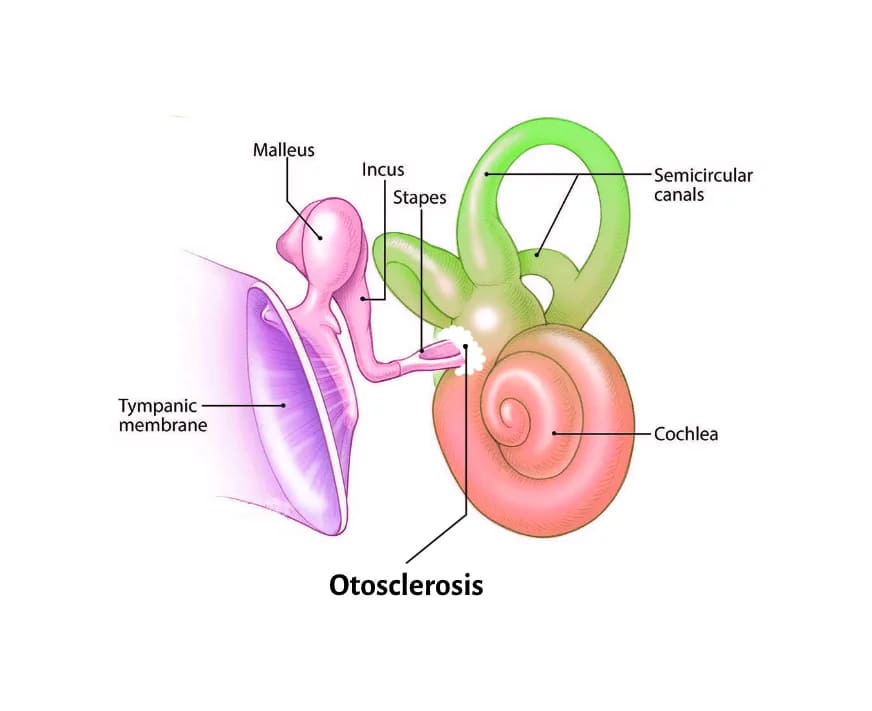
OTOSCLEROSIS Synonym: OTOSPONGIOSIS. In this, there is an osseus dyscrasia (disorder of bone metabolism) where in, normally dense enchondral layer of bony labyrinth is replaced by foci of irregularly laid spongy bone. Remodelling at stapedio-vestibular joint leads to stapes fixation and conductive deafness. When bone remodelling encroaches upto the cochlea, sensorineural hearing loss can occur.
HISTOPATHOLOGY
The bony labyrinth exhibits property of limited remodelling. There is laminar bone resorption by osteoclasts where as there is deposition of new spongy bone of greater thickness, vascularity and cellularity by osteoblasts. The bone turnover is dependent on the ratio of two cytokines factors – osteoprotegerin (OPG) and Receptor activator nuclear kb ligand (RANKL).
OPG is an inhibitor of osteoclast maturation and functions in competition with RANKL (an activator) for the osteoclast RANK receptor.
FINDINGS UNDER LIGHT AND ELECTRON MICROSCOPY:
Grossly, otosclerotic lesion appears chalky white, yellow greyish or it may be red in colour due to increased vascularity.
Microscopically, the lesion is classified as “active”and “inactive”depending on the stage of bone turn over.
- Active lesions are characterized by spongiotic, immature osseous tissue with many dilated vascular channels and osteoclastic giant cells.
- Inactive lesions are characterized by solid, compact, lamellar, sclerotic bone containing tiny marrow spaces and small infrequent blood vessels.
- Blue mantles are remodelled hypercellular bone and cement substance which stains blue with haematoxylin-eosin stain.
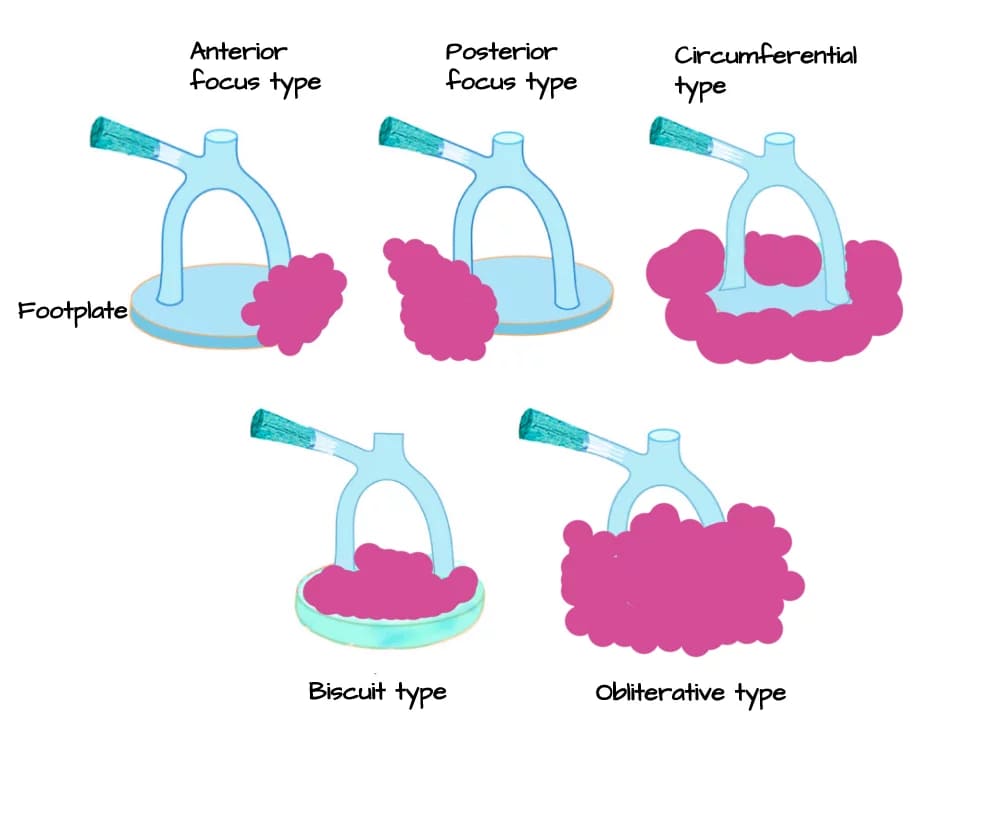
| Depending on the amount of otosclerotic bone deposition in the region of the footplate of stapes, they are divided into: Type I: Less than half of the footplate is involved and normal thin bluish appearance of the footplate is retained. Type II: More than half of the footplate is involved with thickening of the footplate. Type III: Whole of the footplate is involved and appears thickened. The margin of the footplate can be identified. Type IV: Otosclerotic bone is deposited in the entire footplate obliterating the oval and/or round window. |
ETIOLOGY
Otosclerosis is idiopathic; however, these causes have been hypothesised.
- Genetic predisposition: Positive family history is reported in 50% cases. It is an autosomal dominant trait. Several genes encoding for cytokines is linked with otosclerosis – TGFb1 and bone morphogenetic protein.
- Viral infection: Studies have shown low levels of anti-measles virus IgG in serum, and higher levels in perilymph. Considering the histological similarity between otosclerosis and Paget’s disease, it is more likely that otosclerosis is also a viral disease as has been suggested for Paget’s disease.
- Autoimmune : Elevated circulating antibodies against Type 2 collagen and Type 9 collagen are seen in blood of the otosclerotic patient.
- Anatomical basis : The sites of predilection for bone remodelling are –fissula ante fenestram lying anterior (front) to the oval window and fissula post fenestram lying posterior (behind) to oval window. Other areas affected in stapedial otosclerosis are stapes footplate (circumferential), in the footplate but annular ligament free to move (biscuit type), oval window niche (obliterative type). Area around round window is involved in cochlear otosclerosis.
- Gender: Otosclerosis predominates in females in India.
- Age of onset: Hearing loss starts between 20 and 30 years of age.
- Van der Hoeve syndrome: It is triad of symptoms of osteogenesis imperfecta, otosclerosis and blue sclera due to genes encoding type I collagen.
- Hormonal: Otosclerosis may be worsened by pregnancy, puberty and during menopause.
TYPES OF OTOSCLEROSIS
- Stapedial/ Clinical Otosclerosis. It affects stapes, stapedio-vestibular joint causing conductive deafness.
- Cochlear Otosclerosis. It involves cochlear endosteum without affecting the stapes or the stapedio-vestibular joint causing pure sensorineural hearing loss with no conductive element.
- Histologic Otosclerosis. It does not affect the stapes or the stapedio-vestibular joint and cochlear endosteum hence remain asymptomatic throughout life. Lesion is detected only on post-mortem. It is a gold standard for reporting of incidence.
Types of stapedial otosclerosis
SYMPTOMS
- Hearing Loss: There is slow onset, painless, progressive hearing loss in early adulthood. It may be conductive, sensorineural or mixed. Conductive hearing loss is due to ankylosis/ narrowing of annular ligament especially posterior part, full obliteration of round window niche, cavitating otosclerosis (third window effect) and malleus fixation. Sensorineural hearing loss is due to the entry of toxic materials in the inner ear. The endosteum of bony labyrinth is involved leading to atrophy and hyalinization of spiral ligament. It is a rare type. Paracusis willisii : It is feature seen in otosclerosis. The patient has a sensation that he hears more easily in noisy surroundings than in a quiet surroundings. It is because the other person tends to raise his voice in noisy surroundings.
- Vertigo: It is caused may be due to co-existing Meniere’s disease. However, vertigo to loud noises and Valsalva’s manoeuvre suggests ‘third window lesions’ (superior semi-circular canal dehiscence).
- Speech: Voice is soft and well-modulated because bone conduction is more and patient hears his own voice louder.
- Tinnitus : It is seen more in cochlear otosclerosis and when lesions are active.
SIGNS

Investigations
- Otoscopy : Normal and mobile tympanic membrane. A congested area/ red blush may be seen on the promontory through the tympanic membrane (Schwartze sign/ flamingo flush).
- Rinne test negative (i.e. BC >AC) first for 256 Hz and then 512 Hz and still later, when stapes fixation is complete, for 1026 Hz.
- Weber test is lateralized to the worst ear.
- Absolute bone conduction is normal in stapedial but decreased in cochlear otosclerosis.
- Gelle’s test is negative in fixed stapes footplate.
- Pure tone audiometry shows conductive type of hearing loss, more for lower frequencies. Air– bone gap is greatest at 0.5, 1 and 2kHz frequencies. Bone conduction is usually normal but sometimes carhart notch is seen. Carhart notch was first described in otosclerosis, but it occurs in all ears that have a conductive hearing loss. There is a dip in bone conduction curve and it is different at different frequencies but maximum at 2000 Hz. (e.g. 5 dB at 500 Hz, 10 dB at 1000 Hz, 15 dB at 2000 Hz and 5 dB at 4000 Hz).
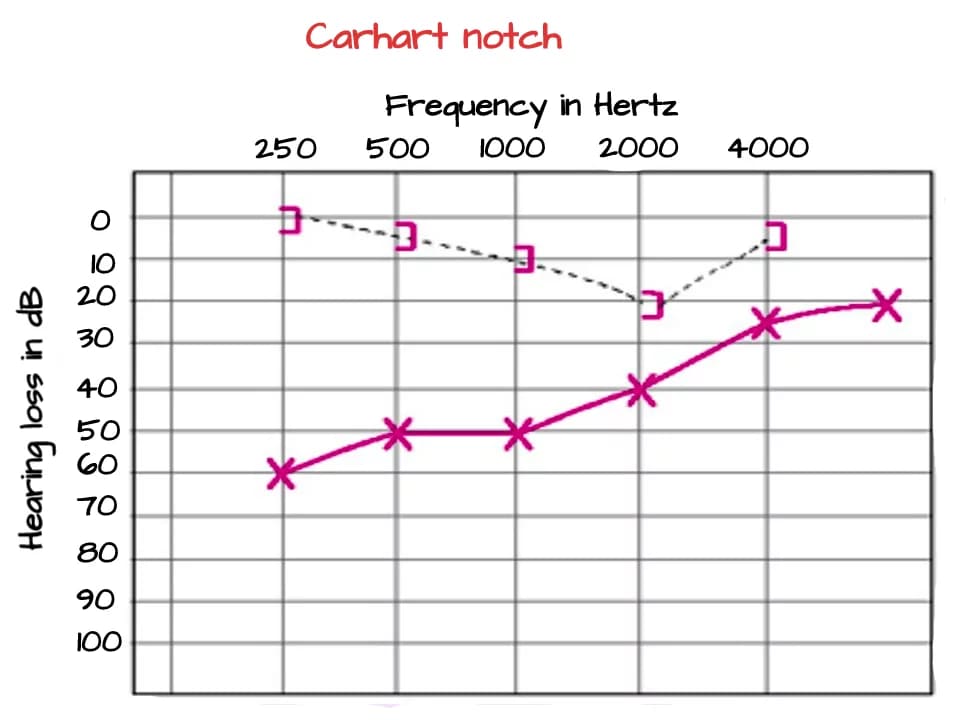
Reason of Carhart notch: When the skull is vibrated by bone conduction sound, the sound is detected by the cochlea via three routes.
- Route 1 is by direct vibration within the skull.
- Route 2 is by vibration of the ossicular chain, which is suspended within the skull.
- Route 3 is by vibrations emanating into the external auditory canal as sound and being heard by the normal air-conduction route.
In patient having conductive hearing impairment the latter two routes are deficient causing notch. Bone conduction is artificially reduced by 5–15dB. Carhart effect is greatest around 2kHz frequency, which is near the resonant frequency of the ossicular chain. Bone-conduction thresholds improve following successful reconstruction surgery.
| Carhart Notch is commonly attributed to: Loss of inertial component of bone conduction by stapes fixation. Fixation of stapes disrupts normal ossicular resonance, happening at about 2000 Hz. Relative perilymph immobility due to stapes fixation disturbs the normal compressional mode of bone conduction. Cookie bite pattern may be rarely seen in mixed hearing loss. |
7. Speech audiometry: Normal discrimination score except in cochlear otosclerosis.
8. Tympanometry: May be required to rule out Otitis media with effusion. Stapedial reflex is absent in case of fixed stapes.
9. High resolution CT scan of temporal bone is able to detect abnormal bone densities within the bony labyrinth.
Classic double ring sign: Oval window margins are ill-defined, narrowed and later oval window opening and niche gets obliterated. This sign is seen in cochlear otospongiosis.
TREATMENT
A. MEDICAL
(i) Oral Fluorides. 40 mg sodium fluoride, 500mg of calcium gluconate and 400 units of vitamin D every day for 12-24 months can be considered in otosclerosis patients with progressive sensory hearing loss .
(ii) Third generation bisphosponates. It reduces bone remodelling and the rate of sensory hearing loss in patients with cochlear otosclerosis.
B. HEARING AIDS.
(i) Patients who refuse surgery or are unfit for surgery may use conventional hearing aids.
(ii) Far Advanced Otosclerosis (FAO): Patients with air conduction over 85dB and unmeasurable bone conduction are not benefitted fully by air-conduction hearing aids alone and require stapedectomy and conventional hearing aids, cochlear implantation or new direct acoustic cochlear stimulation (DACS) device.
(iii) Bone- anchored hearing aid is used in patient whose ‘only hearing ear’ gets otosclerosis or the patient having post- fenestration cavity not benefitted by conventional hearing aids. This aid is risk free as it does not cause a dead ear.
(iv) Direct acoustic cochlear stimulation (DACS) device may be used inpatients with mixed hearing loss where stapedotomy is not sufficient. The device consists of an active middle ear implant attached to a stapes prosthesis.
(v) Cochlear implantation. can be done in Far Advanced Otosclerosis or after failed stapedotomy.
Pitfalls of cochlear implantation in otosclerosis are as a result of previous otosclerosis surgery, which are:
- Incus subluxation
- Middle ear adhesions
- Tympanic membrane vulnerable at site of bony curettage
- Ossification of Scala tympani from post-stapedectomy labyrinthitis
- As a result of disease process
- Obliteration of round window by spongiotic bone
- Incomplete electrode placement
- ‘Looping’ of electrode through soft spongiotic bone in cochlea
- Facial nerve stimulation by placement of electrodes in cochlea
C. STAPES SURGERY
- Stapedectomy – The fixed, otosclerotic stapes is removed and a prosthesis (made of teflon piston, stainless steel piston, platinum–teflon or titanium–teflon piston) is inserted between incus and oval window.
- Vein graft teflon interposition operation.
- Laser stapedotomy.
- Stapedotomy with stapedius tendon preservation.
STAPEDECTOMY
Selection of patient for stapes surgery:
- Socially handicapped (Hearing threshold for air conduction 30 dB or worse).
- Average air-bone gap at least 15 dB with Rinne negative for 256 and 512 Hz.
- Speech discrimination score 60% or more.
Contraindications of stapes surgery:
- Otosclerosis in the only hearing ear.
- Age > 70 years.
- Young children- Recurrent eustachian tube dysfunction may displace the prosthesis or cause acute otitis media.
- Sportspersons, snorkelling, parachuting, construction workers at high altitudes, scuba divers and frequent air travellers have risk of postoperative vertigo.
- Patients having occupational noise exposure are susceptible to get sensorineural hearing loss after surgery.
- Pregnancy
Relative contraindications:
- Diabetes, active otosclerosis and eustachian tube dysfunction.
- Active infection in outer or middle ear, tympanic membrane perforation and exostosis
Steps of Stapedectomy: The surgery is preferably done under local anaesthesia
- An incision is given in the meatus to elevate tympano-meatal flap.
- Expose stapes area (tympanotomy).
- Incudostapedial joint is mobilized/ divided.
- Divide stapedius tendon with a laser/ scissors or microhook.
- Remove stapes superstructure by fracturing the crura down, away from the facial nerve, however, it is better to first divide the posterior crus with a laser/crurotomy scissors to reduce the risk of mobilizing the footplate.
- Measure the distance between the footplate and the incus. Prosthesis selected to be 0.25 mm longer than the distance from the underside of the incus to the footplate.
- Create a hole with a laser/ electrical microdrill in posterior third of the footplate (stapedotomy) or removal of a part of footplate (stapedectomy). The perforation must be slightly wider than the prosthesis. If a 0.4 mm prosthesis is being used, a perforation is approximately 0.5–0.6 mm.
- Place the prosthesis.
- Reposition the tympanomeatal flap.
Complications of stapes surgery:
- Postoperative conductive hearing loss. There are three main causes. Displacement of short or loose prosthesis by Valsalva or sneezing (incorrect measurement of prosthesis.), Later on Incus erosion may be seen, Bony regrowth over the fenestration.
- Sensorineural hearing loss. Perioperative SNHL causes – Surgical trauma, drilling due to obliterative otosclerosis, floating footplate or perilymph aspiration. Delayed SNHL causes – Barotauma (air travel), Labyrinthitis, Perilymph fistula, reparative granuloma.
- Facial nerve injury arising from local anaesthetic infiltration or nerve over-heated by drill during surgery.
- Vertigo may occur in first week of post-operative period (serous labyrinthitis).
- Incus dislocation. During post-operative period (due to intraoperative trauma, serous labyrinthitis, long prosthesis). Incus dislocation may occur as a late complication also due to perilymph fistula and benign paroxysmal positional vertigo.
- Dysgeusia, xerostomia and soreness of the tongue due to injury to chorda tympani
- Dead ear: The patient may not hear at all due to reparative granuloma formed after stapedotomy.
———— End of the chapter ————
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Susan Standring, Gray’s Anatomy.
- Ganong’s Review of Medical Physiology.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
