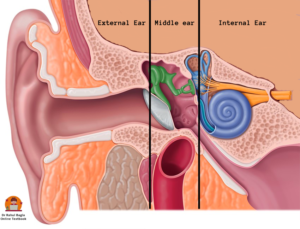
Anatomy of Internal ear. The internal ear or the labyrinth is an important organ of hearing via the cochlea, and balance via the vestibular system. It is present in the petrous part of the temporal bone between the middle ear laterally and the internal acoustic meatus medially.
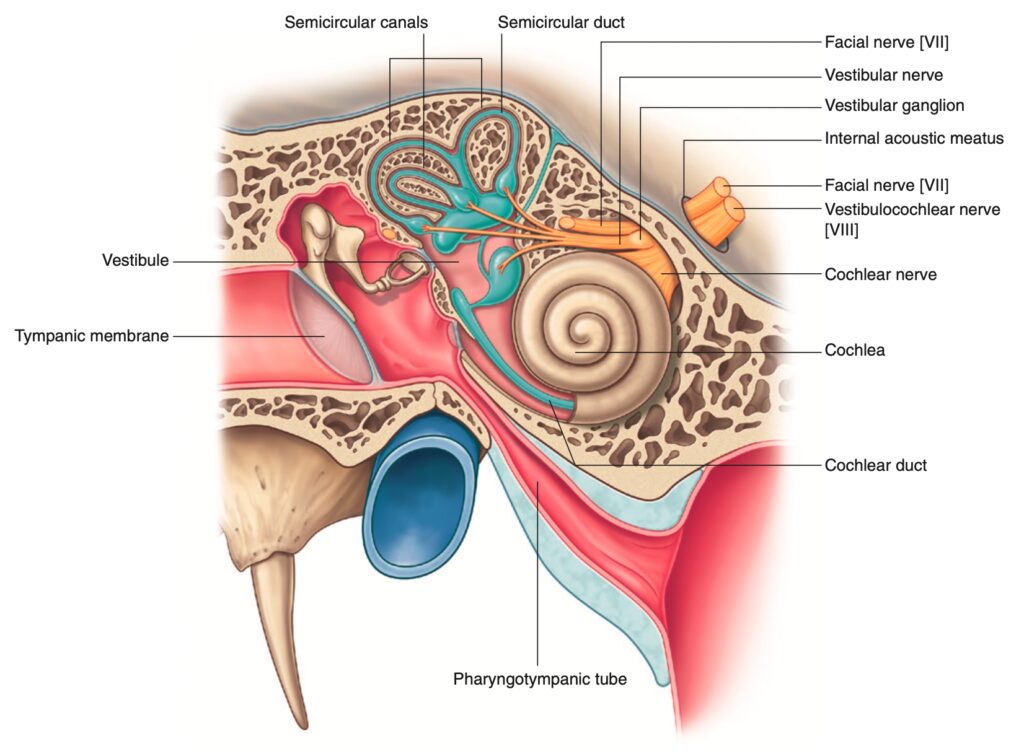
It is responsible for transduction of mechanical energy to electrical signals that can then be passed to the brain along the auditory or vestibular nerves. Movements of the stapes footplate are transmitted to the cochlear fluids which moves the basilar membrane and sets up a shearing force between the tectorial membrane and the hair cells. The distortion of hair cells gives rise to cochlear microphonics, which trigger the nerve impulse. Internal ear is also responsible for maintaining balance by detecting position and motion.
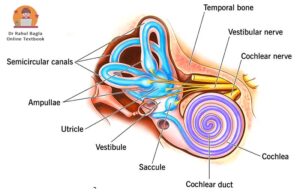
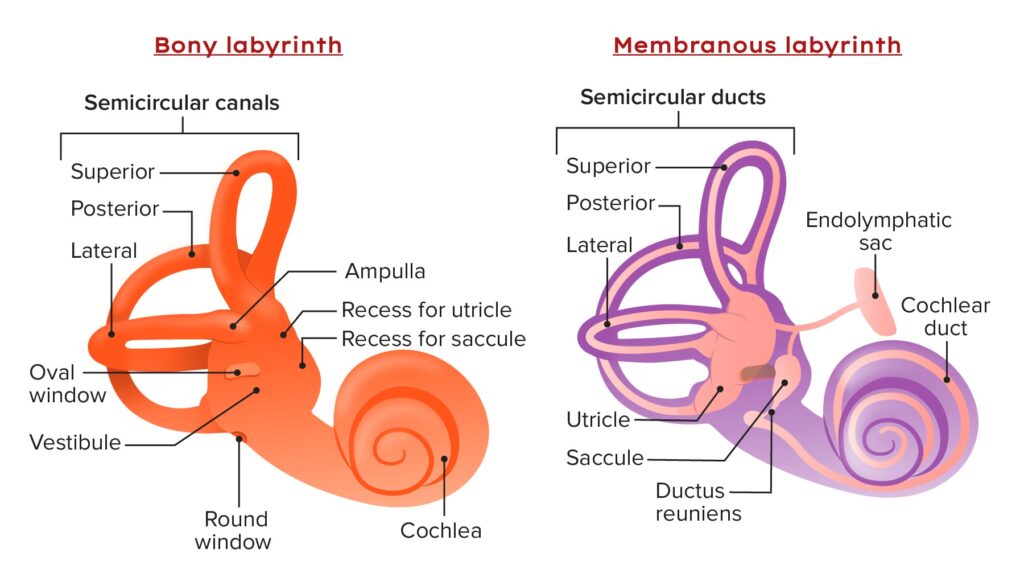
It is divided into bony and membranous labyrinth. Perilymph is filled in the space present between membranous and bony labyrinths. The membranous labyrinth is filled with clear fluid called endolymph. This means that the membranous labyrinth is suspended in the perilymph of the bony labyrinth.
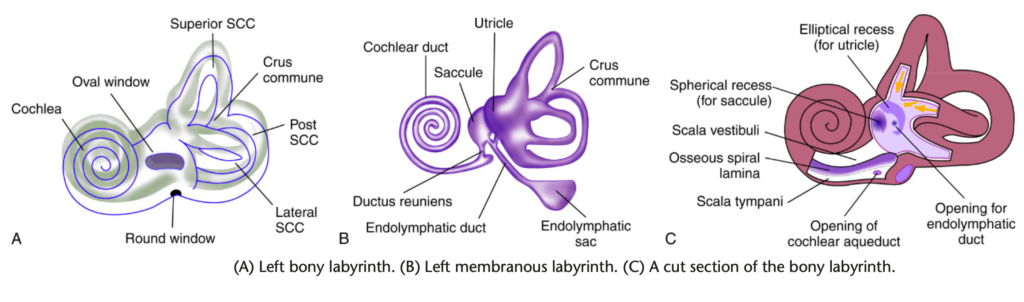
- Bony labyrinth consists of vestibule, semi-circular canals and cochlea.
- Membranous labyrinth consists of the cochlear duct, the utricle and saccule, the three semicircular ducts, and the endolymphatic duct and sac.
BONY LABYRINTH.
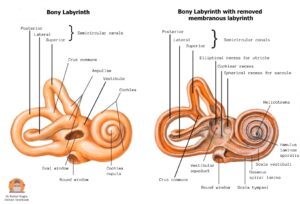
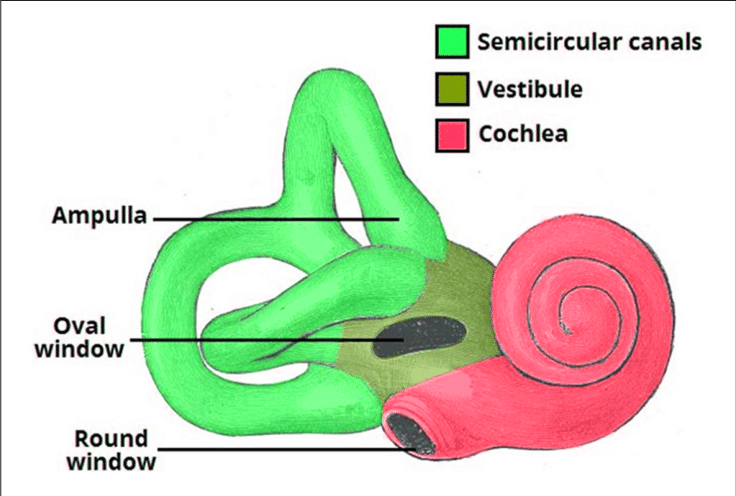
It consists of three parts: the vestibule, the semicircular canals and the cochlea.
Bony labyrinth showing the vestibule, the semicircular canals and the cochlea.
- Vestibule. It is the central chamber (5 mm) of the labyrinth. It is separated from the middle ear by the oval window and communicates anteriorly with the cochlea and posteriosuperiorly with the five openings of semi-circular canals. The vestibule communicates with the posterior cranial fossa through the vestibular aqueduct.
Vestibule has following important structures:
- On its lateral wall – Oval window (Fenestra vestibuli) is present which is closed by footplate of stapes.
- On its medial wall – Two recesses are present, a spherical recess, which lodges the saccule, and an elliptical recess, which lodges the utricle. Recesses are part of bony labyrinth while saccule and utricle are part of membranous labyrinth. Opening of aqueduct of vestibule is also present below the elliptical recess. Through this passes the endolymphatic duct.
2. Semicircular canals. There are three semicircular canals (SCC), the lateral (horizontal), posterior and superior (anterior). Each canal has a diameter of 0.8 mm and occupies 2/3rd of a circle. The length of lateral SCC is 12–15 mm, posterior SCC is 18–22 mm and superior SCC is 15–20 mm. The lateral SCC is the shortest SCC and is set at an angle of about 30 degrees to the horizontal plane. All three lie in planes at right angles to one another.
- Lateral SCC detects rotation of the head in the transverse plane (vertical axis).
- Posterior SCC detects rotation of the head in the coronal plane.
- Superior SCC detects rotation of the head in the sagittal plane.
Each canal has an ampullated end which opens independently into the vestibule. The non-ampullated ends of posterior and superior canals unite to form a common channel called crus commune (4 mm length). Crus commune opens into the medial part of vestibule. So, the three SCCs open into the vestibule by five openings and not by six openings.
3. Cochlea. It is present anterior to vestibule. The bony cochlea twists on itself to form a coiled tube (like a snail) making 2.5 to 2.75 turns (30 mm length) around a central pyramid of bone called modiolus. The wide base of modiolus is directed towards internal acoustic meatus and transmits vessels and nerves to the cochlea. A thin plate of bone called osseous spiral lamina, winds spirally like the thread of a screw around the modiolus. The spiral ganglions are present in the Rosenthal’s canal, which runs along the osseous spiral lamina. This osseous spiral lamina gives attachment to the basilar membrane and divides the bony cochlear tube into three compartments:
- Scala vestibuli which contains perilymph.
- Scala tympani which contains perilymph.
- Scala media or the membranous cochlea which contains endolymph.
The scala vestibuli and scala tympani communicate with each other through an opening called helicotrema at the apex of cochlea. Footplate of stapes closes the scala vestibuli separating it from the middle ear. Secondary tympanic membrane also known as the round window membrane closes the scala tympani separating it from the middle ear. The scala tympani runs parallel to the scala vestibuli and terminates at the round window. It is also connected with the subarachnoid space through the aqueduct of cochlea (Figure 1.19). The bony bulge in the medial wall of middle ear, the promontory, is due to the basal coil of the cochlea.
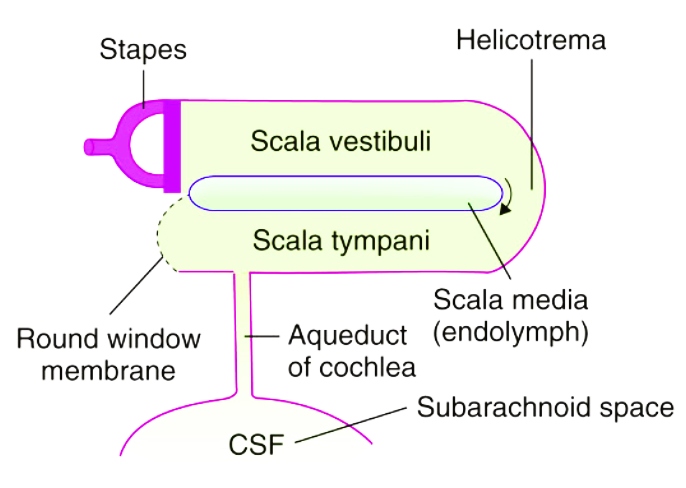
Perilymphatic system. CSF passes into the scala tympani through the aqueduct of the cochlea.
MEMBRANOUS LABYRINTH
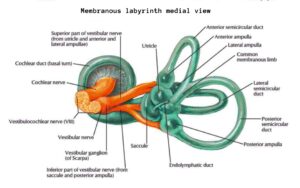
Membranous labyrinth consists of two sacs (utricle and saccule) and four ducts (three semicircular ducts and one cochlear duct). The utricle, saccule, and three semicircular ducts are related to the balance (equilibrium) while the cochlear duct is related to the hearing.
The general structure of the membranous labyrinth is:
- the saccule and utricle are present in the vestibule of the bony labyrinth. Its sensory epithelium is called macula.
- the three semicircular ducts are present in the three semicircular canals of the bony labyrinth. Its sensory epithelium is called cristae.
- the cochlear duct is present in the cochlea of the bony labyrinth. The sensory epithelium of the cochlea is the organ of Corti.
- All of the sensory epithelia (macula, crista and organ of corti) are composed of two main cell types: sensory hair cells and non-sensory supporting cells.
Utricle and saccule.
- The utricle is present in the posterior part of bony vestibule in the elliptical recess. The five openings of the three semicircular ducts open in the utricle. The utricle is connected to the saccule through utriculosaccular duct, which continues as endolymphatic duct that passes through the vestibular aqueduct. Terminal part of endolymphatic duct is dilated to form endolymphatic sac between the two layers of dura on the posterior surface of the petrous bone in the posterior cranial fossa. Endolymphatic sac functions in resorption of endolymph. Endolymphatic sac is exposed for drainage or shunt operation in Meniere’s disease.
- The saccule is present in the spherical recess of bony vestibule, anterior to the utricle and opposite the stapes footplate. The cochlear duct empties into the saccule through the thin reunion duct. In Meniere’s disease, the distended saccule lies against the stapes footplate and can be surgically decompressed by perforating the footplate.
- The utricle is bigger than saccule and lies superior to saccule. The sensory epithelium (sense organ) of both utricle and saccule is called macula and in the ampulla of each of the three semicircular ducts it is the crista. The utricle responds to linear acceleration in the horizontal plane and sideways head tilts. The saccule responds to linear acceleration in the vertical plane, such as forward-backward and upward-downward movements.
Semicircular ducts. They are three in number and open in the utricle. Each semicircular duct is same in shape to its complementary bony semicircular canal including a dilated end forming the ampulla. They correspond exactly to the three bony canals. The ampullated end of each duct contains a thickened ridge of neuroepithelium called crista ampullaris. Its sensory epithelium is called cristae which respond to rotational movement in any direction.
Cochlear duct. Also called membranous cochlea or the scala media. It is a blind coiled tube.
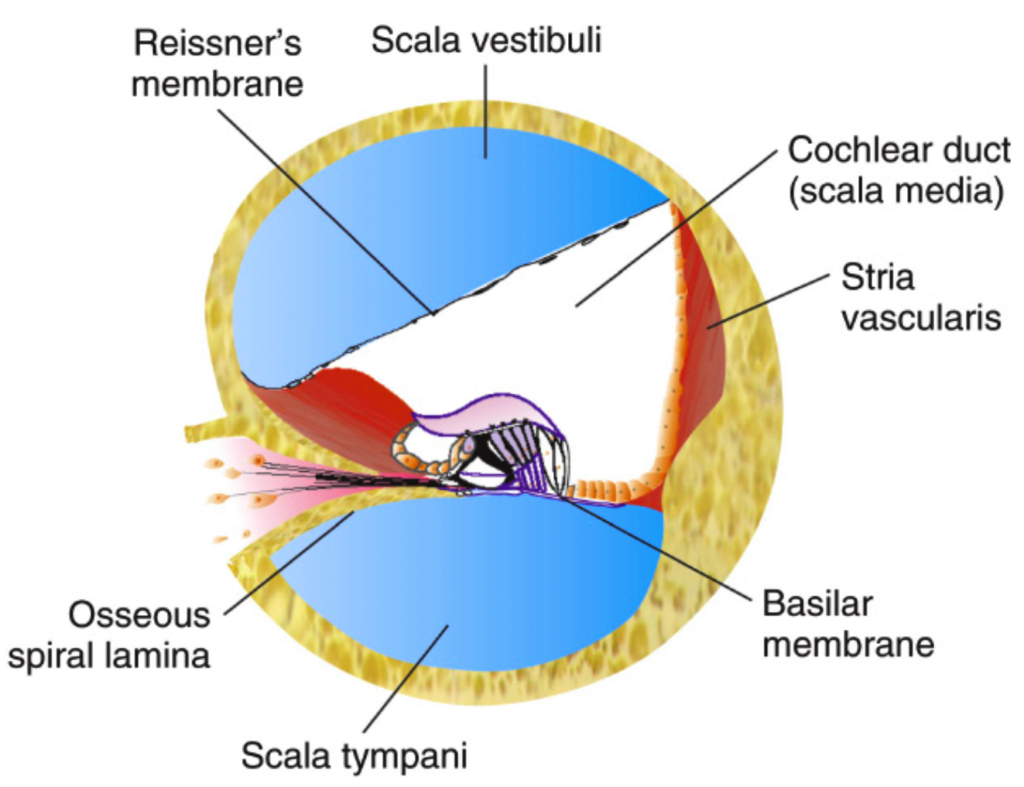
A section through the cochlea to show scala media (cochlear duct), scala vestibuli and scala tympani.
It appears triangular on cross-section and its three walls are formed by:
- the basilar membrane (floor), which supports the organ of Corti and separates the scala media endolymph from the perilymph in the scala tympani. Its length increases as it proceeds from the basal coil to the apical coil. So, the higher frequencies of sound are heard at the basal coil while lower tones at the apical coil.
- the Reissner’s membrane (roof), which separates it from the scala vestibule. It separates scala endolymph from the perilymph in the scala vestibuli.
- the stria vascularis, which contains vascular epithelium and is concerned with secretion of endolymph. It contains vascular epithelium and secrets endolymph.
Cochlear duct is connected to the saccule by ductus reuniens. The length of basilar membrane increases as we proceed from the basal coil to the apical coil. It is for this reason that higher frequencies of sound are heard at the basal coil while lower ones are heard at the apical coil. The utricle is the larger of the two sacs. It is oval, elongated and irregular in shape and is in the posterosuperior part of the vestibule of the bony labyrinth.
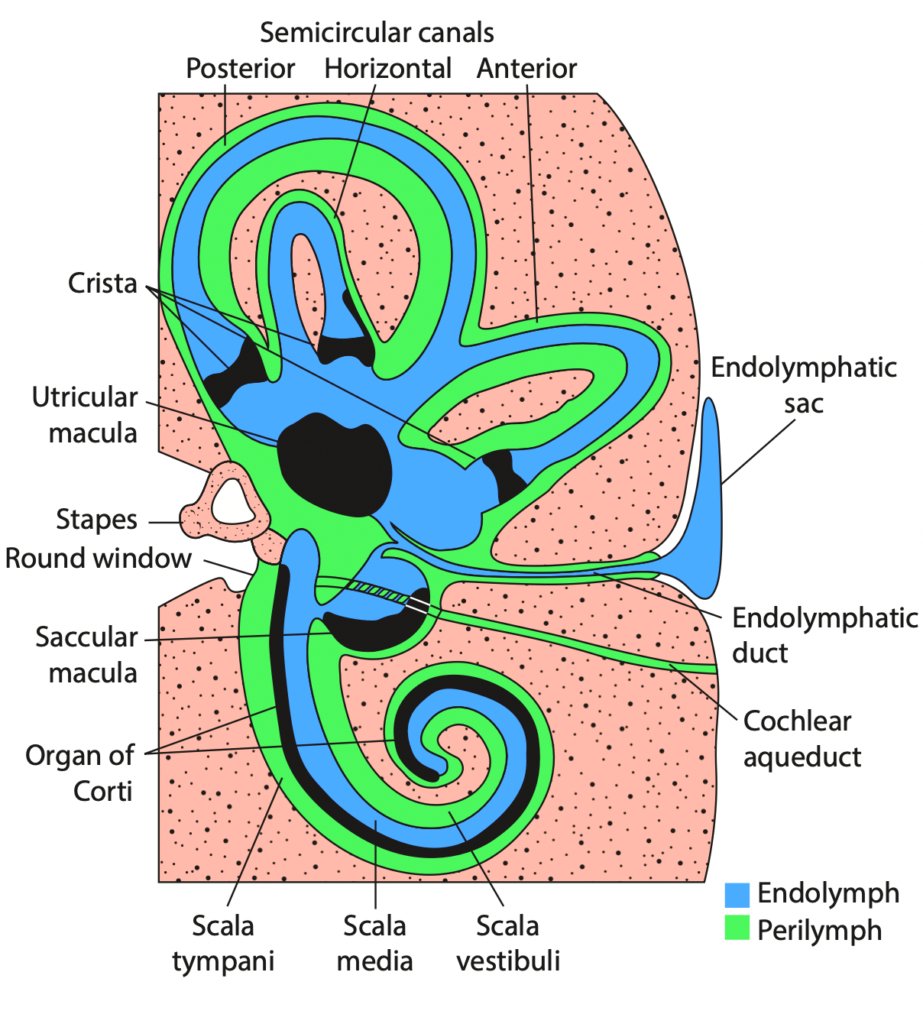
Overview of Inner ear
INNER EAR FLUIDS AND THEIR CIRCULATION
There are two fluids in the inner ear: perilymph and endolymph. Perilymph fills the space between bony and membranous labyrinth while endolymph fills the entire membranous labyrinth.
- Perilymph. It resembles extracellular fluid and is rich in Na ions. It communicates with CSF through the aqueduct of cochlea which opens into the scala tympani near the round window. In fact this duct is not a direct communication but contains connective tis- sue resembling arachnoid through which perilymph percolates. There are two views regarding the formation of perilymph: (i) It is a filtrate of blood serum and is formed by capillaries of the spiral ligament and (ii) it is a direct continuation of CSF and reaches the labyrinth via aqueduct of cochlea.
| TABLE 1.2 COMPOSITION OF INNER EAR FLUIDS | Endolymph | Perilymph | CSF |
| Na+ (mEq/L) | 5 | 140 | 152 |
| K+ (mEq/L) | 144 | 10 | 4 |
| Protein (mg/dL) | 126 | 200–400 | 20–50 |
| Glucose (mg/dL) | 10–40 | 85 | 70 |
Values are average and may differ slightly according to the site of collection of endolymph (cochlea, utricle, sac) and perilymph (scala tympani or scala vestibuli).
2. Endolymph. It fills the entire membranous labyrinth and resembles intracellular fluid, being rich in K ions. It is secreted by the secretory cells of the stria vascularis of the cochlea and by the dark cells (present in the utricle and also near the ampullated ends of semicircular ducts). There are two views regarding its flow: (i) longitudinal, i.e. endolymph from the cochlea reaches saccule, utricle and endolymphatic duct and gets absorbed through endolymphatic sac, which lies in the subdural space and (ii) radial, i.e. endolymph is secreted by stria vascularis and also gets absorbed by the stria vascularis. This view presumes that endolymphatic sac is a vestigial structure in man and plays no part in endolymph absorption.
BLOOD SUPPLY OF LABYRINTH
The entire labyrinth receives its arterial supply through labyrinthine artery, which is a branch of anterior-inferior cerebellar artery but sometimes from the basilar.
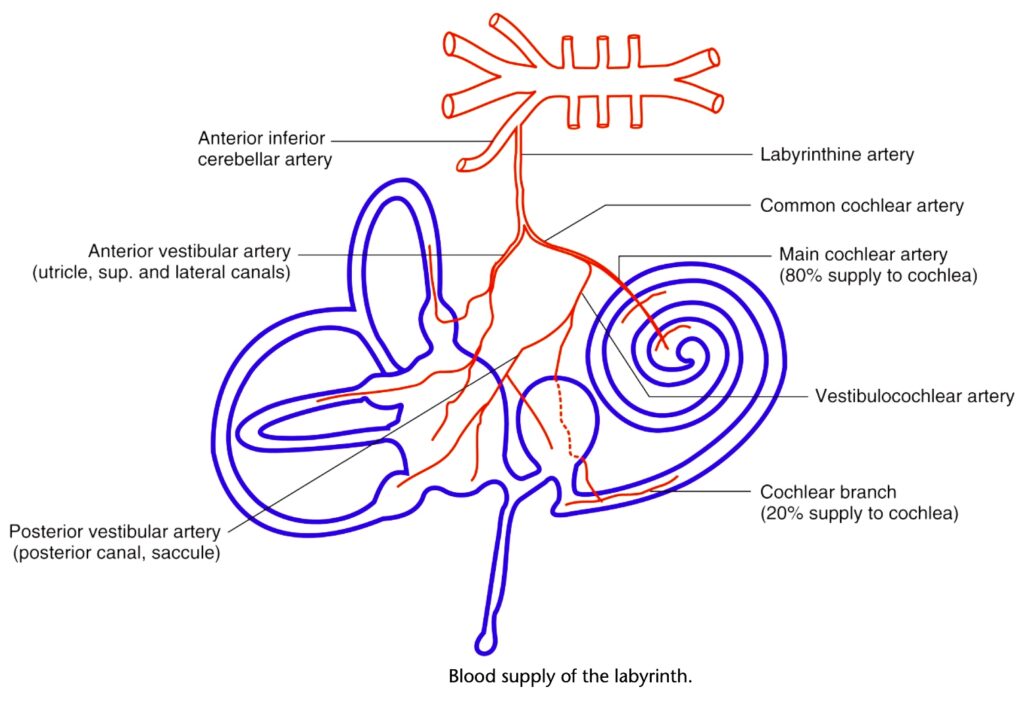
Divisions of the labyrinthine artery which supply blood to various parts of the labyrinth.
Venous drainage is through three veins, namely internal auditory vein, vein of cochlear aqueduct and vein of vestibular aqueduct, which ultimately drain into inferior petrosal sinus and lateral venous sinus.
It is to be noted that:
1. Blood supply to the inner ear is independent of blood supply to middle ear and bony otic capsule, and there is no cross circulation between the two.
2. Blood supply to cochlea and vestibular labyrinth is segmental, therefore, independent ischaemic damage can occur to these organs causing either cochlear or vestibular symptoms.
——- End of the chapter ———–
-
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
-
Join our Facebook group: https://www.facebook.com/groups/628414274439500
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Susan Standring, Gray’s Anatomy.
- Frank H. Netter, Atlas of Human Anatomy.
- B.D. Chaurasiya, Human Anatomy.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
