOUSTIC REFLEX. is based on the fact that a loud sound 70–100 dB above hearing threshold of one ear, causes bilateral contraction of the stapedius muscle (which pulls the stapes slightly outward and upward) & and tensor tympani muscle (pulls the tympanic membrane slightly inward). The effect is more pronounced on the stapedius muscle than on tensor tympani. Stapedial reflex threshold (SRT): Minimal intensity of sound that produces stapedial reflex. (bilateral reflex)
Reflex arc:
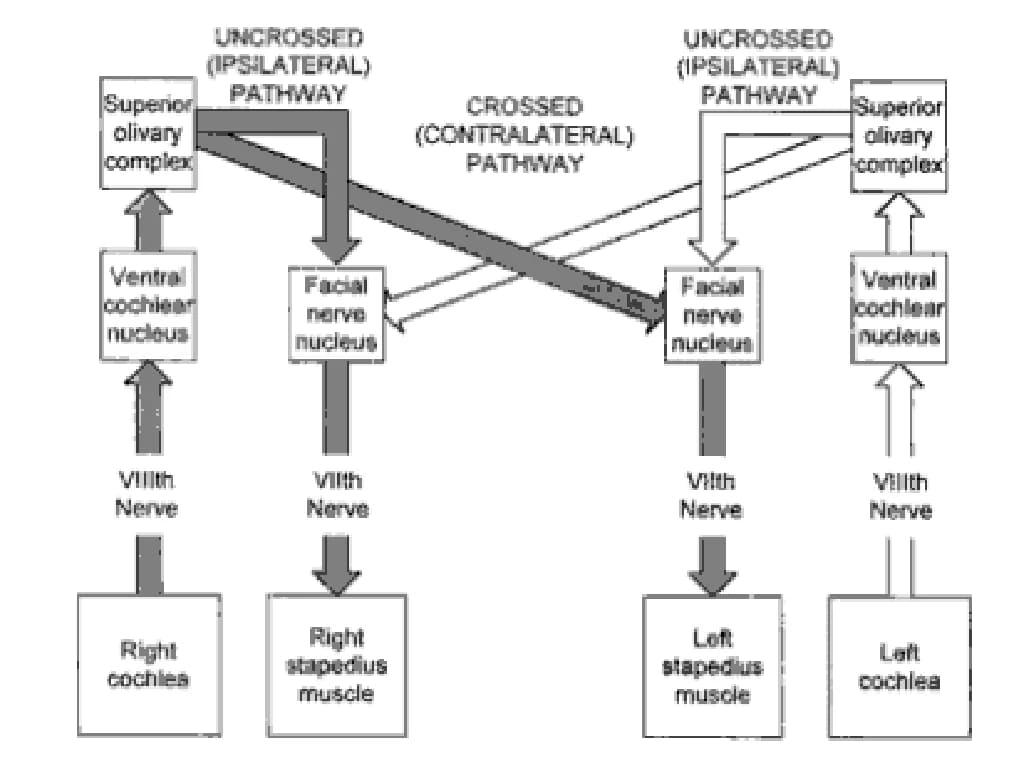
Ipsilateral ear: CN VIII → ventral cochlear nucleus → CN VII nucleus → ipsilateral stapedius muscle.
Contralateral ear: CN VIII → ventral cochlear nucleus → contralateral medial superior olivary nucleus → contralateral CN VII nucleus → contralateral stapedius muscle
Uses of acoustic reflex: It is very simple to perform, requires a few minutes, is a non-invasive objective test (does not depend upon subjective responses from the patient)
Acoustic reflex tests help the otolaryngologist/neurologist :
- To test the hearing in infants, young children and uncooperative patients.
- To assess middle ear function accurately.
- To differentiate cochlear and retro-cochlear pathology. In cochlear lesion, the stapedial reflex is present at lower intensities, e.g. 40–60 dB than the usual 70 dB(recruitment phenomenon)
- To detect brain-stem pathologies: If ipsilateral reflex is present but the contralateral reflex is absent, the lesion is in the area of crossed pathways in the brainstem.
- To detection non-organic hearing loss: A malingerer does not give any response on pure tone audiometry but shows a positive stapedial reflex.
- To identify the level of lesion in facial nerve paralysis: Absence of stapedial reflex when hearing is normal indicates a lesion of the facial nerve, proximal to the nerve to stapedius. The reflex can also be used to find prognosis of facial paralysis as the appearance of reflex after it was absent, indicates return of function and a favourable prognosis.
- To detect VIIIth nerve lesion: If a sustained tone of 500 or 1000 Hz, delivered 10 dB above acoustic reflex threshold, for a period of 10 s, brings the reflex amplitude to 50%, it shows abnormal adaptation and is indicative of VIIIth nerve lesion (stapedial reflex decay).
——— End of the chapter ———
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Ganong’s Review of Medical Physiology.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
