SYNONYM: Idiopathic Endolymphatic Hydrops/ Labyrinthine Hydrops. Meniere’s disease is an idiopathic disorder of membranous labyrinth of inner ear. It was first described by a French doctor, Prosper Meneire.
Endolymphatic hydrops means raised hydraulic pressure in the endolymphatic system causing a tetrad of symptoms (i) recurrent, spontaneous episodic vertigo (ii) fluctuating or progressive sensorineural deafness (iii) tinnitus (low tone roaring sound) and (iv) fullness or heaviness in ear. Meniere’s disease is often preceded by aural fullness and associated with nausea and vomiting.
MÉNIÈRE DISEASE V/S MÉNIÈRE SYNDROME
Ménière’s disease is idiopathic, on the other hand, Ménière syndrome occurs secondary to autoimmune dysfunction, endocrine disorders, syphilis, trauma, electrolyte imbalance, parasitic infections, (various processes interfering with normal production or resorption of endolymph). This distinction in nomenclature is analogous to Bell’s palsy. If the source of facial paralysis is known, Bell’s palsy is not the diagnosis. Similarly, when the cause of vertigo is known, Ménière disease is not the diagnosis.
ETIOLOGY
Ménière disease is idiopathic, by definition. Ménière syndrome occurs secondary to following disorders :
- Autoimmune: Meniere disease is seen in a few patients with lupus and rheumatoid arthritis
- Genetic: Though most cases are sporadic, 5–15% are reported to be familial have autosomal dominant pattern of inheritance.
- Viral infections: A few patients were benefitted by acyclovir therapy suggesting Herpes simplex virus as one of the etiology.
- Allergy: Food triggers may worsen symptoms. Presence of IgG and IgA in cells of endolymphatic sac supports this hypothesis.
- Sympathetic overactivity leads to spasm of internal auditory artery producing deafness and vertigo.
- Hypothyroidism: 4% cases of Ménière’s disease are due to hypothyroidism requiring thyroid replacement therapy.
- Endolymphatic Hydrops secondary to otic capsule disease like congenital or acquired syphilis, otosclerosis, Paget’s disease and post-stapedectomy cases.
- Exclude. Transient ischemic attacks, endolymphatic sac tumour, vestibular schwannoma, vestibular migraine, vestibular paroxysmia, recurrent unilateral vestibulopathy.
PATHOPHYSIOLOGY:
The underlying pathology in Meniere’s disease is excessive fluid collection in the endolymphatic system due to:
- Excessive endolymph production (Endolymph is secreted by stria vascularis)
- Reduced absorption of endolymph in the endolymphatic sac (Endolymph is carried via endolymphatic duct to endolymphatic sac where it is absorbed)
- Both above causes.
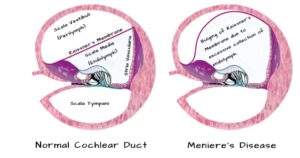
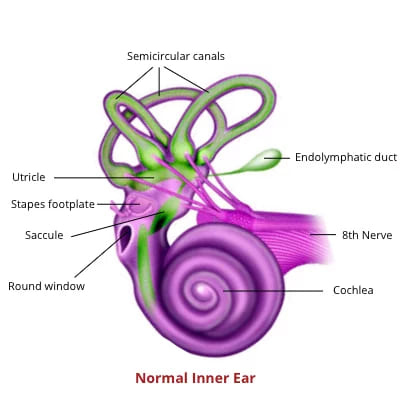
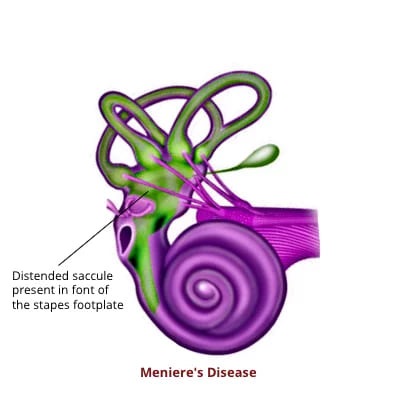
| Raised endolymphatic pressure. ↓ Dilated cochlear duct may fills the scala vestibuli ↓ Bulged Reissner’s membrane herniates through helicotrema into the apical part of scala tympani ↓ Rupture of the membrane that separates perilymph (low potassium extracellular fluid) from endolymph (potassium-rich intracellular fluid) ↓ Mixing of fluids ↓ Sudden change in the rate of vestibular nerve firing ↓ Acute vestibular imbalance producing sudden hearing loss & vertigo. ↓ When perilymphatic compartment is restored to normal, symptoms subside. ↓ Aided by the collapse, the rupture heals, and the process is repeated. |
CLINICAL FEATURES
(i) Vertigo: It is sudden, episodic and attack may last for a few minutes to hours with periods of remission lasting for weeks, months or years. The patient feels as if he is rotating, or his environment is moving “up and down” or “to and fro”. Vertigo is associated with nausea, vomiting, ataxia, nystagmus, abdominal cramps, diarrhoea, cold sweats, pallor and bradycardia. However, the patient remains conscious. A few patients have reported warning signs like aural fullness, change in tinnitus character or ear discomfort prior to attack. During periods of remission, the patient may experience hearing loss, sense of imbalance or show no symptoms at all.
Two definitive episodes of vertigo lasting for at least 20 minutes are essential for the diagnosis.
Tullio phenomenon: Attacks of vertigo on hearing loud noise probably due to the distended saccule lying against the stapes footplate. However, this phenomenon is also noticed when there are three functioning windows in the ear, e.g., a fenestration of horizontal canal in the presence of mobile stapes.
Table : Grading of severity of Vertigo
| 0 | No vertigo | – |
| 1 | Mild attack | Brief vertigo < 20 minutes and/or vague sense of disequilibrium lasting < 2 hours. |
| 2 | Moderate attack | Vertigo for 20–60 minutes and/or disequilibrium lasting > 2 hours hampering daily activity. |
| 3 | Severe attack | Vertigo lasting >1hour, associated nausea and vomiting, with or without disequilibrium lasting > 2 hours hampering daily activity. |
| 4 | Extreme attack | Vertigo > 1 hour with nausea, vomiting and severe disequilibrium requiring bed rest throughout day. |
(ii) Fluctuating Hearing Loss. May accompany or precede vertigo. Hearing is usually normal during remission phase. However, with repeated episodes, permanent deafness may be reported. Hearing loss for low frequency sounds is common and music may appear disharmonious. Such patients are unable to tolerate sound amplification due to recruitment phenomenon and are thus poor candidates for hearing aids. A phenomenon diplacusis is seen which implies tone of a particular frequency appearing normal in one ear but of higher pitch in the other ear.
(iii) Tinnitus: low-pitched ocean like roaring or whistling or hissing type. Alteration in intensity and pitch of tinnitus may be the warning symptom of impending vertigo attack.
(iv) Spontaneous Nystagmus:
| Phase | Direction of Nystagmus |
| 1. Irritative phase | Nystagmus beats towards the affected ear in a horizontal /horizontal–torsional direction. |
| 2. Paretic phase | Nystagmus beats away from the affected ear |
| 3. Recovery phase | Nystagmus beats towards the affected side as peripheral vestibular function recovers. |
(v) Age and sex: Peak age is fourth to sixth decade. Males and females show 1:1 preponderance.
CLINICAL EXAMINATION
- Otoscopy findings are normal, but pneumo-otoscopy of the diseased ear may elicit symptoms.
- Nystagmus: The quick component of nystagmus is towards the normal ear.
- Tuning Fork Tests indicate sensorineural hearing loss.
- Weber is lateralized to the better ear.
- Rinne test positive
- Absolute bone conduction reduced in the affected ear.
- Neurologic examination to differentiate Ménière’s disease from other conditions. New-onset vertigo might be an early sign of stroke, migraine, or brainstem compression requiring urgent evaluation.
INVESTIGATIONS
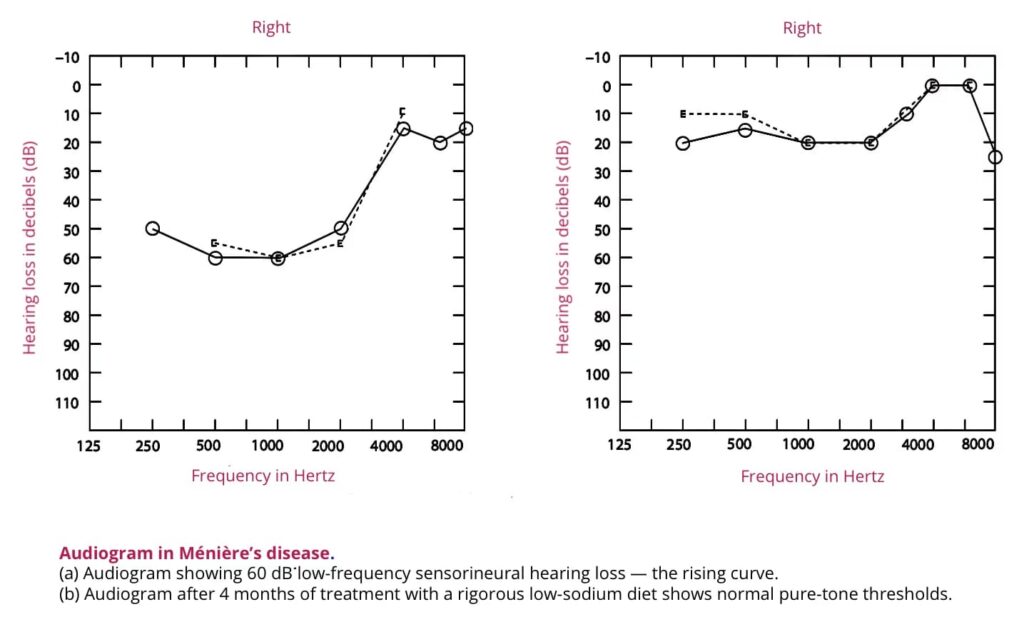
- Pure Tone Audiometry: In early stages, lower frequencies SNHL is recorded, and the curve is of rising type. When higher frequencies are involved, curve becomes tent or falling type later it becomes flat.
2. Speech Audiometry: Speech Discrimination score is 55–85% and discrimination ability is impaired during and immediately following an attack.
Table : Differences between cochlear and retro-cochlear lesion
| Normal | Cochlear lesion | Retrocochlear lesion | |
| Pure tone audiogram | Within normal limits | SNHL | SNHL |
| BERA | Normal interval between wave I & V | Normal interval between wave I & V | Wave V delayed or absent |
| Recruitment | Not present | Present | Not present. |
| SISI score | 0–15% | Over 70% | 0–20% |
| Threshold tone decay test | 0–15 dB | Less than 25 dB | Above 25 dB |
| Speech discrimination score | 90–100% | Below 90% | Very poor |
| Roll over phenomenon | Not present | Not present | Present |
| Stapedial reflex | Present | Present | Not present |
| Stapedial reflex decay | Within normal limits | Within normal limits | Abnormal |
3. Electrocochleography: An electrophysiological test to measure ratio of the summating potential SP (Potential due to basilar membrane movement) and nerve action potential AP through trans-tympanic or extra-tympanic means. In Ménière’s disease, SP/AP ratio is enhanced due to distention of basilar membrane towards scala tympani. (Normally, SP/AP ratio is 30%, it is raised in Ménière’s disease).
4. Caloric Test shows decreased response and a canal paresis on the diseased side in 75% of cases. However, in a few cases, directional preponderance to healthy side or a combination of both canal paresis on the affected side and directional preponderance on the opposite side is reported.
5. Glycerol Test: When given orally, glycerol (1.5 mL/kg- a dehydrating agent ) with an equal amount of water and a lemon juice, reduces endolymph pressure and improves hearing. An improvement of 10 dB in two or more adjacent octaves in audiogram, a gain of 10% in speech discrimination score in 1–2 hrs, improvement in tinnitus and aural fullness after ingestion of glycerol. The test has a diagnostic and prognostic value. These days, glycerol test is combined with electrocochleography.
6. Posterior fossa MRI of the brain should be done to rule out acoustic neuromas or other cerebellopontine angle lesions (in the absence of any contraindications to MRI).
7. Delayed Gadolinium enhanced MRI: I.V. gadolinium contrast given 4 hours prior to MRI or intra-tympanically 24 hours prior to MRI is used as a biomarker to differentiate between perilymphatic and endolymphatic spaces. Gadolinium loads into the perilymphatic space without entering the endolymph in a healthy inner ear.
MÉNIÈRE’S DISEASE VARIANTS
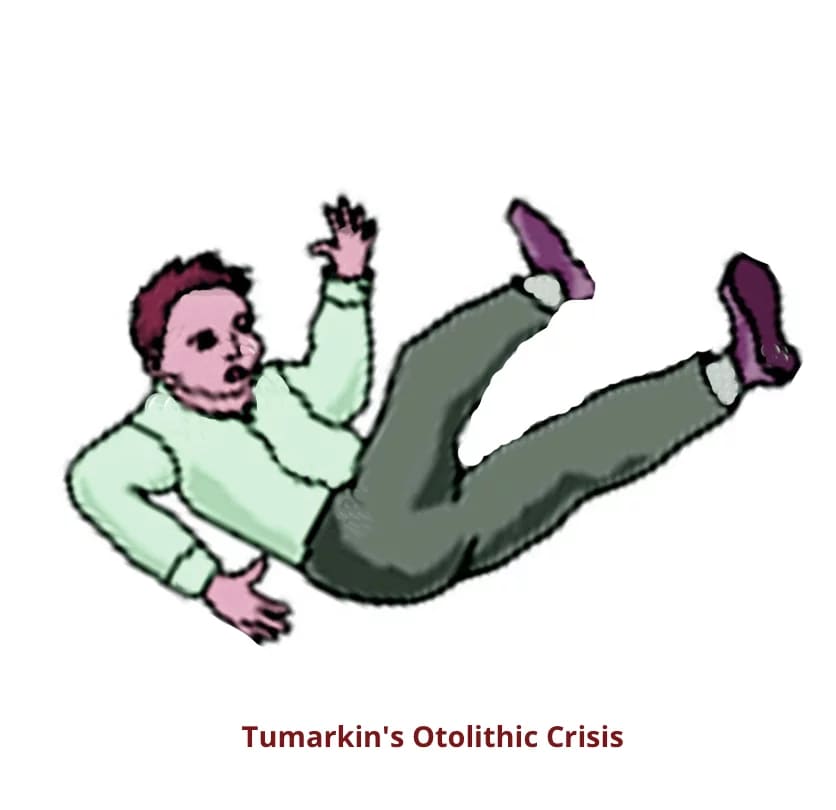
- Tumarkin’s otolithic crisis/ Utricular crisis: The patient gets feeling of being pushed on the ground suddenly without loss of consciousness. There is no vertigo or hearing loss. The underlying mechanism is deformation of the otolithic membrane of the utricle/saccule as a result of changes in the endolymphatic pressure. Treatment: Intratympanic injection of gentamicin
- Cochlear hydrops: Symptoms and signs of only cochlear disease are present because there is block at the level of ductus reunions. Vertigo is not seen.
- Vestibular Hydrops: Patient gets attacks of episodic vertigo while cochlear functions are normal.
- Lermoyez Syndrome: It is Ménière’s disease in reverse order. First hearing starts deteriorating followed by episodes of vertigo.
- Delayed hydrops: caused by viruses, bacteria or spirochaetes.
DIAGNOSIS OF MENIERE’S DISEASE.
The most recent guidelines for the diagnosis of Ménière’s disease were issued in 2015 by the Classification Committee of the Bárány Society, The Japan Society for Equilibrium Research, the European Academy of Otology and Neurotology (EAONO), the Equilibrium Committee of the American Academy of Otolaryngology– Head and Neck Surgery (AAO–HNS) and the Korean Balance Society. It is as follows.
Table : Diagnostic criteria for Meniere’s disease (other causes excluded)
|
Diagnosis |
Criteria |
|
Certain |
Definite Meniere’s disease confirmed by histopathology. |
|
Definite Meniere’s disease |
≥ Two definitive spontaneous episodes of vertigo lasting 20 minutes to 12 hours + Audiometrically documented low- to medium-frequency sensorineural hearing loss in the affected ear on at least one occasion before, during or after one of the episodes of vertigo + Fluctuating aural symptoms (hearing, tinnitus or fullness) in the affected ear. |
|
Probable Meniere’s disease |
≥ Two episodes of vertigo or dizziness, each lasting 20 minutes to 24 hours + Fluctuating aural symptoms (hearing, tinnitus or fullness) in the reported ear |
|
Possible Meniere’s disease |
Meniere’s type episodic vertigo without documented hearing loss, or sensorineural hearing loss, fluctuating or fixed, with vertigo but without definitive episodes. Other causes excluded |
Hearing loss:
The staging system is essential in the diagnosis of certain, definite and probable Meniere’s disease. It is based on the average of pure tone thresholds at 0.5, 1, 2 and 3 kHz (rounded to the nearest whole) of the worst audiogram during 6 months before start of treatment.
Table: Staging of ménière’s disease
|
|
Pure tone average in dB in previous 6 months |
|
1 |
≤25 |
|
2 |
26–40 |
|
3 |
41–70 |
|
4 |
>70 |
TREATMENT
A. GENERAL ADVICE
(i) Relieve patient’s anxiety through relaxation exercises and yoga.
(ii) Smoking Cessation – Nicotine causes vasospasm hence smoking needs to be stopped.
(iii) Dietary restrictions. Patient should take salt-free, caffeine-free diet.
(iv) Avoid activities requiring good equilibrium such as flying, underwater diving or working at great heights.
(v) Avoid stress and excessive drinking of water.
B. MANAGEMENT OF ACUTE ATTACK
(i) Reassurance and complete bed rest with head elevated and minimum movements of head is advised.
(ii) Vestibulosuppressants work by dulling the brain’s response to signals from the inner ear. Drugs used are dimenhydrinate (Dramamine), promethazine theoclate (Avomine) or prochlorperazine (Stemetil) Diazepam (Valium or Calmpose) 5–10 mg i/v to suppresses the activity of medial vestibular nucleus.
C. MANAGEMENT OF CHRONIC PHASE
(i) Vestibulosuppressants and anti-nausea medications Cinnarizine and Prochlorperazine (Stemetil 10 mg TDS orally for two months and after that 5 mg TDS for one month)
(ii) Diuretics. If vestibulo suppressants and vasodilators are not able to improve symptoms, Furosemide, 40 mg tablet, is given on alternate days along with potassium supplement to control recurrent episodes. Thiazide diuretics (hydrochlorothiazide), 12.5 mg daily can also be used.
(iii) Vasodilators. Betahistine (Vertin) 8–16 mg, TDS, given orally, increases labyrinthine blood flow by releasing histamine in the body.
(iv) Microwick- It is a small wick (1 mm × 9 mm) made of polyvinyl acetate meant to deliver drugs from external canal to the inner ear and thus avoid repeated intratympanic injections. A tympanostomy tube (grommet) to be inserted into tympanic membrane and the wick is passed through it. When soaked with a drug, the wick delivers the drug to the round window to be absorbed into the inner ear. It has been used to deliver steroids in sudden deafness and gentamicin to destroy vestibular labyrinth in Ménière’s disease.
(v) Salvage treatment with repeated intratympanic injections of dexamethasoneis indicated when medical treatment fails. In cases refractory to dexamethasone, Inj gentamycin is indicated. This drug is absorbed through round window and is vestibulotoxic (partial chemolabyrinthectomy) Though gentamycin controls vertigo spells in 60–80% of patients but it may cause sensorineural hearing loss as a long-term complication. It is mainly indicated in unilateral meniere’s disease and refractory or end stage cases (tumarkin crisis).
Trans tympanic low-pressure therapy through MENIETT device delivers 3-5 cycles of 0.6 sec pulse at pressure of 0 to 20 cm H2O to the middle ear via grommet for 5 minutes. These pressure waves pass through the perilymph and redistributes endolymph in the endolymphatic sac, blood vessels or communicating channels thereby, reducing pressure and relieving symptoms.
(vi) Allergen elimination: Removal of triggers (food or inhalant allergen) that precipitate attack
D. SURGICAL TREATMENT
(i) Conservative Procedures:
- Endolymphatic sac surgery.
- Endolymphatic sac decompression.
- Endolymphatic shunt to connect endolymphatic sac with subarachnoid space and drain excess endolymph.
- Tenotomy of the tensor tympani and stapedial tendons. The tympanic membrane is pushed laterally by increased cochlear pressure against the ossicular chain. By sectioning the tendon of tensor tympani or stapedius muscle this effect is partially alleviated and ameliorates symptoms.
- Fick’s operation (Sacculotomy) – Distended saccule lies close to stapes footplate and is punctured with a needle footplate. Cody’s tack procedure. Stainless-steel tack is placed in the distended saccule to periodically decompress it. Both these operations are not done now.
- Cochleosacculotomy. Here cochlear duct is punctured with a curved needle is passed through the round window and drained into the perilymph (otic-periotic shunt).
- Ultrasonic destruction of vestibular labyrinth. Cochlear function is preserved.
- Surgical Section of vestibular nerve preserving the facial and cochlear nerve is an alternative to intratympanic injection of gentamicin. It controls vertigo but preserves hearing.
(ii) Destructive procedures. Aim of surgery is to completely destroy cochlear and vestibular function and are thus used only when cochlear function is not serviceable.
a. Labyrinthectomy. Membranous labyrinth is completely destroyed to provide relief from vertigo spells. Routes:
- Through the lateral semi- circular canal by transmastoid route
- Through the oval window by a transcanal approach
b. Laser destruction of inner ear.
———— End of the chapter ————
Anatomy of Temporal Bone Anatomy of Temporal Bone Anatomy of Temporal Bone Anatomy of Temporal Bone Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone
-
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
-
Join our Facebook group: https://www.facebook.com/groups/628414274439500
-
Read chapter Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head and Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat and Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
