ACUTE SUPPURATIVE OTITIS MEDIA. It is a rapid onset, acute (by definition: duration less than 3 weeks) pyogenic inflammation of middle ear cleft, which includes the eustachian tube, middle ear, attic, aditus, antrum and mastoid air cells. Though AOM can occur in all ages, it mainly occurs in children (more common in 6 to 24 months of age) as the Eustachian tube is shorter, wider, more horizontal and flaccid as compared to adults. ASOM, ASOM ASOM, ASOM, ASOM, ASOM, ASOM
Most commonly it is infective in origin, but inflammation can also result from autoimmune, neoplastic, traumatic and metabolic disorders. It normally develops behind an intact tympanic membrane but may include acute infections arising in the presence of ventilation tubes or existing tympanic membrane perforations.
Almost always, acute otitis media include mastoiditis as the middle-ear cavity is in continuity with the mastoid air cells. Acute mastoiditis is differentiated from acute otitis media by abscess formation either within or superficial to the mastoid air cells.

Causative Organisms:
Generally, viral infection of upper respiratory tract precedes the disease but soon the pyogenic organisms invade the middle ear.
- Common viral organisms are respiratory syncytial virus and rhinovirus. While less commonly are coronavirus, influenza type A, adenovirus, and parainfluenza virus.
- Common bacterial organisms in infants and young children are streptococcus pneumoniae (reported in 18–55% of cases), haemophilus influenzae (16-37%) and morexella catarrhalis (11-23%).
- Other organisms in adults are streptococcus pyogenes (13%), staphylococcus aureus (5%) and sometimes pseudomonas aeruginosa.
- Few uncommon are gram-negative bacilli from skin (after trauma) such as bacillus proteus, bacillus pyocyneous and bacillus coli.
- Common fungal organisms are the aspergillus and candida species and mainly it result from superinfection of an initial viral process in immunocompromised individuals.
- In about 18–20%, no growth is seen.
Routes of infection:
1. Via Eustachian tube. It is the most common route. Infection travels via the lumen of the tube or along sub-epithelial peritubal lymphatics. Negative pressure in the middle ear facilitate the movement of bacteria up the Eustachian tube.
2. Via External ear. ASOM normally develops behind an intact tympanic membrane but presence of ventilation tubes or existing tympanic membrane perforations open a route to middle ear infection. It is commonly associated with water exposure.
3. Via Blood-borne route. Blood-borne has been inferred from studies of viral identification in the blood and middle ear. It is an uncommon route.
Predisposing factors:
- Recurrent attacks of common cold, upper respiratory tract infections.
- Infections: Adenoiditis, tonsillitis, rhinitis, sinusitis, pharyngitis. Adenoids serve as a bacterial reservoir in nasopharynx.
- Nasal allergy: Inhalants and foods.
- Palatal disorders: Cleft palate and palatal palsy.
- Feeding bottle in supine position, swimming, forceful blowing of nose & barotrauma.
- Iatrogenic: Postnasal packing and after adenoidectomy.
- Fracture of temporal bone causing injury to middle ear.
- Reduced immunity: Malnourishment, poor dietary habits.
- Exanthematous fevers: Measles, diphtheria, whooping cough.
- Lower socioeconomic group associated with poor housing and overcrowding.
- Familial association. When one family member had AOM, there is increased risk for other family members.
- Maternal blood group A is reported to an independent risk factor.
Pathology and clinical features:
The course of the disease is usually divided into five stages, which begin from stage of eustachian tube occlusion, pre-suppuration, and suppuration and end with either stage of resolution or complications. If appropriate antibiotic therapy is started early in the course of AOM, the disease process may regress from any stage. Regression may also begin without rupture of the TM.
1. Eustachian tube occlusion (Stage 1). Generally, viral infection of the upper respiratory tract precedes the otitis media involving the mucosa of the nose, nasopharynx, middle ear mucosa, and eustachian tubes. Oedema and hyperaemia of nasopharyngeal end of eustachian tube blocks the tube resulting in decrease in ventilation. This leads to a cascade of events resulting in absorption of air and negative pressure in middle ear. There is retraction of the tympanic membrane with some degree of effusion in the middle ear, but the fluid may not be clinically visible.
- Symptoms. Mild hearing loss, Ear fullness, Mild Earache and No fever.
- Signs. There is retraction of tympanic membrane with loss of light reflex. Handle of malleus is more horizontally placed and lateral process of malleus is more prominent. Tuning fork tests shows conductive hearing loss.
2. Pre-suppuration (Stage 2). This stage occurs if the eustachian tube is still not opened because patient is not taking medications or taking inappropriate medications. This results in development of more negative pressure in the middle ear and production of inflammatory exudate from inflamed hyperaemic middle ear mucosa. Due to ineffective drainage from eustachian tube, there is also collection of mucosal secretions. This allows invasion of bacterial and viral organisms in the middle ear but there is still no pus formation in this stage. That is why this stage is called as “stage of pre-suppuration”.
- Symptoms. There is severe throbbing earache which may disturb sleep. There is high grade fever. Hearing loss and tinnitus is present.
- Signs. Tympanic membrane appears red due to congestion giving “cart wheel appearance” (leash of blood vessels along the handle of malleus and at the periphery of TM). There is bulging of tympanic membrane due to collection of exudate and mucosal secretion in the middle ear. Tuning fork tests show conductive hearing loss.
3. Suppuration (Stage 3). In this stage, due to bacterial organisms in the middle ear, there is formation of pus in the middle ear and to some extent in mastoid air cells. It is due to an immunologic response that destroys the offending bacterial organism, culminating in the collection of pus in the middle ear. In the stage of pre-suppuration, there was a bulging of the tympanic membrane, but now in the stage of suppuration, the bulge will reach to the point of rupture. Sometimes a nipple-like protrusion may also be seen in the tympanic membrane with a yellow spot marking the point of rupture.
- Symptoms. There is excruciating earache becomes excruciating. Excruciating ear pain. Increasing deafness. Due to the absorption of toxins, the child develops constitutional symptoms like fever of 102–103 °F, accompanied by with vomiting, diarrhoea and even convulsions.
- Signs. The tympanic membrane appears red and bulging to the point of rupture with loss of landmarks. Handle of malleus is engulfed by the swollen and bulging tympanic membrane. There is tenderness present over the mastoid antrum. There is clouding of air cells in the X-ray mastoid due to the presence of exudates.
Pictures of TM in various stages of ASOM
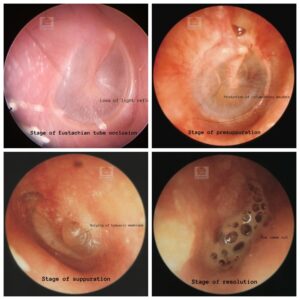
4. Resolution (Stage 4). The tympanic membrane which was at the point of rupture in the stage of suppuration (stage 3), ruptures (due to pressure necrosis) in this stage with the release of pus and there is relief from symptoms. The inflammatory process begins to resolve. If appropriate treatment is started early or if the infection was mild, resolution may start even without rupture of the tympanic membrane.
- Symptoms. With the release of pus, earache is relieved, the fever comes down and the patient feels better.
- Signs. External auditory canal may contain blood-tinged discharge (serosanguinous) which later becomes mucopurulent. The discharge can be pulsatile showing the characteristic “lighthouse effect” (i.e. pus comes out under pressure and synchronises with each arterial pulse). Usually, a small perforation is seen in the anteroinferior quadrant of pars tensa. Hyperaemia of the tympanic membrane begins to subside with the return to normal colour and landmarks.
5. Complications (Stage 5). Usually, AOM is self-limiting in children and subsides well to medical treatment. If the virulence of the organism is high and resistance of the patient is poor, the infection may spread beyond the middle ear boundaries. Complications usually occur in the second week and signs and symptoms reappear. It may lead to acute mastoiditis, subperiosteal abscess, facial paralysis, labyrinthitis, petrositis, extra-dural abscess, meningitis, brain abscess or lateral sinus thrombophlebitis.
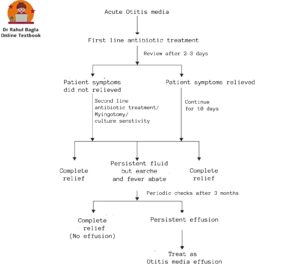
Treatment:
1. Antibacterial therapy. Antibacterial therapy must be continued for a minimum of 10 days, till tympanic membrane regains normal appearance and hearing returns to normal. Inappropriate or inadequate therapy may lead to secretory otitis media and residual hearing loss.
- Amoxicillin – 40 mg/kg/day in three divided doses (first line of antibiotic).
- Cefaclor, Co-trimoxazole or Erythromycin (who are allergic to penicillin’s).
- Amoxicillin clavulanate, Augmentin, Cefuroxime axetil or Cefixime (where β-lactamase-producing h. Influenzae or m. Catarrhalis are isolated).
2. Decongestants. Nasal drops Ephedrine (1% in adults and 0.5% in children) or oxymetazoline (nasivion) or xylometazoline (otrivin) is used to relieve oedema at the nasopharyngeal end of eustachian tube oedema and promote ventilation of middle ear. Oral Pseudoephedrine (sudafed) 30 mg twice daily or a combination of decongestant and antihistaminic (triominic) may achieve the same result without resort to nasal drops which are difficult to administer in children.
3. Analgesics and antipyretics. Paracetamol for relieving pain and fever.
4. Ear toilet. Clean the ear discharge.
5. Dry local heat. Helps to relieve pain.
6. Myringotomy. It is a procedure where incision is made in the tympanic membrane to evacuate fluid or pus from the middle ear. Indications are:
- Drum is bulging and there is acute pain.
- There is an incomplete resolution despite antibiotics when drum remains full with persistent conductive hearing loss.
- There is persistent effusion beyond 12 weeks.
Flowchart of Treatment
———- End of the chapter ———–
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Gordon B. Hughes, Textbook of Clinical Otology.
- Mario Sanna, Textbook of Color Atlas of Endo-Otoscopy.
- Marcos V Goycoolea, Atlas of Otologic Surgery and Magic Otology.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
