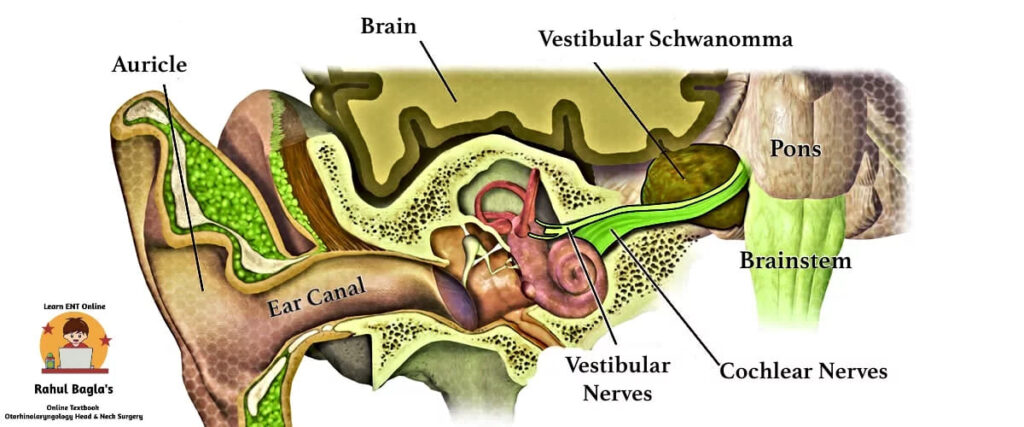
Acoustic neuroma is also known as vestibular schwannoma, neurilemmoma or eighth nerve tumour. It is a benign, encapsulated, extremely slow-growing tumour. Malignant transformation is rare. Vestibular schwannoma accounts for 80-90% of tumours found within the cerebellopontine angle and the remaining 8-10% are meningiomas and epidermoids. CP angle tumours accounts for 10% of total intracranial tumours.
Bilateral CP angle tumors are characteristic for neurofibromatosis 2 (NF2) and are typically vestibular schwannomas. Bilateral tumors not associated with NF2 are facial nerve schwannomas, plexus papillomas, endolymphatic sac tumors, metastases, or osteomas and are rare.
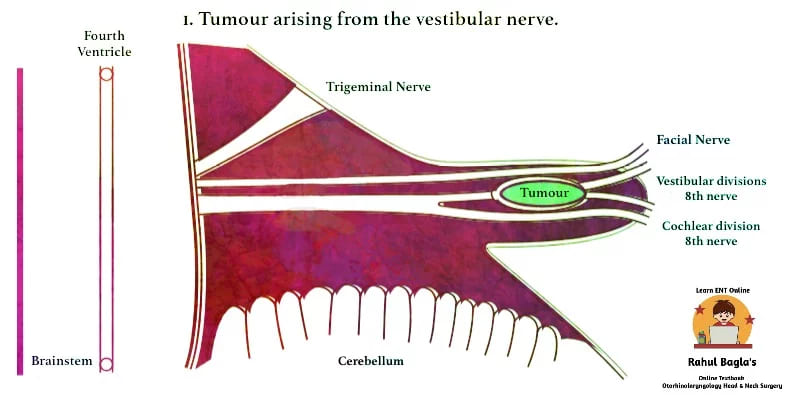
Earlier, in the vestibular nerve, the superior vestibular nerve sheath was regarded as the site of nearly two-thirds of tumours. However, the inferior vestibular nerve is now considered as the predominant site. The term acoustic neuroma is a misnomer as the tumour originates from the sheath of vestibular nerves rather than the neuronal tissue.
ETIOLOGY:
- Idiopathic: Most cases are idiopathic. Incidence is higher in the age group 40-60 years. Both sexes are equally affected.
- Genetic: There is a defect in the gene on chromosome 22q12. Normally, this gene is responsible for control the growth of Schwann cells. It also produces a tumour suppressor protein. Defect leads to the production of abnormally proliferative Schwann cells.
- Environmental: Exposure to high-dose ionising radiations.
PATHOLOGY:
It generally arises from the abnormally proliferative Schwann cells of the vestibular division of the 8th cranial nerve (rarely from cochlear division). Earlier, in the vestibular nerve, the superior vestibular nerve sheath was regarded as the site of nearly two-thirds of tumours. However, the inferior vestibular nerve is now considered as the predominant site. The term acoustic neuroma is a misnomer as the tumour originates from the sheath of vestibular nerves rather than the neuronal tissue.
The most common site of origin is the Obersteiner-Redlich zone (Schwann-glial junction near the Scarpa’s ganglion in the internal auditory meatus). Schwann cells are abundant in this region. As the tumour develops in the nerve sheath, it compresses rather than invades the nerve on which it arises.
| Bill’s bar is named after William House (nickname Dr Bill). It separates the facial nerve from the superior vestibular nerve at the fundus of the IAC. Identification of Bill’s bar allows early identification of the facial nerve. Facial nerve is mostly not involved with pathology (ie, a vestibular schwannoma arising from a vestibular nerve). |
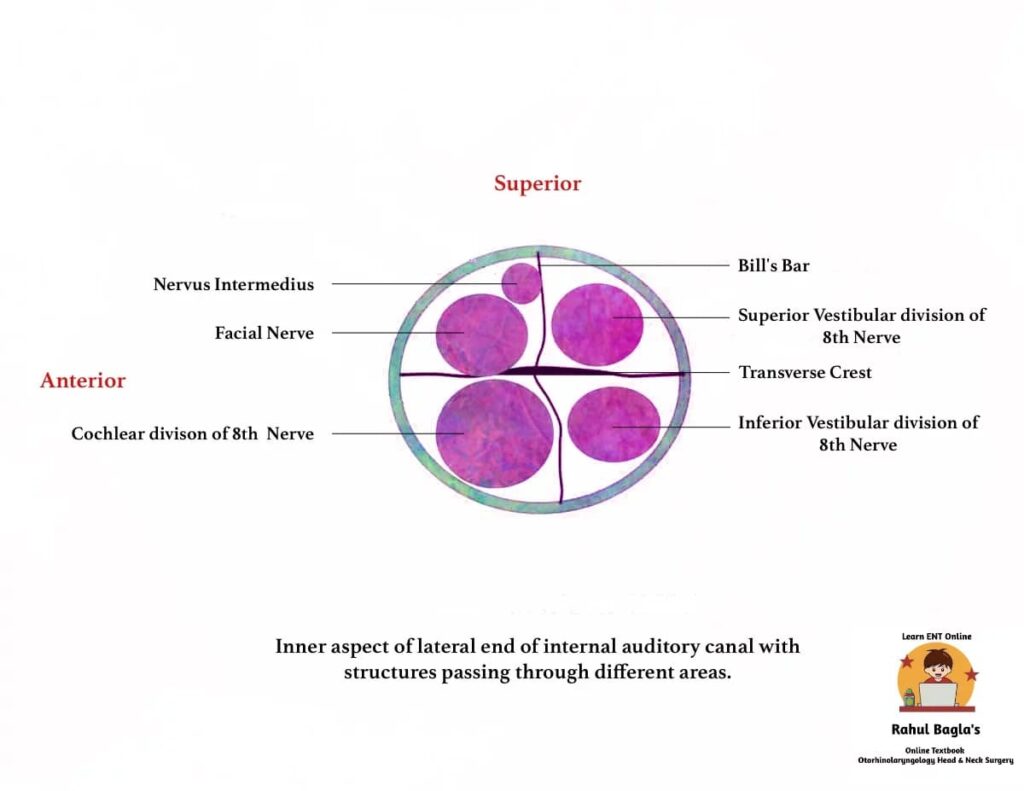
ANATOMY OF INTERNAL AUDITORY CANAL:
On cross-section, the fundus of IAC is divided into four quadrants. It is divided horizontally into superior and inferior by a thin bony septum “crista falciformis” (transverse crest). It is divided vertically into anterior and posterior compartments by Bill’s bar.
Contents:
- Anterior superior quadrant – Motor root of the facial nerve and the nervus intermedius
- Posterior superior quadrant – Superior vestibular nerve
- Anterior inferior quadrant – Cochlear nerve
- Posterior inferior quadrant – Inferior vestibular nerve.
There is a close anatomical relationship between the motor root of the facial nerve, nervus intermedius and vestibulocochlear nerve. This explains the disturbances in lacrimation, taste, salivary flow, hearing, balance or facial motor control that may result from lesions in either the cerebellopontine angle or internal acoustic meatus.
BOUNDARIES OF CEREBELLOPONTINE ANGLE:
It is a triangular potential space located posterior to the pyramid, inferior to the tentorium, lateral to the pons, and ventral to the cerebellum.
ORIGIN AND GROWTH OF TUMOUR
The growth of the tumour is difficult to interpret. It is extremely slow-growing and there may be a history of several years. The growth pattern of the tumour determines the pattern of symptoms. The tumour may grow continuously or only to a certain size, followed by stagnation or even shrinkage.
The patterns of rate of growth are:
- Slow growth: 0.02 cm per year
- Medium growth: 0.20 cm per year
- Fast growth: 1.00 cm per year
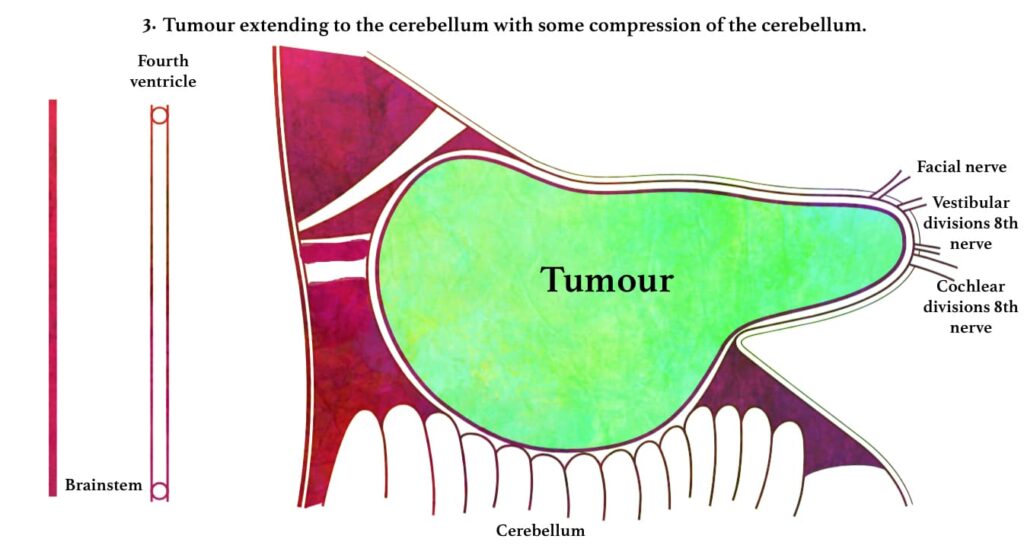
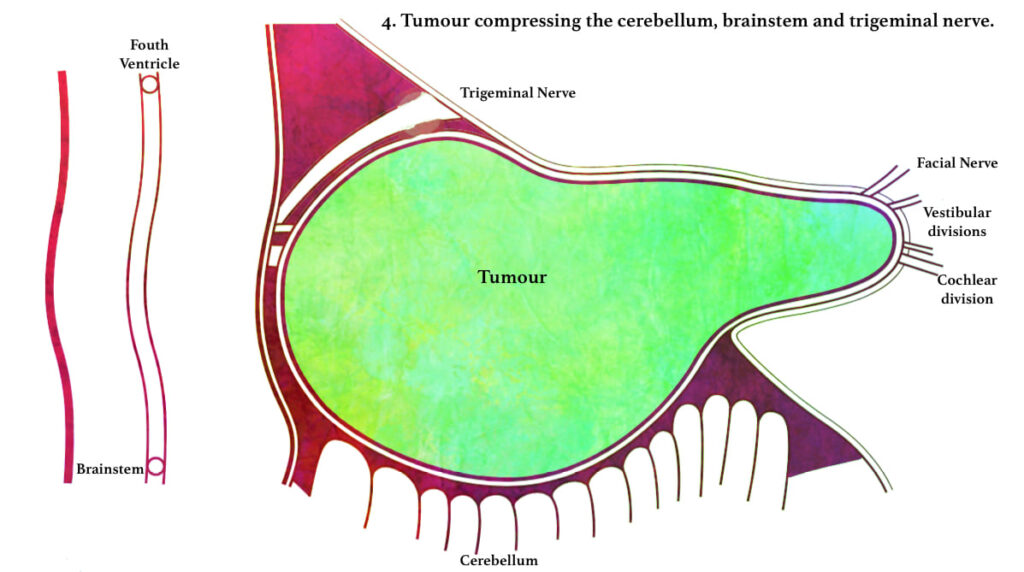
A tumour confined to the internal auditory canal does not produce any symptom. However, as it slowly expands, causes widening and erosion of the canal. Tumour may press on the cochlear, vestibular, facial nerves and the labyrinthine vessels. The tumour may also extend medially into the cerebellopontine angle where, it may grow antero-superiorly to involve Vth nerve or inferiorly to involve the IXth, Xth and XIth cranial nerves.
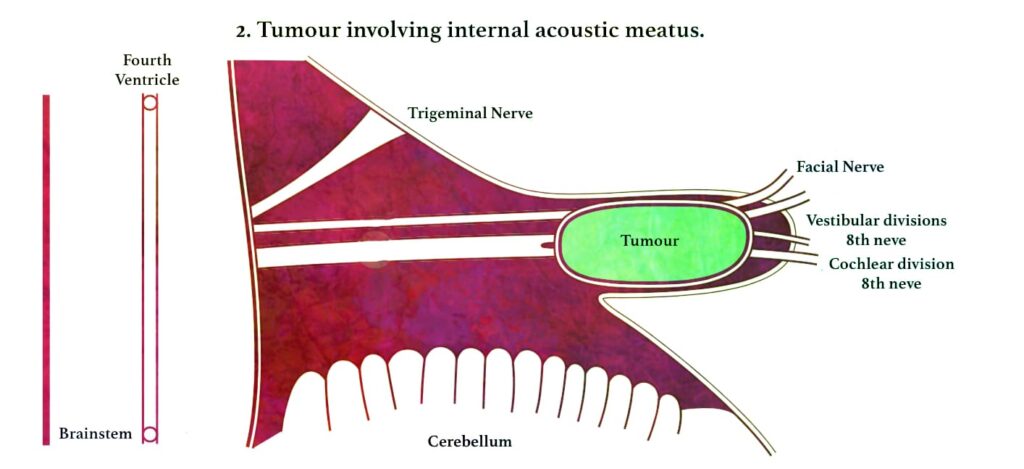
| PATHOPHYSIOLOGY Acoustic Neuroma arises from vestibular division in IAC ↓ Press cochlear, vestibular, facial nerves and labyrinthine vessels ↓ Extend medially into the cerebellopontine angle ↓ Grow antero-superiorly to involve Vth nerve ↓ Grow inferiorly to involve the IXth, Xth and XIth cranial nerves ↓ Further growth inferiorly can displace brain stem and put pressure on cerebellum ↓ Raised intracranial pressure (Hydrocephalus) ↓ Death if untreated |
Further progressive growth in the cerebellopontine angle inferiorly will eventually lead to compression of the brain stem and/or the cerebellum, occlusion of the fourth ventricle. It leads gradually to hydrocephalus followed by death if untreated.
GROSS APPEARANCE:
A well-circumscribed, benign, encapsulated tumour of the vestibular nerve. Small tumours are pink/yellow and rubbery in consistency, whereas large tumours are more yellow, mottled, owing to haemorrhage and fibrosis and cystic in consistency.
MICROSCOPIC APPEARANCE:
Structurally, vestibular schwannoma (Acoustic Neuroma) is composed of two histological patterns:
- Antoni A fibres (arranged in cellular, compact fashion, cells are spindle-shaped and whorling or palisading nuclei (Verocay bodies) are aligned in rows and
- Antoni B fibres (arranged in loose fashion, packed and less cellular with spongy appearance).
Most vestibular schwannomas show predominantly type A histology, with intermingled areas of type B. Microscopically, long spindle cells with rod-shaped nuclei are seen.
CLASSIFICATION ACCORDING TO SIZE OF THE TUMOUR
The classification scheme as proposed and recommended at the consensus meeting on “Reporting Systems of Vestibular Schwannoma” in 2003.
| GRADE | SIZE (mm) |
| 0 Intrameatal | 0 |
| 1 Small | 1–10 |
| 2 Medium | 11–20 |
| 3 Moderately large | 21–30 |
| 4 Large | 31–40 |
| 5 Giant | >40 |
Intrameatal – The tumour is within the meatus and does not extend beyond porus (medial end of IAC). Extrameatal size of such a tumour is zero.
There is another classification which is also commonly used.
- Intracanalicular (when it is limited to internal auditory canal)
- Small size (up to 1.5 cm)
- Medium size (1.5–4 cm)
- Large size (over 4 cm)
CLINICAL FEATURES:
- Vestibulocochlear symptoms. If the tumour (Acoustic Neuroma) arises in the IAC, the earliest symptoms are:
- Vertigo or Imbalance: Abrupt in onset, increases with head movement and exertion. Patients feel mild unsteadiness as contralateral vestibular system generally compensates for the slow ipsilateral loss. It gets resolved spontaneously.
- Hearing loss: The first presenting symptom is unilateral, slow, progressive sensorineural hearing loss. It is associated with impairment of speech discrimination that is out of proportion to the pure tone loss (in majority cases). Unusually, there may be sudden hearing loss in 26% of cases and normal hearing in 1 to 5% of cases.
- Tinnitus: High-pitched and continuous on the affected side. Patients already having hearing loss may not bother about the tinnitus. If a patient is having unilateral tinnitus and not having hearing loss, it should be investigated for acoustic neuroma.
- Any patient having unilateral sensorineural hearing loss and/ or unilateral tinnitus with or without imbalance should raise suspicion of vestibular schwannoma.
2. Cranial Nerve Involvement: The number of cranial nerves involved is directly proportional to the size of the tumour.
- Eighth nerve involvement is suggested by tinnitus, vestibular symptoms, and hearing loss. The tuning fork examination helps detect a sensorineural hearing loss on the suspect side.
- Facial nerve: First sensory fibres are affected than the motor fibres. There is hypoaesthesia or pain on the posterior meatal wall (Hitzelberger’s sign), loss of taste in anterior 2/3rd tongue on electrogustometry test, delayed blink reflex on corneal reflex test and decreased lacrimation on Schirmer test.
- Trigeminal nerve is the earliest extra canalicular nerve to be involved especially when the tumour is > 2.5 cm in diameter and has expanded up to the cerebellopontine angle. There is diminished corneal reflex, ipsilateral facial paraesthesia and numbness. Muscles of mastication are seldom involved.
- It is unusual for vestibular schwannomas to affect cranial nerves other than the fifth, seventh and eighth; however, large cerebellopontine angle tumours may also directly affect neighbouring IXth nerve and Xth nerve (causing difficulty in swallowing, nasal regurgitation and change in voice due to palatal, pharyngeal and laryngeal paralysis). XIth and XIIth, IIIrd, IVth and VIth can also get affected.
3. Brainstem dysfunction: It is seen in very large tumours. There may be ataxic gait, weakness and numbness of the arms and legs with exaggerated tendon reflexes and involvement of lower cranial nerves.
4. Cerebellar dysfunction: Pressure symptoms on cerebellum are seen in large tumours. This is revealed by finger-nose test, knee-heel test, dysdiadochokinesia, ataxic gait and inability to walk along a straight line with tendency to fall to the affected side.
5. Raised intracranial pressure. There may be nausea, vomiting, headache, diplopia, papilloedema with blurring of disc margins.
INVESTIGATIONS:
The tumour must be diagnosed at an early stage when it is still intra-canalicular. Hence, all cases of unilateral sensorineural hearing loss with tinnitus or imbalance are to be evaluated with the utmost care and priority.
- Neurological Tests. It includes cranial nerves examination, vestibular function tests, cerebellar function tests, brainstem signs of pyramidal and sensory tracts. Fundus is examined to see blurring of disc margins or papilloedema caused by raised intracranial pressure and optic nerve compression.
- Vestibular function tests. Romberg test may show a tendency to fall to the side of the lesion, and Unterberger step test may show rotation to the side of the lesion. There may be a diminished or absent response on the caloric test.
- Cerebellar function tests. Finger-nose test, dysmetria, knee-heel test and ataxic gait can establish cerebellar involvement.
- Audiological Tests.
- PTA. An audiogram showing an asymmetrical sensorineural hearing loss more marked for high frequencies with disproportionately poor speech discrimination on speech audiometry indicates potential vestibular schwannoma.
- Roll-over phenomenon, i.e. discrimination score decreases when loudness increases after a particular level. This feature is consistent with retrocochlear lesions.
- Brainstem Response Audiometry (BERA): It is the most sensitive test in the diagnosis of vestibular schwannoma. There is an interaural wave V latency difference of greater than 0.2 milliseconds, Prolonged inter-peak latencies greater than 4.4 milliseconds for I-V waves, 2.3 milliseconds for I-III waves, 2.1 milliseconds for III-V waves or complete absence of wave V.
- Short Increment Sensitivity Index (SISI) test shows a retrocochlear type of lesion (score of 0–20%).
- Threshold tone decay test shows a retrocochlear type of lesion.
- Stapedial reflex delay present. It is not done routinely as more sensitive and specific tests are available.
- Recruitment phenomenon is absent as it is in cochlear lesions.
- Radiological Tests:
- Plain X-rays (transorbital, Stenver’s, Towne’s and submentovertical views). It can detect about 80% of tumours except for intracanalicular tumours.
- MRI with gadolinium contrast. It is used to confirm (gold standard) the diagnosis and it is superior to CT scan. Smallest (few milli-metres) of intracanalicular tumours can be detected.
- Computed tomography (CT) scan.
- Vertebral angiography.
DIFFERENTIAL DIAGNOSIS:
Acoustic neuroma should be differentiated from other three most common cerebellopontine angle tumours, e.g. meningioma, primary cholesteatoma and arachnoidal cyst. One should also rule out Meniere’s disease.
TUMOURS OF CEREBELLOPONTINE ANGLE:
- Acoustic neuroma
- Meningioma
- Epidermoid (cholesteatoma)
- Arachnoid cyst
- Schwannoma of other cranial nerves (e.g. CN V >VII > IX, X, XI)
- Aneurysm
- Glomus tumour
- Metastasis
TREATMENT.
Observation and follow-up.
Surgery. Mainstay of treatment. Surgical approach depends on the size of tumour. The various surgical approaches to the cerebellopontine angle are:
- Middle cranial fossa approach. The middle fossa approach is preferred in hearing preservation surgery and small intracanalicular tumours. However, the approach is somewhat cramped. Usually done in intracanalicular tumour < 1 cm size.
- Trans-labyrinthine approach. Most favoured approach. Early identification of the facial nerve and avoidance of cerebellar retraction or resection is its advantage. It involves the destruction of the inner ear and so is not an option for hearing preservation surgery. It has a higher incidence of cerebrospinal fluid (CSF) fistula than other approaches. Usually done in CPA tumour < 3 cm size.
- Suboccipital (retrosigmoid) approach. Preferred for removal of all posterior fossa tumours but particularly for large ones. But it gives a limited view of the internal auditory canal and chances of residual tumour is greater. Usually done in large CPA tumour > 3 cm size.
- Combined translabyrinthine-suboccipital approach.
COMPLICATIONS OF SURGERY:
- 7th, 5th, 6th, 4th Cranial nerve palsy
- CSF fluid leakage (Otorrhea, Rhinorrhoea)
- Intracranial infection (Meningitis)
- Intraoperative bleeding
- Brain oedema
- Venous air embolism
- Cardiac arrhythmia
- Brain herniation
- Death, stroke, haemorrhage, brain injury
Although surgery has a role for those with large tumours (>3 cm maximal intracranial diameter), beyond which the role of stereotactic radiotherapy is considered minimal. For smaller tumours, a conservative approach is commonly advised.
RADIOTHERAPY. Can be done in patients who are not willing for surgery or have contraindications to surgery or have a residual tumour. Radiotherapy arrests the growth (and hence avoid surgery) of the tumour and preserves auditory function.
X-knife or Gamma knife surgery. This is stereotactic radiotherapy where radiation energy is converged and focus only on the tumour, sparing surrounding nerve tissue. This causes arrest of the growth of the tumour or may decrease its size.
Cyber knife. It is more accurate. It uses real-time image guidance technology through computer-controlled robotics.
———- End of the chapter ———–
Anatomy of Temporal Bone Anatomy of Temporal Bone Anatomy of Temporal Bone Anatomy of Temporal Bone Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone, Anatomy of Temporal Bone
-
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
-
Join our Facebook group: https://www.facebook.com/groups/628414274439500
-
Read chapter Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Michael M Paparella, Textbook of Otolaryngology: Principles & Practice.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
