Assessment of hearing – Hearing tests
CLINICAL HEARING TESTS
(i) Finger Friction Test: It is a screening test done to assess hearing threshold and sound localisation. The examiner snaps the thumb and middle finger to create a clicking sound near the patient’s ear and the patient is asked to appreciate the sound with closed eyes.
(ii) Watch Test: It is a screening test which was used by the clinicians before the invent of the audiometer. The examiner brings a watch with a ‘clicking’ sound close to the patient’s ear and measures the distance at which this sound is heard.
(iii) Free field voice/ Speech Test is a structured test of hearing for a clinical setting. Prerequisite: Each ear is tested separately after masking the opposite ear. To produce masking, the assistant rubs the index finger on the patient’s tragus or conchal bowl. A normal person hears sound of conversation at 12 m (40 ft), whisper (with residual air after normal expiration) at 6 m (20 ft). However, 6 m is taken as normal for both conversation and whisper while doing this test.
Procedure: Speech test must be done in quiet surroundings.
- The patient is made to stand at 6 metres with his ‘test ear’ facing towards the examiner with his eyes closed to avoid lip reading
- An assistant blocks the non-test ear of the patient by giving intermittent pressure on the tragus. Barany noise box can also be used for masking.
- Now the examiner speaks spondee words (such as iceberg, sunlight, bathroom, housewife, suitcase) or numbers with letters (Y3G, 6BZ, K4D) and walks towards the patient. The distance at which this conversational voice is heard is measured.
- Then the examiner speaks spondee words in a whisper (with residual air after an ordinary expiration). The distance at which the whispered voice is heard is measured.
Interpretation:
- The patients with >30dB hearing loss are not able to hear a whispered voice at 2 feet from the test ear. (sensitivity of test is 95% and false-positive rates are 10%).
- If a patient is able to hear voice 2 feet away, the pure tone threshold is better than 30dB HL.
Disadvantage:
- The standardisation in intensity and pitch of voice used for testing is doubtful and the ambient noise may interfere with the test results.
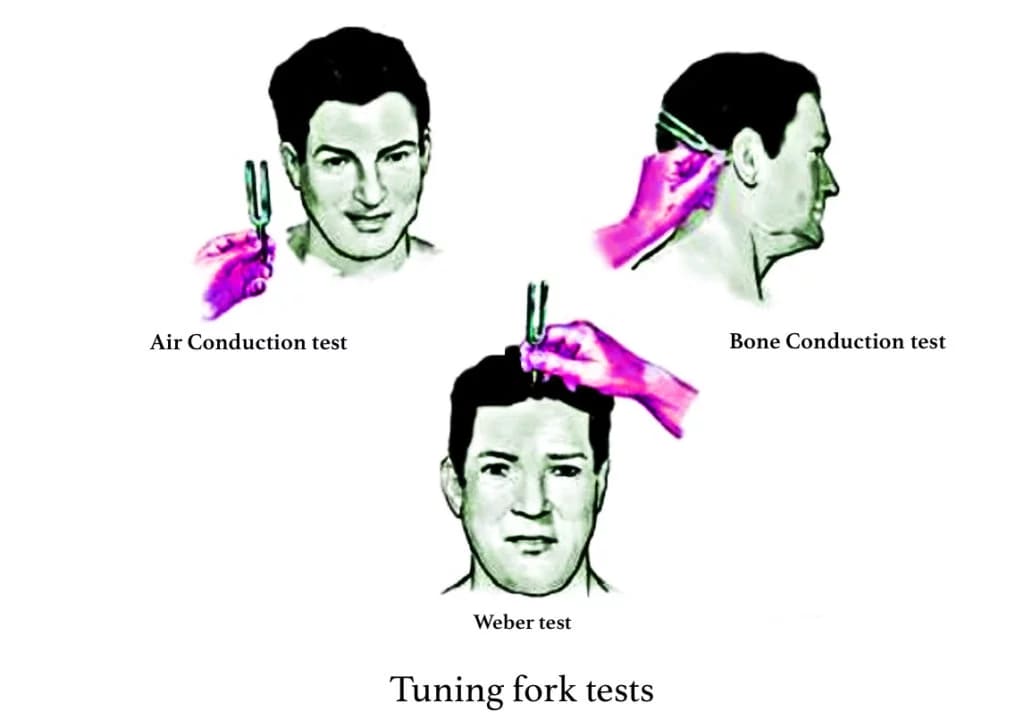
TUNING FORK TESTS
Selection of Tuning fork: Tuning forks of varying frequencies such as 128, 256, 512, 1024, 2048 and 4096 hertz are available in the market. In clinical practice, tuning fork of 512 Hz is considered ideal (Optimum decay time and produce minimal overtones). Shorter frequency forks are not preferred as they give a sense of bone vibration, while higher frequency forks are not preferred due to their shorter decay time.
Setting tunic fork into vibration :
- Hold tunic fork from its stem.
- To activate tuning fork, strike it gently against the examiner’s elbow, the heel of the hand or the rubber heel of the shoe.
- To produce a pure tone, strike the prong at a point 1/3rd of its length from its free end (this will minimize overtones and produce accurate results.)
Pre-requisites for tuning fork tests:
- Explain to the patient that he should raise his finger when he no longer hears the sound.
- The practitioner stabilizes the patient’s head with one hand.
To test air conduction (AC), a vibrating fork is placed vertically in line with the meatus, about 2 cm away from the opening of the external auditory canal. The sound waves are transmitted through the tympanic membrane, middle ear and ossicles to the inner ear. Thus, by the air conduction test, the function of both the conducting mechanism and the cochlea are tested. Normally, hearing through air conduction is louder and heard twice as long as through the bone conduction route.
To test bone conduction (BC), the footplate of the vibrating tuning fork is placed firmly on the mastoid bone. The cochlea is stimulated directly by vibrations conducted through the skull bones. Thus, BC is a measure of the cochlear function only.
The clinically useful tuning fork tests include:
- Rinne’s test. The base of a vibrating tuning fork is kept on the mastoid bone of the patient. When the subject indicates that he can’t hear the sound anymore, the tuning fork is brought 25 mm (2.5 cm) in front of external auditory canal, parallel to the acoustic axis. If he still hears the sound, it means air conduction is more than bone conduction. Alternatively, the patient may be asked to compare the loudness of sound heard through air and bone conduction.
Interpretation of Rinne’s test:
- Rinne’s positive. AC > BC. It is seen in normal persons or patients having sensorineural deafness.
- Rinne’s negative. BC > AC. It is seen in patients having conductive deafness.
- Rinne’s false negative is seen in severe unilateral sensorineural hearing loss. The patient is able to perceive the sound of vibrating tuning fork when placed on mastoid but not in front of the ear. This response is a transcranial transmission of sound to the contralateral healthy ear. To differentiate it from ‘true negative’, the non-test ear is masked with Barany’s noise box while testing for bone conduction. Also, confirmation can be aided by the Weber test which it is lateralized to the better ear.
A prediction of air-bone gap can be made if tuning forks of 256, 512 and 1024 Hz are used.
- A Rinne test equal or negative for 256 Hz but positive for 512 Hz indicates an air-bone gap of 20–30 dB.
- A Rinne test negative for 256 and 512 Hz but positive for 1024 Hz indicates an air-bone gap of 30–45 dB.
- A Rinne negative for all the three tuning forks of 256, 512 and 1024 Hz indicates an air-bone gap of 45–60 dB.
Remember that a negative Rinne for 256, 512 and 1024 Hz indicates a minimum AB gap of 15, 30, 45 dB, respectively.
2. Weber’s test in conjunction with Rinne’s test helps the clinical diagnosis, especially in unilateral hearing loss. Procedure: Place the vibrating tuning fork in the middle of the forehead/ vertex/ central incisors/ mandibular symphysis from where it will be conducted directly to the cochlea. Ask the patient in which ear, hearing is better.
Interpretation of weber’s test:
- Normally, it is heard equally in both ears.
- Lateralisation: It is lateralised to the worse ear in conductive deafness (this is due to loss of ambient noise or failure to dissipate sound because of the ossicular discontinuity). It is lateralised to the better ear in sensorineural deafness (as sound travels directly to the cochlea via bone).
3. Absolute Bone Conduction test. In this test, the bone conduction of the patient is compared with that of the examiner presuming that the examiner’s hearing status is normal. Procedure: The patient’s external auditory canal is blocked by the examiner by pressing over the tragus. Now place the vibrating tuning fork on the mastoid bone. When the patient indicates that he no longer hears the sound, the same tuning fork is placed on the mastoid bone of the examiner with ear occlusion same as done in the patient.
Interpretation of absolute bone conduction test:
- Normal subjects & Conductive deafness – The examiner does not perceive the sound which implies, both the patient and the examiner hear the sound for same time.
- Sensorineural deafness – The examiner is still able to hear the sound which implies, the patient was able to perceive the sound for a lesser duration.
4. Schwabach test. Bone conduction of the patient is compared with that of the normal hearing person (examiner) but in this test, the meatus is not occluded.
Interpretation of schwabach test: Same as absolute bone conduction test.
5. Bing Test: Place a vibrating tuning fork on the patient’s mastoid process. Alter the air pressure in the ear canal by closing/ opening the ear canal by alternatively pressing on the tragus. Ask the patient whether there is any increase or decrease in the sound of the vibrating tuning fork.
Interpretation of bing test:
- Normal or Sensorineural hearing loss – Patient hears louder when the ear canal is blocked and softer when the canal is not blocked (Bing positive).
- Conductive hearing loss – No such change in hearing is seen in patients with fixed or disconnected ossicular chain (Bing negative).
6. Gelle’s test. It is an excellent test for determining the functional status of the ossicular chain. Procedure: Place a vibrating tuning fork on the patient’s mastoid process. Alter the air pressure in the ear canal using a Siegel’s speculum. Ask the patient whether there is any increase or decrease in the sound of the vibrating tuning fork.
Interpretation of Gelle’s test:
- In normal subjects, raised air pressure in the ear canal by Siegel’s speculum will push the tympanic membrane and ossicles inwards. This will raise the intralabyrinthine pressure leading to immobility of the basilar membrane and thus reduced hearing.
- However, no such change in hearing is seen in patients with fixed or disconnected ossicular chain (conductive hearing loss).
TUNING FORK TESTS AND THEIR INTERPRETATION
| Test | Normal | Conductive deafness | SN deafness |
| Rinne | AC > BC (Rinne positive) | BC > AC (Rinne negative) | AC>BC |
| Weber | Not lateralized | Lateralized to poorer ear | Lateralized to better ear |
| ABC | Same as examiner’s | Same as examiner’s | Reduced |
| Schwabach | Equal | Lengthened | Shortened |
SPECIAL TUNING FORK TEST FOR MALINGERING / NON- ORGANIC DEAFNESS
1.Stenger’s test: It is based on the principle that if two equal/ identical sounds strike on the healthy ears, the individual hears it in only one ear – the one in proximity to the sound.
Procedure : The patient is blindfolded and the examiner holds two similar tuning forks (512) struck with moderate intensity and held at 25 cm from each ear. The malingerer hears in the normal ear only. The fork on the deaf side is advanced by 3 inches towards the ear. A malingerer does not hear the sound at all.
2. Chimani Moos test: This test is a modification of the Weber test to detect non-organic hearing loss. If a tuning fork is placed on the forehead, the malingerer states that he hears the sound in his good ear (simulating sensorineural deafness). If the meatus of the good ear is occluded, the truly deaf patient still hears the sound in the occluded ear but the malingerer will pretend that he is not able to hear the sound at all.
3. Teal test: It is used in patients who claim to hear only by bone conduction.
VOICE TESTS FOR MALINGERING / NON- ORGANIC DEAFNESS
- Erhard’s Test: Detects total unilateral hearing loss. In this test, the meatus of the normal ear is occluded. This attenuates speech by 30dB or less. The suspected malingerer is asked to close his eyes and repeat words heard. He is told that the normal meatus is being occluded and the examiner closes it by pressing the tragus. Words are then spoken in the suspected ear, failure to repeat the words indicates malingering since even with head shadow effect the other ear should be able to hear.
- Lombard’s Test: Based on the principle that an individual raises his voice when speaking in a noisy surrounding. The patient is asked to read prose. Noise is then applied to the good ear. If there is organic loss in the suspected ear then the voice level is raised, if feigned then normal monitoring is unimpaired and there is no change in speech.
AUDIOMETRY TESTS
- Pure Tone Audiometry (Gold standard).
- Speech Audiometry
- Bekesy Audiometry
- Impedance Audiometry
- Pure Tone Audiometry (Gold standard). PTA is a subjective test to measure the hearing threshold for pure tones (i.e., sinusoidal waves with a single frequency, amplitude & phase) using an instrument called audiometer. It is an electronic device which produces pure tones, the intensity of which can be increased or decreased in 5 dB steps. At each frequency, the threshold intensity is determined and charted in the form of a graph called audiogram.
An audiometer consists of following main parts:
- Electronic oscillator. It can generate pure tones of frequencies ranging from low to high.
- Intensity dial. It helps to adjust the threshold intensity of hearing for each tone.
- Headphone. It helps to deliver the pure tones of various frequencies to each ear separately.
Pre requisites:
- PTA should be performed in a sound-proof room (accepted level of ambient noise < 35 dB).
- Transient noises (sneezing, coughing or of any movement) should be avoided as it may interfere with the test results.
- The patient sits in a sound-proof booth and the examiner performs audiometry from outside the booth. They should be able to talk to each other through intercom or directly.
- The examiner and the patient should sit face-to-face so that the examiner is able to see the patient’s reactions (discomfort, state of confusion, not able to recognise sound etc).
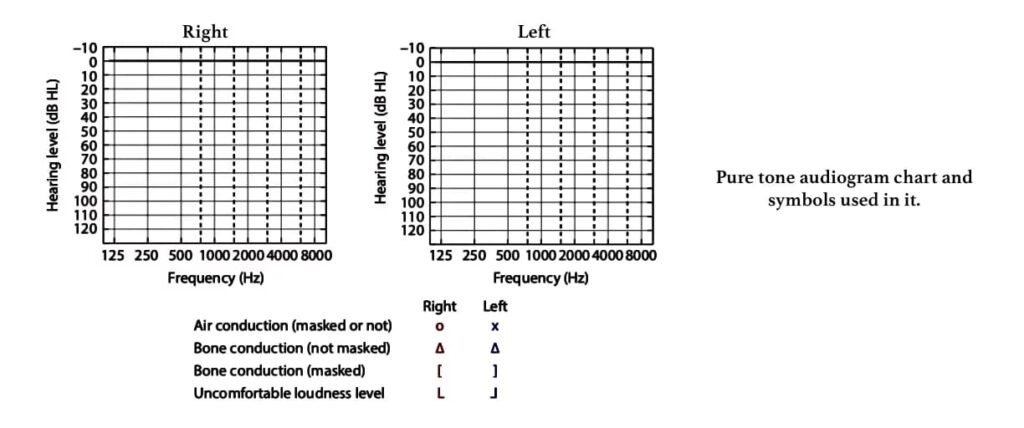
Procedure: The better ear is tested first. The threshold for each pure tone is measured in the order: 1000Hz, 2000Hz, 4000Hz, 8000Hz followed by 500Hz and 250Hz. In case the difference between contiguous frequencies is 20dB or more, inter-octave frequencies (750,1500,3000,6000 Hz) must be tested. Similarly, testing is done in the other ear. Testing is carried out by AC first and then, if necessary, by BC. Test frequencies for BC are those in the range 500–4000Hz, with no retest at 1000Hz required.
Bracketing technique/10dB down, 5dB-up technique/ descending-ascending technique: Each test signal is delivered at an audible level, followed by attenuation in volume(in 10dB steps) until the signal is inaudible. Then the signal is increased in steps of 5 dB until it becomes audible and the patient perceives.
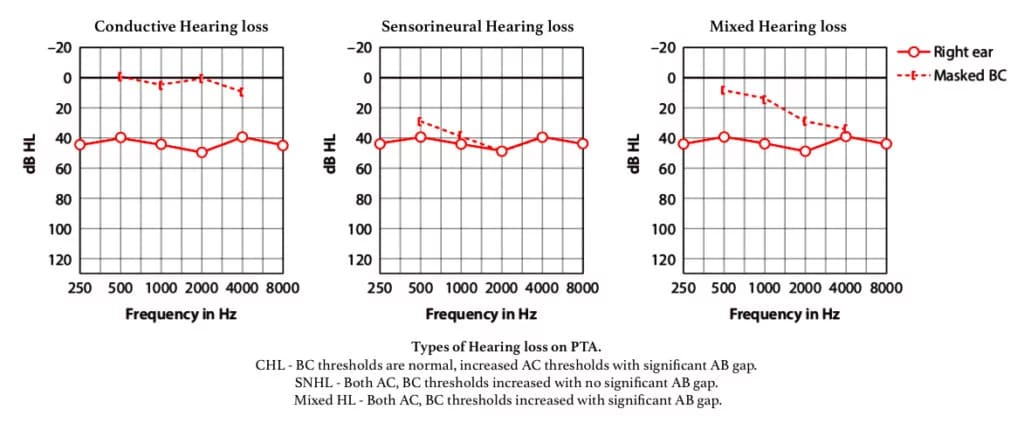
Pure Tone Audiogram is a graphic representation of hearing detection thresholds in each ear.
| MASKING. Masking is done to produce inaudibility of one sound by the presentation of another sound. During masking, one ear is kept busy by a narrow band noise when the other is being tested. Masking of the non-test ear is done in all bone conduction tests because BC signals are transmitted to both cochleae, regardless of the side on which the transducer is placed. However, for air conduction tests, a continuous masking noise (or masker) is required only when the interaural hearing difference (AB gap) exceeds 40 dB or more (when using supra or circum-aural headphones), or 55 dB or more (when using insert earphones). This is done to avoid transcranial transmission/ interaural attenuation/ cross-hearing and accurately measure hearing in each ear. |
Interpretation of PTA.
- Conductive hearing loss. There is a difference of more than 10dB between AC and BC thresholds at any frequency.
- Sensorineural hearing loss. The BC thresholds are raised above 20 dB HL.
- Mixed Hearing loss. If the BC thresholds are raised above 20 dB HL and there is a significant ABG, this is referred to as a ‘mixed’ hearing loss.
Utilisation of PTA:
- The primary purpose is to determine the type, degree, and configuration of hearing loss. AC pure tone audiogram is the primary test to measure the degree of hearing loss. BC pure tone audiogram aids in differentiating between conductive and sensorineural hearing loss. If the hearing loss for AC and BC is equal, it indicates a sensorineural lesion whereas AC > BC indicates a conductive lesion.
- PTA confirms the degree of handicap for medicolegal purposes.
- Audiogram is essential for accurate prescription of hearing aid.
- PTA determines speech reception threshold of the subject.
Disadvantages of PTA:
- It is a subjective test (results are based on the subject’s answers).
- PTA gives inaccurate results in case of a malinger.
- The results are not reliable in a child of age <7 years as it depends on cognitive development and cooperation.
2. Speech audiometry. It is a fundamental tool used to measure the patient’s hearing ability and comprehension of spoken words. The results are plotted on a graph. This test also aids in the detection of retrocochlear pathology and non-organic hearing loss.
Two parameters are studied in speech audiometry:
1. Speech reception threshold
2. Discrimination score.
- Speech Reception Threshold (SRT) or Speech-awareness threshold (SAT) is defined as the lowest speech intensity at which the patient correctly repeats or detects 50% of the words. Spondee words (two-syllable words with equal stress on each syllable such as pancake, hardware, playground) are delivered in the form of recorded tapes or monitored voice through the headphone of an audiometer or free field through speakers in a soundproof room. Spondees are easily understandable and contain information within each syllable that allows reasonably accurate guessing. The intensity is varied in 5 dB steps till half of them are correctly heard. In a normal adult, SRT is within 10 dB of pure tone average (500, 1000 and 2000 Hz). SRT better than pure-tone average by more than 10 dB suggests a functional hearing loss or unreliable pure tone audiogram.
- Speech discrimination score/ speech recognition/ word recognition score. It measures the patient’s ability to understand speech. A list of 25 – 50 phonetically balanced words (single-syllable words, e.g. pin, sin, day, bus) is delivered to each ear separately at 30–40 dB above his SRT, through pre-recorded material played from a computer/ CD and the percentage of words correctly heard by the patient is recorded. In normal persons and conductive hearing loss, a high score of 90–100% is achieved.
Table : Ability to understand speech and its relation to speech discrimination (SD) score. A list of 50 PB words is presented and the number correctly heard is multiplied by 2 the number
| SD score | Ability to understand speech |
| 90–100% | Normal (Excellent) |
| 76–88% | Slight difficulty (Good) |
| 60–74% | Moderate difficulty (Fair) |
| 40–58% | Poor |
| <40% | Very poor |
Patients with conductive deafness show improved recognition scores when the speech signal intensity is increased. Patients with sensorineural deafness usually do not improve their recognition scores with increasing intensity because increasing loudness distorts speech signal. Patients with retro-cochlear pathology may show a reduction of recognition scores with increasing intensity, a phenomenon described as the ‘rollover’ effect. The effect refers to the distortion in word recognition seen at high volumes, suggestive of eighth cranial nerve lesion. With increase in speech intensity above a particular level, the PB word score falls rather than maintain a plateau as in the cochlear type of sensorineural hearing loss.
Performance Intensity Function for PB Words
PB Max: It is better to plot PB scores against various levels of speech intensity on a chart and find the maximum score (PB max) a person can attain, instead of using a single suprathreshold intensity of 30–40 dB above SRT. The intensity of sound is noted at which PB max is attained. Maximum volume of hearing aid must be less than PB max.

Benefits of speech audiometry :
- To measure the speech reception threshold which determines actual disability & not hearing impairment.
- To differentiate organic from nonorganic(functional) hearing loss.
- To find the intensity at which a hearing aid/cochlear implants fits and assessing rehabilitation outcome.
- To differentiate a cochlear from a retrocochlear sensorineural hearing loss.
3. Bekesy Audiometry. It is self-recording audiometry based on sweep and fixed frequency testing, where various pure tone frequencies automatically move from low to high while the patient controls the intensity through a button. Two tracings, one with continuous and the other with the pulsed tone, are obtained. The tracings help to differentiate a cochlear from a retrocochlear and organic from a functional hearing loss. Bekesy audiometry is seldom performed these days.
Various types of tracings obtained are:
- Type I Continuous and pulsed tracings overlap. Seen in normal hearing or conductive hearing loss.
- Type II Continuous and pulsed tracings overlap up to 1000 Hz and then continuous tracing falls. Seen in cochlear loss.
- Type III Continuous tracing falls below pulsed tracing at 100–500 Hz even up to 40–50 dB. Seen in retrocochlear / neural lesion.
- Type IV Continuous tracing falls below pulsed lesion at frequencies up to 1000 Hz by more than 25 dB. Seen in retrocochlear/ neural lesion.
- Type V Continuous tracing is above pulsed one. Seen in nonorganic hearing loss.
4. Impedance Audiometry.
Impedance audiometry is an objective test used to assess middle ear function and mobility of the tympanic membrane. The word ‘impedance’ means resistance to the flow of acoustic energy, expressed in ohms. and compliance is expressed in cubic centimetre of air. It provides valuable otological and neurological information about the nature and site of a lesion. The middle ear functions as the ‘impedance matching device’. Any pathology in the middle ear may cause impedance mismatching and vary the amount of sound reflected back from the tympanic membrane leading to conductive deafness. Impedance audiometry measures the efficiency of the middle ear to perform this function.
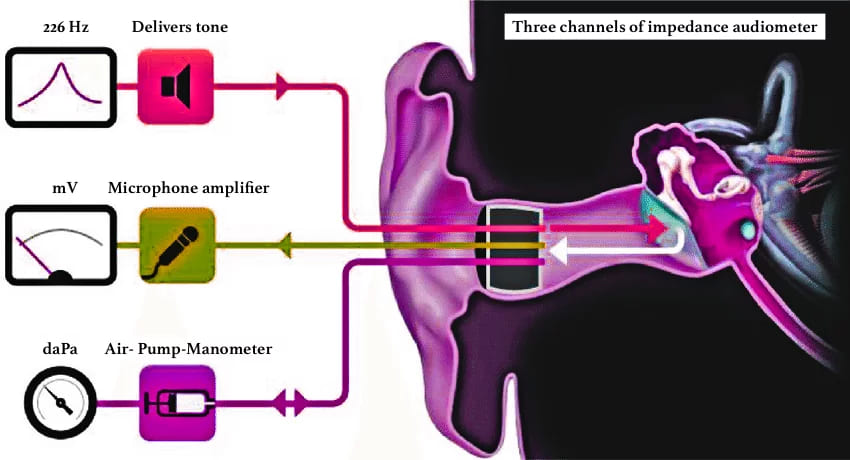
Impedance audiometer consists of a handheld probe which is hermetically sealed into the external auditory meatus forming a leak-free seal from the probe tip to the eardrum and has three channels: (i) first channel delivers a tone of 220 or 226 Hz, (ii) the second channel allows the reflected sound from the tympanic membrane to pass through a microphone amplifier assembly for processing (iii) the third channel is attached to air- pump-manometer system to bring about changes in air pressure in the ear canal from positive to normal and then negative(+300 to -600 mm of water pressure).
It includes:
(i) Tympanometry
(ii) Eustachian tube function test
(iii) Acoustic/ stapedial reflex measurements
(i) TYMPANOMETRY. (one of the acoustic immittance tests) is the measurement of the change of impedance in the middle ear due to varying air pressure in the sealed external auditory meatus. A non-compliant/ stiff tympanic membrane tends to reflect back more sound energy as compared to a compliant TM. This reflected sound pressure is measured at the tip of the probe and charted in the graphical form of with impedance of the middle ear/compliance of TM on Y-axis and the air pressure on X-axis, called the tympanogram.
| Impedance is the opposition/ resistance to the flow of energy, admittance is the ease of movement with which the flow of energy occurs. For ease of measurement most clinical impedance audiometers measure the acoustic admittance. Admittance is reciprocal of impedance just like compliance is the reciprocal of stiffness. |
Procedure:
1. Otoscopy is done to exclude scarring or perforation in the tympanic membrane
2. Remove wax /discharge, if present and choose a well-fitted ear probe tip to create an air tight seal.
3. Mild sedation may be used in un-cooperative patients and children.
4. A probe is inserted in the ear. Increase the pressure to +200 mm of H2O. Reduce the pressure serially to 100, 50, 0 up to 400 mm of H2O to test the compliance at various pressure. Draw a graph with pressure on the X-axis and compliance on the Y-axis. The normal middle ear pressure is ± 25 mm of H2O but for practical purposes ± 100 mm of H2O is taken as normal.
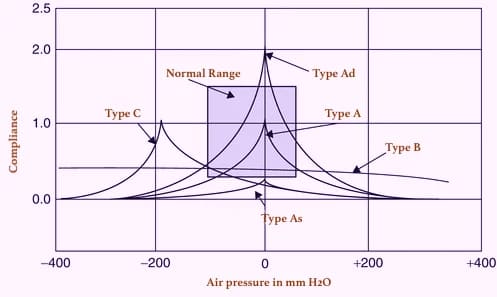
Types of tympanogram:
| Type A | Normal tympanogram (the peak is near zero pressure) |
| Type As | Compliance is lower at or near ambient air (zero) pressure. Hypo-mobile admittance is observed in otosclerosis, tympanosclerosis or malleus fixation. |
| Type Ad | High compliance at or near ambient pressure. Hypermobile admittance is observed in discontinuity of ossicular chain or thin, flaccid tympanic membrane. |
| Type B | A flat or dome-shaped graph. No change is seen in compliance with changes in pressure. This curve is seen in middle ear fluid, adhesive otitis media, thick or perforated TM, or grommet in situ. |
| Type C | Maximum compliance occurs with negative pressure in excess of 100 mm H2O. Seen in retracted tympanic membrane, fluid in middle ear. |
| Type D | A notched graph, seen in scarred and flaccid TM |
| Type E | An undulating graph, seen when 8000 Hz sound is presented . This is seen in thick grafts after myringoplasty or in any mass. |
(ii) EUSTACHIAN TUBE (ET) FUNCTION TEST. Tympanometry can be used to assess eustachian tube function and confirm the integrity of the auditory system. Eustachian tube dysfunction plays a dominant role in the pathogenesis of suppurative and non-suppurative otitis media. The prognosis and treatment of both types of otitis media are dependent upon the eustachian tube function. Tests which can be done are: (a) William’s test (b) Toynbee’s test (c) Acoustic immittance.
(a) William’s test. is done in an intact tympanic membrane. The impedance audiometer is programmed to measure the middle ear pressure in three conditions (i) the middle ear pressure at the beginning of the test (resting pressure), (ii) after swallowing (with the nose pinched and mouth closed) and (iii) after performing Valsalva.
Inference:
- Normal ET function: Middle ear pressure is same as atmospheric pressure at rest, during swallowing or Valsalva.
- Impaired ET function: Pressure becomes negative during swallowing. It does not become positive on Valsalva or vice versa.
- Grossly impaired ET function. Pressure does not change at all in either of the situations.
(b) Toynbee’s test. is done in patients having a perforation in the tympanic membrane or grommet-in -situ. The test is similar to William’s test where negative or positive pressure (−250 or +250 mm H2O) is created in the middle ear and the person is asked to swallow five times in 20 seconds. The test is carried out for a fixed duration of time, e.g., 40 seconds (minimum) or 160 seconds (maximum). The ability to equilibrate the pressure with every act of swallowing indicates whether the patient is having normal tubal function or not.
(c) Acoustic immittance can also measure the physical volume of air between the probe tip and the tympanic membrane. Normally it is up to 1.0 mL in children and 2 mL in adults. Any increase in volume >2 mL in children and >2.5 mL in adults indicate perforation of the tympanic membrane (because middle ear volume is added up to the volume of the external ear canal). This has also been used to find patency of the ventilation tube.
(iii) ACOUSTIC REFLEX. is based on the fact that a loud sound 70–100 dB above hearing threshold of one ear, causes bilateral contraction of the stapedius muscle (which pulls the stapes slightly outward and upward) & and tensor tympani muscle (pulls the tympanic membrane slightly inward). The effect is more pronounced on the stapedius muscle than on tensor tympani. Stapedial reflex threshold (SRT): Minimal intensity of sound that produces stapedial reflex. (bilateral reflex)
Reflex arc:
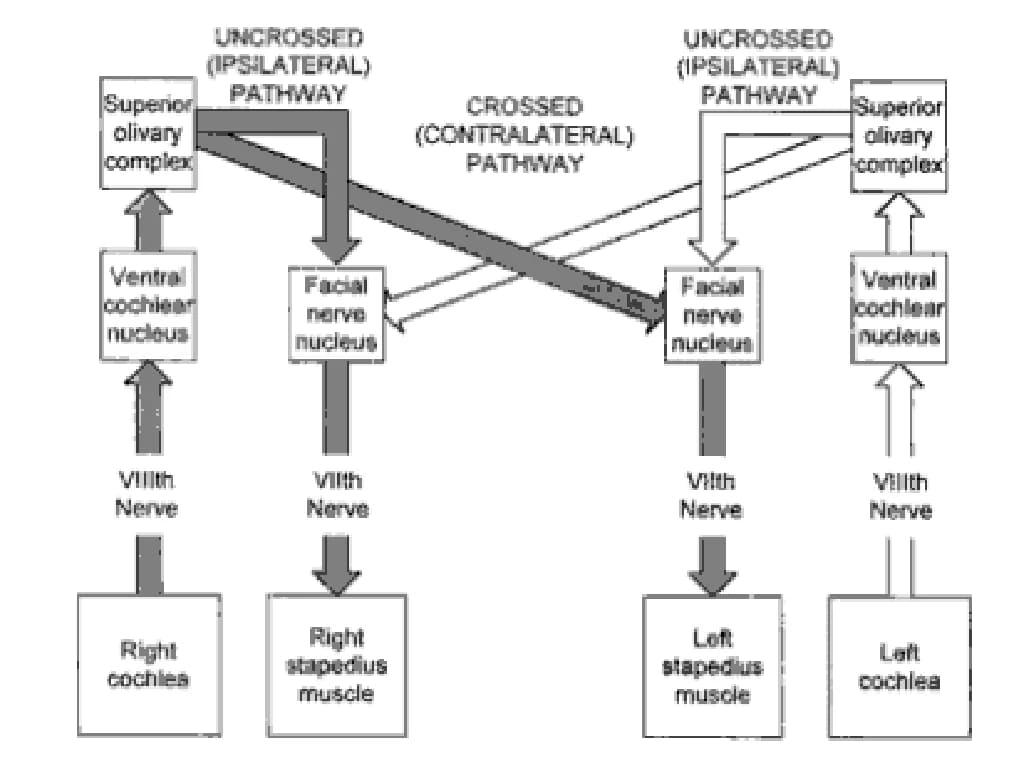
Ipsilateral ear: CN VIII → ventral cochlear nucleus → CN VII nucleus → ipsilateral stapedius muscle.
Contralateral ear: CN VIII → ventral cochlear nucleus → contralateral medial superior olivary nucleus → contralateral CN VII nucleus → contralateral stapedius muscle
Uses of acoustic reflex: It is very simple to perform, requires a few minutes, is a non-invasive objective test (does not depend upon subjective responses from the patient)
Acoustic reflex tests help the otolaryngologist/neurologist :
- To test the hearing in infants, young children and uncooperative patients.
- To assess middle ear function accurately.
- To differentiate cochlear and retro-cochlear pathology. In cochlear lesion, the stapedial reflex is present at lower intensities, e.g. 40–60 dB than the usual 70 dB(recruitment phenomenon)
- To detect brain-stem pathologies: If ipsilateral reflex is present but the contralateral reflex is absent, the lesion is in the area of crossed pathways in the brainstem.
- To detection non-organic hearing loss: A malingerer does not give any response on pure tone audiometry but shows a positive stapedial reflex.
- To identify the level of lesion in facial nerve paralysis: Absence of stapedial reflex when hearing is normal indicates a lesion of the facial nerve, proximal to the nerve to stapedius. The reflex can also be used to find prognosis of facial paralysis as the appearance of reflex after it was absent, indicates return of function and a favourable prognosis.
- To detect VIIIth nerve lesion: If a sustained tone of 500 or 1000 Hz, delivered 10 dB above acoustic reflex threshold, for a period of 10 s, brings the reflex amplitude to 50%, it shows abnormal adaptation and is indicative of VIIIth nerve lesion (stapedial reflex decay).
SPECIAL TESTS OF HEARING
- Recruitment
- SISI Test
- Threshold Tone Decay Test
- Auditory Evoked Potential
- Auditory Steady State Response (ASSR)
- Otoacoustic emmisions (OAE’s)
- Central Tests
1. Recruitment
A sound of a particular intensity becomes abnormally loud and intolerable to the patient. The low magnitude intensity sounds cannot be heard in the affected ear, it begins to hear high intensity sounds as loud or even louder than the normal hearing ear. Recruitment is commonly seen in patients with cochlear dysfunction. Such patients are poor candidates for hearing aids.
Alternate binaural loudness balance test is done to detect recruitment in unilateral cases. A tone, say of 1000 Hz, is played alternately to the normal and the affected ear and the intensity in the affected ear is adjusted to match the loudness in the normal ear. The test is started at 20 dB above the threshold of deaf ear and then repeated at every 20 dB rise until the loudness is matched or the limits of audiometer reached. In conductive and neural deafness, the initial difference is maintained throughout while in cochlear lesions, partial, complete or over-recruitment may be seen
2. Short Increment Sensitivity Index (SISI). A small change in the intensity of pure tone is better appreciated by the patient with cochlear lesions than normal subjects or patient having conductive or retro cochlear dysfunction. Hence this test may be used to differentiate cochlear and retro-cochlear lesion.
Procedure: A continuous, supra-threshold tone (20 dB above the hearing threshold) is given to the patient for 2 minutes. Thereafter, the tone is raised by 1 dB every 5 seconds and 20 such tones are given. The patient is instructed to count the number of tones heard.
- In conductive deafness. SISI score < 15%
- In nerve deafness – 0–20%
- In cochlear deafness – 70–100%
Disadvantages: The patients having severe deafness (above 85 dB) cannot be tested with most clinical audiometers. It requires active cooperation of the patient.
3. Threshold Tone Decay Test. This test is used in audiology to detect ‘decibels of delay’ and measure the auditory nerve fatigue. In a person with normal hearing, a tone whose intensity is only slightly above their absolute threshold of hearing can be heard continuously for 60 seconds. However, a patient of nerve fatigue is unable to hear for the entire 60 sec, the tone stops hearing earlier.
A tone at a frequency of 4000 Hz is presented for 60 sec at intensity 5 dB above the patient’s hearing threshold. If the patient stops hearing the tone before 60 sec has elapsed, the intensity level is raised by another 5 decibels. The procedure is repeated till the patient is able to hear the tone continuously for 60 s, or no level exists above the threshold where the tone is audible for full 60 seconds. The resultant measure gives as the decibels of decay.
Interpretation: A decay of between 15 and 20 decibels is indicative of cochlear hearing loss. A decay more than 25 dB is diagnostic of a retro-cochlear lesion.
4. Auditory Evoked Potentials. It records the potentials from the auditory pathways in response to a brief auditory stimulation using special equipment with an averaging computer. Though several components of evoked electric response have been reported only two have gained clinical acceptance.
(i) Electrocochleography (EcoG): It measures the summated intracellular potentials of the outer hair cells seen in response to an auditory stimulus. The electrical response is either due to cochlear microphonic potentials(electrical activity in the cochlea), summating potentials(a complex measurement of many electrophysiological parameters taken together) or electrical activity due to action potential of 8th nerve. It is an objective test that provides a reasonably accurate measurement of the hearing threshold between 1000 to 8000 Hz. No masking in the contralateral ear is required.
Procedure: The electrical activity can be detected by inserting a needle-like thin, active recording electrode through the tympanic membrane and placing onto the promontory or round window. The reference and ground electrodes are placed on the mastoid process and on the forehead respectively. It is usually done under sedation or local anaesthesia.
Uses of EcoG:
- To diagnose Meniere’s disease.
- To detect hearing threshold in the young infants and children within 5–10 dB
- To differentiate cochlear lesions from eighth nerve lesions.
- To monitor cochlea and cochlear nerve during neurotological surgical procedure.
(ii) Brainstem auditory evoked response (BAER) or BERA (brainstem evoked response audiometry). It is an objective, non-invasive test to assess the structural integrity and functional status of the auditory pathway from the spiral ganglia to the level of the lateral lemniscus in the midbrain. The test was introduced by Jewitt & Williston.
Principal : The series of electrical potentials generated by the activation of different parts of the auditory system are recorded by placing electrodes on the scalp. But since these cortical potentials are small and buried in the background of spontaneous electrical activity (EEG waves), an amplifier is required to study the waves in detail.
Procedure :
- The test is conducted in a sound-proof room.
- The patient is asked to be in a supine posture with eyes closed, relaxed and preferably asleep(to reduce myogenic potentials). However, accurate assessment in children may require sedation.
- Test one ear at a time.
- Three surface electrodes are used:
- Active electrode kept on the vertex (best location) and if not possible may be placed on the lop of the forehead just below the hairline.
- Reference electrode kept on ear lobe/mastoid of the tested ear.
- Ground electrode kept on ear lobe/mastoid of the opposite ear.
- The electrical potentials generated in response to a series of 1000-1200 clicks (given at a rate of 5-50/sec) at an intensity of 50 to 60dB above the average pure tone hearing level are picked up from the vertex by the active electrode and is plotted graphically.
- These neurogenic potentials elicited are recorded for the first 10 milliseconds. This is the time taken for the electrical responses to be carried to the brainstem alone
- In a normal person, seven waves are produced in the first 10-15 milliseconds. The first, third and fifth waves are most stable and are used in measurements.
Characteristics of waves:
- Latency – absolute, inter-wave (usually between wave i and v) and interaural.
- Absolute latency is the time interval (in millisec) between the onset of the stimulus and the peak of the wave. The absolute latency of the wave V is most important, as it is common, easily identifiable and is least affected when intensity increases.
- lnterwave latency is the time interval between two different waves in the same ear and in the same BERA tracing.
- Interaural latency is the difference in the time interval of the same wave between the two ears e.g. the latency of wave IV of left ear and right ear
Upper limits of normal values
- Latency of wave V – 5.9 m.s.
- I – V interval – 4.4 m.s.
- I – V interaural difference – 0.29 m.s.
| Wave I | Distal part of CN VIII |
| Wave II | Proximal part of CN VIII near the brainstem |
| Wave III | Cochlear nucleus |
| Wave IV | Superior olivary complex |
| Wave V | Lateral lemniscus |
| Waves VI and VII | Inferior colliculus |
Remember as mnemonic EE COLI (eight, eight, cochlear nucleus, olivary complex, lateral lemniscus, inferior colliculus) compare E COLI-MA in pathways of hearing.
Uses:
- Objective hearing assessment test in infants, young children, non-cooperative adults, in malingerers, comatose and unconscious patients.
- To diagnose the site of lesion in retro cochlear pathologies particularly acoustic neuroma.
- To diagnose brainstem pathology, e.g. multiple sclerosis or pontine tumours.
- To monitor and preserve the auditory nerve intraoperatively during surgery of acoustic neuromas
Disadvantages :
- There is no standardisation at present for BERA.
- Wave V is not recorded if the hearing level is 75 dB at 3 kHz.
- Normally, the latency of wave V increases in old age, conductive hearing loss and pure sensorineural hearing loss.
- Wave I is not easily identifiable in BERA.
Limitations :
- ABR testing is highly sensitive(90 %) for detecting large tumours; however, small tumours (<1 cm) may be missed. MRI is a more sensitive and specific test for an acoustic neuroma.
- ABR waves are usually absent when a patient has a severe or profound hearing loss.
- A conductive hearing loss also attenuates cochlear stimulation and increases ABR wave latencies.
- It does not give frequency-specific information. Low-frequency hearing losses are undetectable by the BERA. Hence additionally ASSR is needed.
- The test is practically insensitive for hearing losses above 75·dB.
- This test can only be done on awake, conscious and cooperative adult patients. It can be done in infants and young children under sedation as the latter has no effect on BERA.
5. Auditory Steady State Response (ASSR)
It is an electrophysiological test to predict the frequency-specific hearing thresholds. The steady-state pure tone signals(modulated in amplitude and frequency) are used in ASSR unlike, the transient signals of tone bursts or clicks used in ABR producing a frequency-specific audiogram.
Uses :
- Hearing loss of more than 80 dB can be detected. It can help in the early detection of the children who need cochlear implantation.
- ASSR can be done in all ages, any mental state, any degree of hearing loss.
- Multiple frequencies can be assessed at the same time, as long as their carrier frequencies utilize different modulation rates.
- ASSR is an objective test that can be analysed and interpreted easily using statistical methods.
6. Otoacoustic Emissions (OAEs). An ever-evolving, fast, easy to obtain, minimally-invasive screening test, used for screening for hearing loss in early life. OAE tests play an important role in monitoring ototoxicity and noise-induced hearing loss (NIHL) because OAEs can detect outer hair cell dysfunction earlier than a pure tone audiogram can.
Pathophysiology: OAE are the sounds of low intensity produced by the outer hair cells of a normal cochlea and recorded from the external auditory canal with the help of a sensitive microphone placed in the external ear canal. The sound produced by the outer hair cells travels in a reverse direction: outer hair cells → basilar membrane → perilymph → oval window → ossicles → tympanic membrane → ear canal.
OAEs are present in healthy outer hair cells, thus helps to test the functional status of the cochlea. OAE’s are absent in 50% of normal individuals, lesions of the cochlea, middle ear disorders (as sound travelling in the reverse direction cannot be picked up) and when the hearing loss exceeds 30 dB.
Types of OAEs:
(i) Spontaneous OAE’s are seen in the persons with normal hearing or when hearing loss < 30 dB.
(ii) Evoked OAE’s. Depending on the sound stimulus used, evoked OAE may be:
- Transient evoked OAEs (TEOAEs): A series of click stimuli are presented at 80–85 dB SPL (sound pressure level) and the response is recorded. TEOAEs can be recorded from 500–4000Hz but are more sensitive for hearing loss at 500 and 1000 Hz.
- Distortion product OAEs (DPOAEs): Two continuous tones of moderate-intensity, e.g. 55 and 65dB SPL, are presented to the cochlea at the same time to produce distortion. They are used to test hearing in the range of 1000–8000 Hz but have a better clinical performance for hearing loss at 4000 Hz.
Uses of OAE’s
- OAEs is used to distinguish between deafness caused by cochlear and retro-cochlear lesions. OAEs are absent in cochlear lesions, e.g. ototoxic sensorineural hearing loss.
- DPOAEs may be used to monitor ototoxicity effects earlier than pure tone audiometry.
- It may also be used in non-cooperative or mentally unwell patients, in non-organic hearing loss after giving sedation. Sedation does not affect OAEs.
Disadvantages:
- It is advisable to do tympanometry with OAEs because the middle ear pathology may interfere with the recording of OAEs. There are chances that the clinicians may misinterpret the absence of OAEs as a sensorineural hearing loss if they are unaware of the existence of middle ear pathology.
- OAEs may not diagnose the auditory neuropathy in the neonates. Auditory neuropathy is a hearing disorder characterized by abnormal or absent auditory brainstem response in the presence of normal outer hair cell function. Therefore, AABR is the best method in the NICU/SCBU population to detect auditory neuropathy.
OAE test results are affected by the ambient noise level and the patient’s internal noise level (e.g. breathing or body movements. Therefore, the results of OAE tests should be interpreted in conjunction with pure tone audiometry, tympanometry etc.
7. Central Auditory Tests, Auditory processing disorder, Central deafness
The patients with the central auditory pathology have difficulty in hearing a distorted, unclear speech and also when there is some background noise like in a party. They have normal pure-tone hearing thresholds and other hearing tests but cannot follow instructions. These problems are due to poor processing of the auditory cues in the higher auditory pathways.
Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests Assessment of hearing – Hearing tests
Types of speech discrimination tests :
- A message is presented in a distorted speech. Patients with cortical lesions will face difficulty in understanding the message.
- Two different speech messages (a pair of spondaic words along with digits or nonsense words) are presented at the same time, one to each ear and the patient is asked to identify both. The patients with temporal lobe lesions will have difficulty identifying these words when presented to the ear opposite to that of the side of the lesion.
- Binaural tests. They are used to identify the integration of information from both ears. Such tests are normal in cortical lesions but affected in lesions of brainstem and thus help to localize the site of the lesion. A most common test used is the binaural masking level difference test.
——— End of the chapter ———
Learning resources.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Susan Standring, Gray’s Anatomy.
- Ganong’s Review of Medical Physiology.
Author:

Dr. Rahul Kumar Bagla
MS & Fellow Rhinoplasty & Facial Plastic Surgery.
Associate Professor & Head
GIMS, Greater Noida, India
msrahulbagla@gmail.com
Please read. Glomus Tumour. https://www.entlecture.com/glomus-tumour/
Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
Join our Facebook group: https://www.facebook.com/groups/628414274439500
