Submandibular Gland Surgery
It is a surgical procedure that involves the surgical removal of the submandibular salivary gland.
Click here to: Read Anatomy of the Submandibular Glands

Anatomy Relevant to Submandibular Gland Surgery
| Structure | Relations | Key Points for Surgery |
|---|---|---|
| Submandibular gland | Lies in the submandibular triangle, superficial to mylohyoid muscle, deep to platysma | Divided into superficial & deep lobes separated by mylohyoid muscle; the duct (Wharton’s) runs forward beneath the tongue. |
| Marginal mandibular branch of facial nerve (MMB FN) | Runs below lower border of mandible anterior to angle, loops over facial artery/vein, supplies muscles of lower lip | Risk of injury during skin incision / flap elevation. |
| Lingual nerve | Deep to submandibular duct, passes over hyoglossus, under mucosa of tongue | Must be identified / protected when dissecting duct or submandibular ganglion. |
| Hypoglossal nerve (CN XII) | Deep to posterior belly of digastric, over hyoglossus, supplies tongue muscles | Risk during deep dissection, especially inferior & posterior aspects. |
| Submandibular (Chorda tympani / ganglion) | Parasympathetic to gland via ganglion; runs with lingual nerve | Needs careful separation during gland removal. |
| Facial artery & vein | Facial artery crosses inferior border of mandible just anterior to masseter, enters gland; facial vein is posterior or lateral | Must ligate facial vessels; useful landmarks for MMB FN. |
Indications
- Recurrent or chronic sialadenitis not responding to conservative therapy.
- Sialolithiasis (stones) causing obstruction, pain, swelling, and repeated infection.
- Benign tumours (most common: pleomorphic adenoma)
- Malignant tumours (e.g., mucoepidermoid carcinoma, adenoid cystic carcinoma).
- As part of a selective, modified, radical neck dissection to remove lymph nodes in level I of the neck
Contraindications
- Known high-grade malignancy
- Bleeding disorder
- Acute infection of the gland
- Stones confined to the distal portion of Wharton’s duct
Steps of submandibular gland surgery
- Patient position & Anaesthesia. The patient lies supine with the face turned away from the operative side, neck slightly extended (shoulder roll). General anaesthesia with oral endotracheal tube.
- Skin Incision. A horizontal incision is made at least 2 cm below the inferior border of the mandible, ideally in a natural skin crease. The length of the incision should be 3-4 cm.

- Flap elevation & Protection of the Marginal mandibular branch of the facial nerve. The marginal mandibular branch of the facial nerve enters the neck 1cm in front of the angle of the mandible, loops over the facial artery and vein 2cm below the lower border of the body of the mandible, before sweeping superiorly to the angle of the mouth.
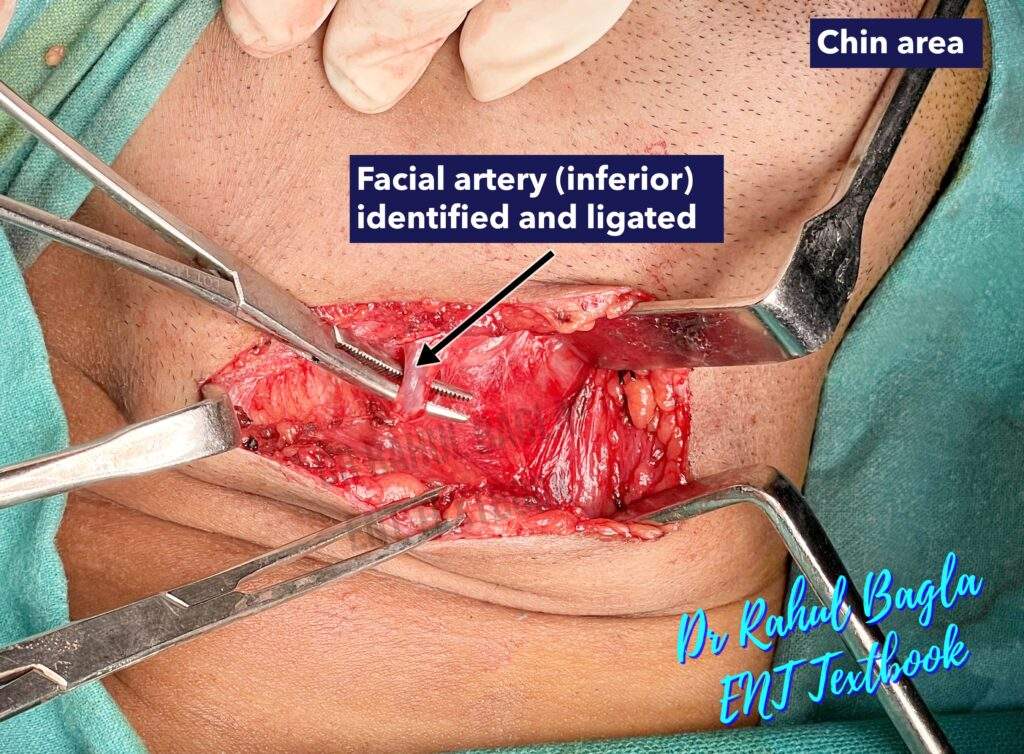
Generally, the submandibular gland is removed without the identification of the marginal mandibular nerve to avoid its injury. For this, a superior subplatysmal flap is not raised as the marginal mandibular branch of the facial nerve runs in the same tissue plane. Elevation of the subplatysmal flap superiorly may cause inadvertent injury to the nerve and cause paresis in the postoperative period. - Identification and Ligation of facial vessels. Dissection is initially directed to the inferior surface of the gland and proceeds cautiously along the capsule from inferior to superior until the facial vessels are ligated and reflected superiorly (subcapsular flap is elevated). The marginal mandibular nerve lies lateral to the facial vessels and can then be lifted out of the operative field by traction.
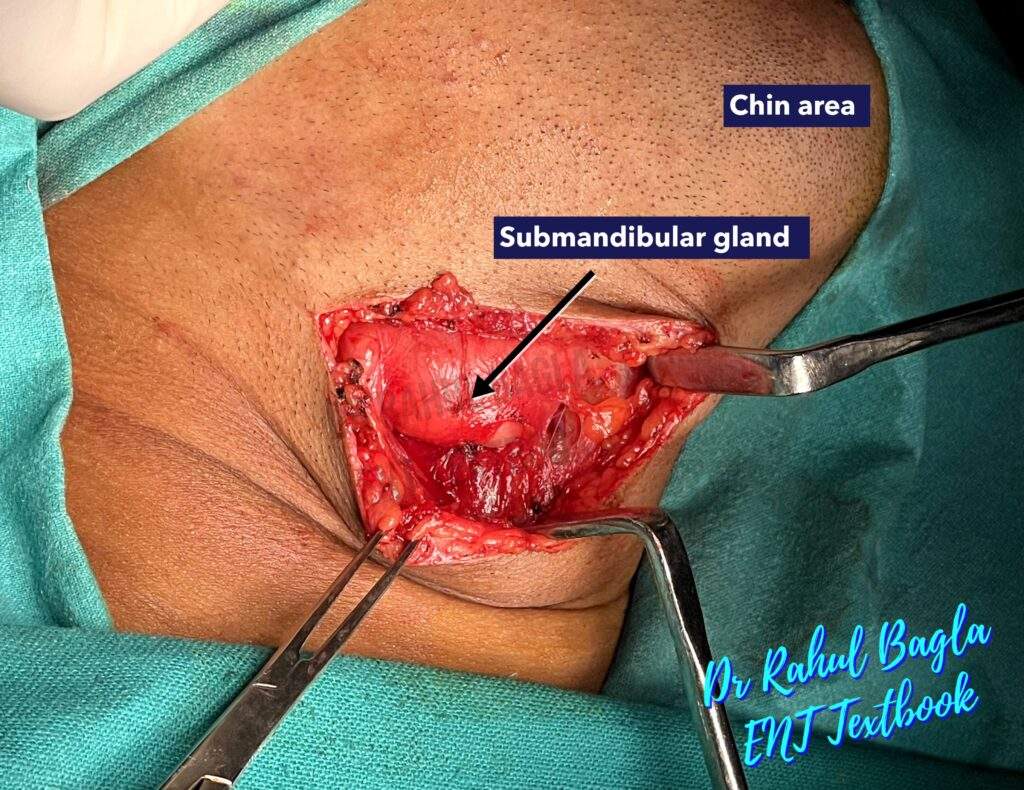
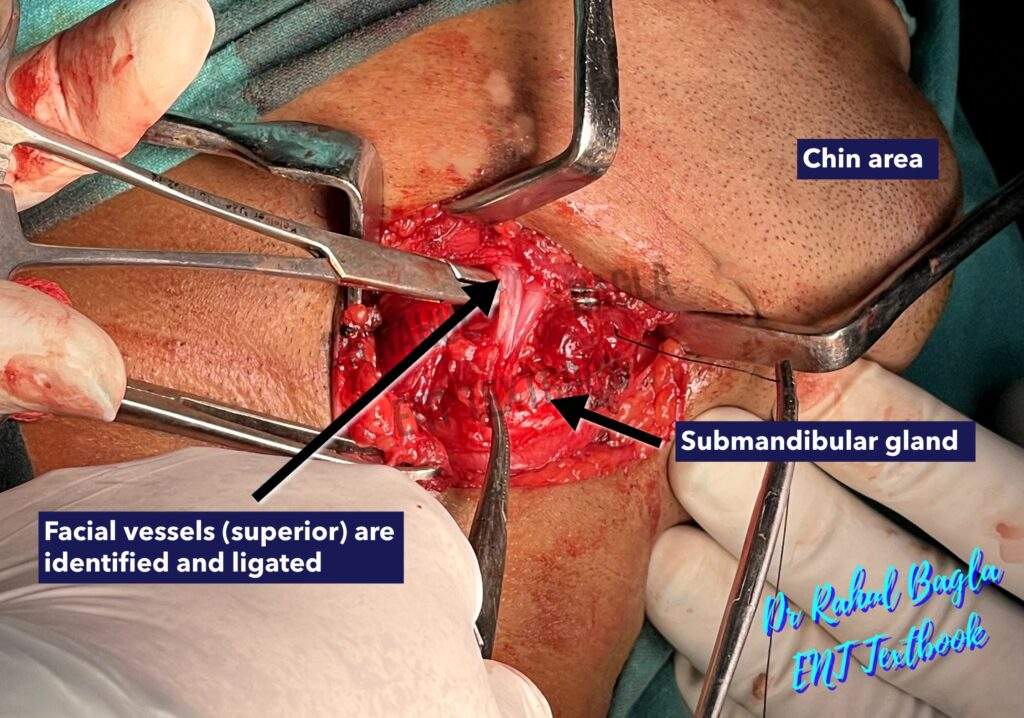
- Dissection of deep structures. Identify the digastric muscle (posterior belly) as a landmark. Retract posterior belly of digastric; maintain plane over mylohyoid muscle.
- Identification of the hypoglossal nerve. During inferior dissection, keep the dissection along the capsule over the digastric muscles to prevent injury to the hypoglossal nerve, which runs deep to the digastric muscles. The submandibular gland is pulled superiorly to expose the course of the hypoglossal nerve. The nerve runs on the surface of the hyoglossus muscle.

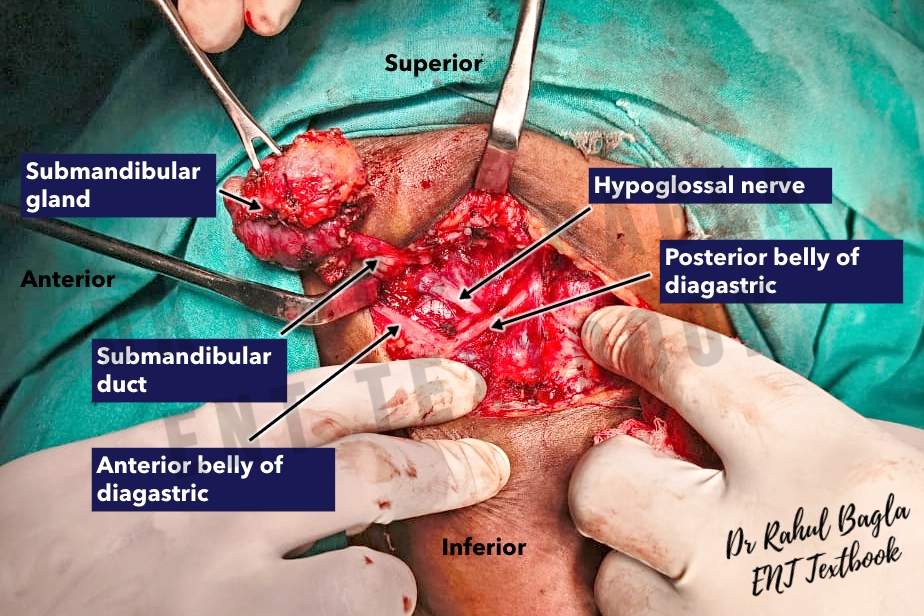
- Identification of the lingual nerve and submandibular ganglion. The posterior border of the mylohyoid muscle is retracted anteriorly, and the submandibular gland is pulled inferiorly, which draws the lingual nerve inferiorly into the field of dissection. The lingual nerve appears as a ribbon-like V-shaped band loosely attached to the body of the gland. The submandibular ganglion is surgically identified as the attachment point of the gland to the lingual nerve. The lingual nerve is then separated from the gland by sharp dissection through the fibres (the parasympathetic secretomotor supply) attached from the submandibular ganglion to the submandibular gland (submandibular duct mainly). This causes the lingual nerve to move upwards automatically and out of the surgical field.

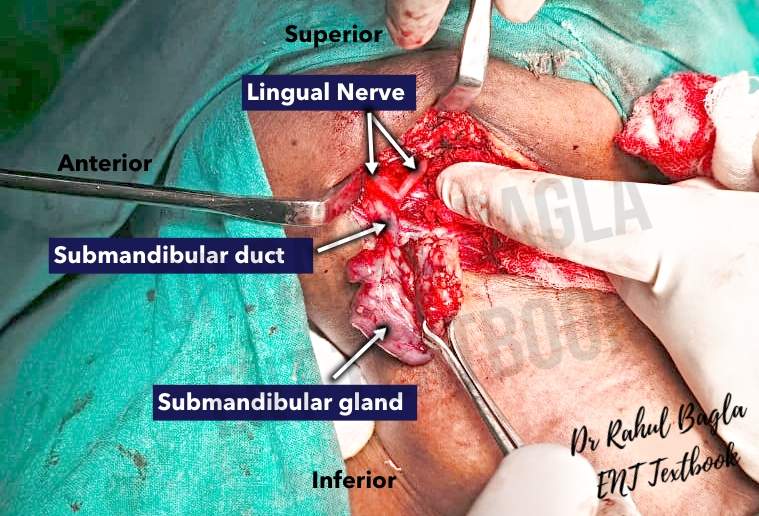
- Identification of the submandibular (Wharton’s) duct for ligation. The posterior border of the mylohyoid muscle is retracted anteriorly, and the submandibular gland is pulled posteriorly to identify the submandibular duct on tension. The submandibular gland duct is covered by the sublingual gland and should be separated before tying it. It is important to palpate the submandibular gland duct to ensure there are no stones in the duct. The duct is then divided and tied off. Then the gland is removed.
- A small vacuum drain is inserted and brought out through the skin posteriorly. The wound is closed in two layers (deep fascia, platysma/skin).
Complications
- Marginal mandibular nerve injury. Occurs temporarily in 10–15% of cases and permanently in 1–3% (PMC). Caused by injury during flap elevation, use of electrocautery, or nerve traction. Leads to lower lip asymmetry, drooling, and cosmetic dissatisfaction.
- Lingual nerve injury. Seen in 1–4% of surgeries (PMC). Occurs during duct dissection or separation of the submandibular ganglion. May result in altered tongue sensation or taste disturbance.
- Hypoglossal nerve injury. Very rare, with less than 2% incidence (PMC). Results from deep dissection near the posterior belly of the digastric or excessive traction. Long-term effects include tongue deviation, speech difficulty, and swallowing issues.
- Retained stone in the distal portion of Wharton’s duct. Seen in 15–20% of sialolithiasis surgeries (PMC). Caused by failure to detect or remove distal duct stones. Leads to recurrent pain, swelling, or infection.
- Bleeding and hematoma
- Infections are rare; antibiotics are only used preoperatively if history of sialadenitis
——– End of the chapter ——–
Download the full PDF Link:
Submandibular Gland Surgery Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Cummings, Otolaryngology-Head and Neck Surgery.
- Stell and Maran’s, Textbook of Head and Neck Surgery and Oncology.
- Ballenger’s, Otorhinolaryngology Head And Neck Surgery
- Susan Standring, Gray’s Anatomy.
- Frank H. Netter, Atlas of Human Anatomy.
- B.D. Chaurasiya, Human Anatomy.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery.
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Ganong’s Review of Medical Physiology.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Steps of submandibular gland surgery, Marginal mandibular nerve injury, Lingual nerve injury, Hypoglossal nerve injury, Retained stone in the Wharton’s duct.

Good.
Nice
Hello Dr. Hakeem Yousef! 🙏
Thank you so much — it truly means a lot! I’m very happy to hear that you found the chapter helpful. It’s always a pleasure to know that the work is reaching and supporting fellow medical professionals. Please don’t hesitate to reach out if you ever have questions. Wishing you continued success!
Warm regards,
Dr. Rahul Bagla
Dear Dr.
Nicely explained the surgical excision of submandibular gland. One thing I want to say, if I go through intracapsular dissection (in benign disease), it is possible to save the facial vessels. Otherwise, it’s fine. In some videos, I have seen somebody is raising the upper flap upto the margin of mandible, identifying the marginal mandibular nerve & then doing all the dissensions.
Thanks & regards.
Hello Mohammed Sirazul Islam
Yes, some surgeons prefer to elevate the subplatysmal flap up to the inferior margin of the mandible to identify the marginal mandibular nerve before proceeding with dissection. The nerve can typically be located just above and anterior to the posterolateral edge of the mandible (gonion point). Visual identification of the marginal mandibular nerve prior to dissection is advisable, as it helps reduce the risk of injury.
Both approaches are acceptable; however, actively searching for the nerve carries a higher chance of inadvertent trauma. Additionally, excessive or high elevation of the subplatysmal flap can risk injuring the nerve and lead to postoperative paresis. Ultimately, the choice of technique depends on the surgeon’s preference and experience.
Regards
Dr Rahul Bagla