GLOMUS TUMOUR (Also known as paragangliomas or chemodectomas) was first described by Guild (Glasscock, 1982). It is the most common benign neoplasm of middle ear and the second most common tumour of the temporal bone. The tumour arises from the neural crest paraganglionic cells (glomus bodies) which resemble carotid body in structure. Glomus bodies are found in the dome of jugular bulb or on the promontory along the course of tympanic branch of IXth cranial nerve (Jacobson’s nerve). The tumour is slow growing benign neoplasm, often seen in fifth and sixth decades of life. Glomus tumour is five times more female to male preponderance.
Major feeding vessel of glomus tumour is ascending pharangeal artery, which is a branch of the external carotid artery. 10% of the glomus tumours are familial, 10% are multicentric (occurring in more than one site) and up to 10% are functional, i.e. they secrete catecholamines.
Pathologically, It is a benign, nonencapsulated but extremely vascular tumour. Its rate of growth is very slow (similar to acoustic neuroma) and it rarely metastasize. Although it is histologically benign, these tumours can grow aggressively and cause multiple cranial nerve abnormalities.
Macroscopically, All paragangliomas are firm, well-circumscribed lesions that are yellow, tan, brown or reddish in colour. They can have a thin, but focally thickened, fibrous capsule.
Microscopically, it shows masses or sheets of epithelial cells which have large nuclei and a granular cytoplasm. There is abundance of thin-walled blood sinusoids with no contractile muscle coat, accounting for profuse bleeding from the tumours.
These tumours occur in the temporal bone (glomus tympanicum and glomus jugulare), the carotid bifurcation (glomus caroticum), and the upper parapharyngeal space (glomus vagale).
Common sites of paraganglioma are:
- Middle ear (glomus tympanicum)
- Jugular fossa (glomus jugulare)
- Carotid artery bifurcation (carotid body tumours or glomus caroticum)
- Inferior ganglion (ganglion nodosurn) of the vagus nerve (glomus vagale).
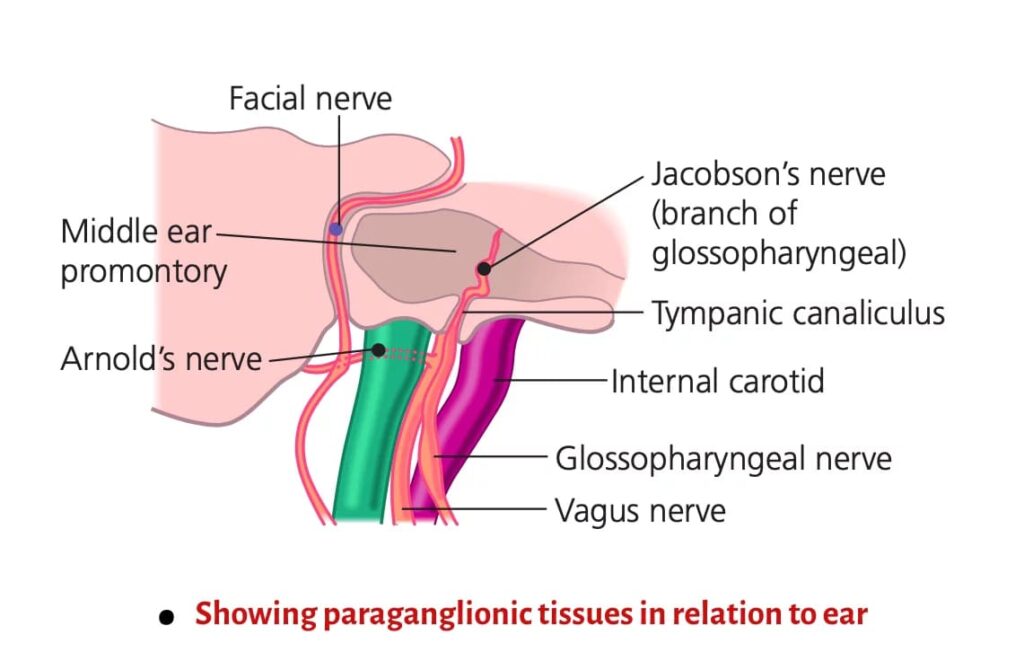
1. Glomus Tympanicum. It is the most common middle ear tumour. It arises from the paraganglion’s located in the promontory. They are located along the tympanic branch (Jacobson’s nerve) of the glossopharyngeal nerve and auricular branch (Arnold’s nerve) of the vagus nerve. In contrast to glomus jugulare, bone erosion is rare in glomus tympanicum (the hypotympanic floor, jugular fossa and ossicles are usually intact). Large tumour may cause bulge of the tympanic membrane, and a smooth indentation of the promontory causing aural symptoms. Posteriorly it may extend into the mastoid and inferiorly into the hypotympanic air cells and jugular fossa.
CT is the investigation of choice for diagnosis. Axial and coronal sections shows a well-defined nodular area of soft tissue on the cochlear promontory. MRI is only indicated for larger lesions extending outside the middle ear cavity. It seldom requires preoperative embolization and can be resected with conventional tympanoplasty techniques.
2. Glomus Jugulare. It arises from the paraganglion’s located in the jugular bulb, the Xth nerve ganglion, and/ or from the Arnold or Jacobson nerves.
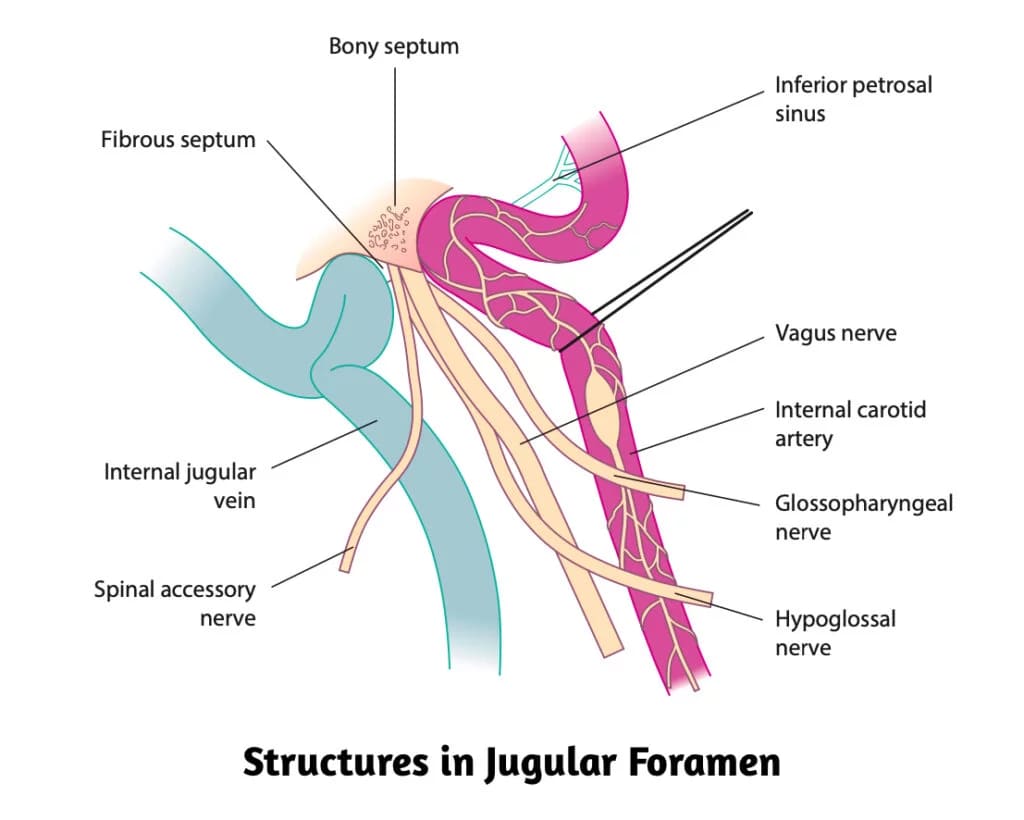
Glomus jugulare tumours erode the jugular fossa and break through the bony roof of the jugular fossa causing neurological signs of IXth to XIIth cranial nerve involvement. Destruction of bone around the caroticojugular spine, jugular tubercle, and hypoglossal canal may also be seen. As the tumor increases in size, it causes erosion of floor of hypotympanum and may fill the entire middle ear cavity and from there into the external auditory canal.
Lateral extension of the lesion into the mastoid often leads to erosion of the facial canal and involvement of the facial nerve. Medially it invades petrous pyramid and destruction of perilabyrinthine bone and petrous apex. Extracranially it may compress jugular vein or invade its lumen. lntracranial involvement is often observed in large tumors, although the lesion usually remains extradural.
Spread of Glomus Jugulare Tumour
- As the floor of the hypotympanum is eroded, the tumour extends superiorly into the middle ear cavity and later perforate through the tympanic membrane to present into the external auditory canal as a vascular polyp.
- It may invade labyrinth, petrous pyramid and the mastoid.
- It may invade jugular foramen and the base of skull, causing IXth to XIIth cranial nerve palsies.
- By spread through eustachian tube, it may present in the nasopharynx.
- Intracranially it may spread to the posterior and middle cranial fossae. lntracranial involvement is often observed in large tumors, although the lesion usually remains extradural.
- Metastatic spread to lungs and bones is rare, but seen in 4% of cases. Metastatic lymph node enlargement can also occur.
MRI is the study of choice and shows characteristic ‘salt and pepper’ appearance on T1 images, which is a combination of flow voids from intratumoural vessels, and areas of micro-haemorrhage.
CT of glomus jugulare helps in detection of the bony changes. CT of glomus jugulare shows a typical pattern of permeative bone destruction that involves the carotico-jugular spine early in the disease process.
Fisch classification for glomus tumours. It helps in surgical planning and provide standards for reporting surgical results.
- Type A tumor: Limited to the middle ear cleft (glomus tympanicum)
- Type B tumor: Limited to the tympanomastoid area with no infra-labyrinthine compartment involvement
- Type C tumor: Involving the infra labyrinthine compartment of the temporal bone and extending into the petrous apex
- Type C1 tumor: With limited involvement of the vertical portion of the carotid canal
- Type C2 tumor: Invading the vertical portion of the carotid canal
- Type C3 tumor: Invasion of the horizontal portion of the carotid canal
- Type D1 tumor: With an intracranial extension <2 cm in diameter
- Type D2 tumor: With an intracranial extension >2 cm in diameter
Clinical features:
Almost in 90% of skull base paragangliomas have conductive hearing loss and symptoms pertain to the ear.
- Pulsatile tinnitus and/ or hearing loss. Earliest symptoms are pulsatile tinnitus and/ or hearing loss. Tinnitus is swishing in character, synchronous with pulse and can be temporarily stopped by carotid pressure. A glomus tympanicum may present early with conductive hearing loss which is slowly progressive in nature; whereas glomus jugulare may present with a mixed deafness when the middle and inner ears are both involved. There may be otalgia, ear fullness, otorrhea and aural bleeding.
- Polypoidal mass. On examination red, vascular polyp in the ear canal may be present in advance disease. It bleeds readily and profusely either spontaneously or on attempts to clean it or at biopsy.
- Dizziness or vertigo.
- Earache is generally not present. Absence of earache differentiates it from carcinoma of the external and middle ear.
- Ear discharge may be seen due to secondary infection and the condition may simulate chronic suppurative otitis media with polyp.
- Tumour mass. Tumour may present as a mass over the mastoid or in the nasopharynx.
- Cranial Nerve Palsies. This is a late feature appearing several years after aural symptoms. CN VII and VIII become involved in the internal auditory canal. IXth to XIIth cranial nerves become involved in the jugular foramen. Order of frequency of involvement (VII > X > XII > IX > XI). There is dysphagia and hoarseness with asymmetric palatal elevation or an abnormal gag reflex (IX, X) and dysarthria and hoarseness of voice due to unilateral paralysis of vocal cords (X) with weakness of the trapezius and sternomastoid muscles (XI) and deviation on protrusion, wasting and atrophy of tongue (XII) nerves. Horner’s syndrome (ptosis, meiosis, anhydrosis and enopthalmus) can be observed.
- Audible Bruit. Auscultation with stethoscope should be done over the upper neck and mastoid, which may reveal “systolic bruit” being indicative of underlying pathology.
- Catecholamines symptoms. Headache, sweating, palpitation, hypertension and anxiety.
DIAGNOSIS:
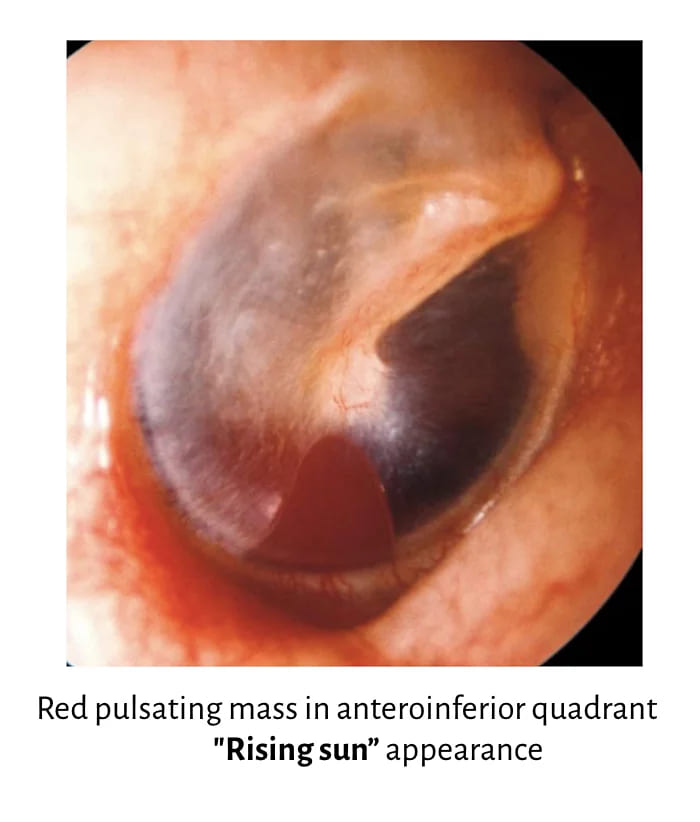
- On otoscopic examination reddish-blue reflex may be seen through intact tympanic membrane. If tumour is arising from the promontory red pulsatile mass may be seen behind the tympanic membrane and glomus tympanicum tumour is the most likely diagnosis. If tumour is arising from the floor of middle ear, ‘Rising sun appearance’ is seen and glomus jugulare tumour is the most likely diagnosis. Tympanic membrane also appears blue in cases of hemotympanum (temporal bone fracture), glue ear, glomus tumor and haemangioma of middle ear.
- “Pulsation sign” (Brown’s sign) is positive, i.e. when earcanal pressure is raised with Siegel’s speculum, tumour pulsates vigorously and then blanches; reverse happens with the release of pressure.
- Polypoidal mass. On examination red, vascular polyp in the ear canal may be present in advance disease. It bleeds readily and profusely either spontaneously or on attempts to clean it or at biopsy.Preoperative biopsy or myringotomy is contraindicated. Avoid injuring the high jugular bulb (which appears darker in colour) or aberrant internal carotid artery (normally placed in the anterior mesotympanum).
- Inspection and palpation of the neck (cervical mass and trapezius weakness in extensive jugulotympanic glomus). Examination of the neck is also important in patients with glomus tumours to identify synchronous paragangliomas or detect direct extension of a large tumour into the neck (e.g. glomus jugulare or vagale).
- Inspection of the oral cavity and pharyngolarynx (tongue deviation, decreased gag reflex, vocal cord paresis in extensive jugulotympanic glomus).
INVESTIGATIONS:
Combination of CT, MRI and angiography is required for assessment of patients with glomus tumours.
- Computed Tomography (CT) Scan Head. Helps in differentiating glomus tympanicum from the glomus jugulare tumour by identification of caroticojugular spine which is eroded in the latter. CT scan also helps to differentiate it from the aberrant carotid artery, high or dehiscent jugular bulb.
- MRI. It shows soft tissue extent of tumour. Magnetic resonance angiography and venography further help to delineate invasion of jugular bulb and vein or compression of the carotid artery.
- CT Head and MRI Combined. together provide an excellent preoperative guidance in the differential diagnosis of petrous apex lesions.
- Four-Vessel Angiography. It is necessary when CT head shows involvement of jugular bulb, carotid artery or intradural extension. It also helps to delineate any other glomus tumour (as they may be multiple), find the feeding vessels or embolization of tumour if required.
- Brain Perfusion and Flow Studies. They are necessary when tumour is pressing on internal carotid artery. If the case needs surgery, brain perfusion and adequacy of contralateral internal carotid artery and circle of Willis can be assessed. If needed, xenon blood flow and isotope stud-ies are done for precise blood flow, and the risk of stroke and need for surgical replacement of internal carotid artery.
- Catecholamine secretion : Serum levels of catecholamines or their breakdown products in 24-h urine (metanephrine, vanillylmandelic acid).
- Pure tone and speech audiometry to assess the type and degree of hearing loss. Vestibular function tests for dizziness or vertigo.
TREATMENT:
1. Surgical removal. Treatment of choice is complete surgical excision. The surgical approach depends on the limits of the tumor and its classification. Surgical approaches to glomus tumours:
- Transcanal Approach. Suited for limited glomus tympanicum tumour where entire circumference of the tumour is visible, only tympanotomy will suffice to gain access to the tumour. Indicated in Fisch Type A tumor.
- Hypotympanic Approach. Suited for tumours limited to promontory with extension to hypotympanum but not into the mastoid. A superiorly based tympanomeatal flap is raised by postauricular approach. Bony inferior tympanic ring is drilled away to see the lower limit of tumour.
- Extended Facial Recess Approach. Used for glomus tympanicum extending into mastoid but not into the jugular bulb. If extensive, modified radical operation is done.
- Mastoid-Neck Approach. Used for glomus jugulare tumours not extending to internal carotid artery, posterior cranial fossa or neck.
- Infratemporal Fossa Approach of Fisch. Used for large glomus jugulare tumours.
- Transcondylar Approach. Used for tumours extending towards foramen magnum. Usually they are recurrent glomus jugulare tumours. It gives approach to craniocervical junction with exposure of occipital condyle and jugular tubercle.
2. Radiation. Irradiation may be appropriate for tumours impossible to remove surgically, having intracranial extension, residual tumours, or for old patients with limited life expectancy. The aim is to reduce its vascularity and bring about sclerosis and fibrosis, hence arrest its growth.
3. Embolization reduces vascularity of the tumour. It is done before the surgery to reduce intra-operative bleeding and gives comparatively clean operative field during surgery. Thereby it reduces chances of complications and intraoperative time. Embolization of feeding vessels is done 1–2 days before operation. Embolization can also be done in the in-operable patients who have received radiation. Gelfoam and coils can be are used in feeding vessel occlusion proximal to the tumour. Gelfoam powder is derived from derived from pork-skin gelatin.
4. Combination of the above techniques.
———- End of the chapter ———–
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Stell and Maran’s, Textbook of Head and Neck Surgery and Oncology.
- Michael M Paparella, Textbook of Otolaryngology: Principles & Practice.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Susan Standring, Gray’s Anatomy.
- Ganong’s Review of Medical Physiology.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
