Anatomy of Internal ear.
The internal ear, also called the labyrinth, is a crucial organ responsible for hearing (via the cochlea) and balance (via the vestibular system). It is one of the most protected structures in the body, safely enclosed within the petrous part of the temporal bone.
Location & Connections
- Location: The internal ear is positioned between the middle ear and the brain, deep within the skull.
- Connections to the Middle Ear: It connects to the middle ear through two small openings:
- The oval window (fenestra vestibuli) – where sound vibrations from the stapes enter the cochlea.
- The round window (fenestra cochleae) – allows pressure release from the cochlear fluid movements.
- Connections with the Brain: It communicates with the brain through two key pathways:
- The internal acoustic meatus transmits the cochlear nerve (for hearing) and the vestibular nerve (for balance) to the brainstem.
- The cochlear aqueduct is a small canal involved in fluid regulation. It connects the scala tympani of the cochlea to the subarachnoid space.
- Vestibular Aqueduct: This canal transmits the endolymphatic duct and sac towards the posterior cranial fossa.

Functions of the Inner ear.
1. Hearing (Auditory Function): The cochlea is the primary organ for hearing. The cochlea is responsible for the transduction of mechanical energy into electrical signals that can then be passed to the brain along the auditory or vestibular nerves. Movements of the stapes footplate are transmitted to the cochlear fluids, which move the basilar membrane and set up a shearing force between the tectorial membrane and the hair cells. The distortion of hair cells gives rise to electrical potentials (e.g., cochlear microphonics), which trigger the nerve impulse, which is then transmitted to the brain for interpretation as sound.
2. Balance (Vestibular Function): The internal ear is also responsible for maintaining balance by detecting position and motion. The vestibular system, comprising the semicircular canals and the vestibule (which includes the otolithic organs, specifically the utricle and saccule), is responsible for detecting head position and motion. The semicircular canals detect angular (rotational) acceleration (e.g., head turns), while the utricle and saccule detect linear acceleration (e.g., forward/backwards movement, gravity). These organs then send nerve impulses via the vestibular nerve to the brain, contributing to posture, gaze stability (vestibulo-ocular reflex), and spatial orientation.
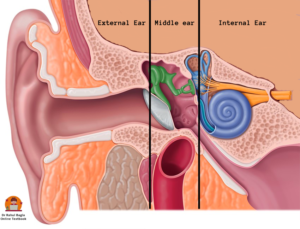
Parts of the Inner ear. The internal ear is divided into parts:
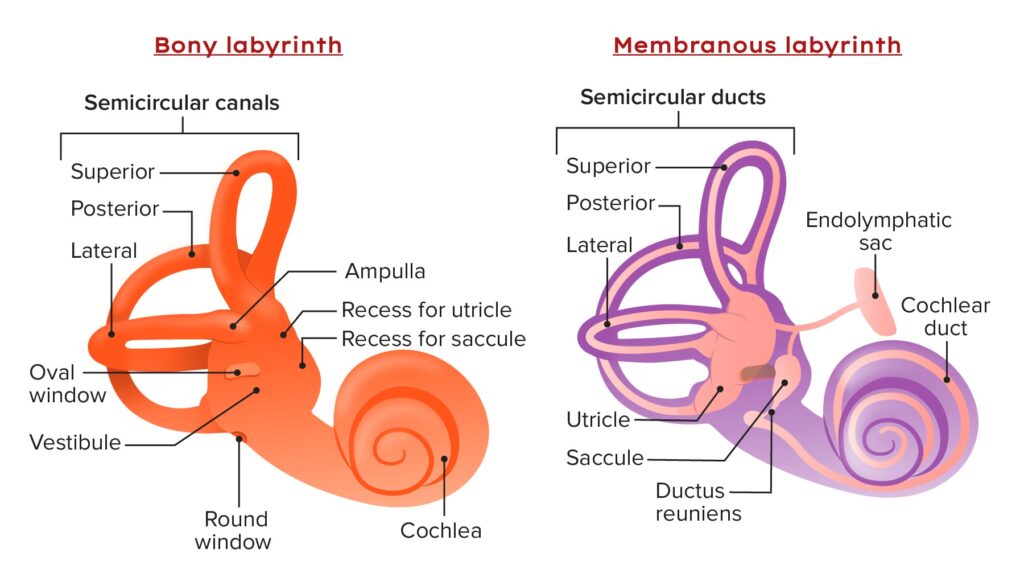
1. Bony labyrinth – A rigid, protective outer shell is filled with perilymph. It consists of:
- Cochlea
- Bony vestibule
- Three semicircular canals.
2. Membranous labyrinth – A delicate structure inside the bony labyrinth, which is filled with endolymph and houses the sensory receptors (hair cells). It consists of:
- Cochlear duct (inside the cochlea)
- Utricle and saccule (inside the bony vestibule)
- Three semicircular ducts (inside the semicircular canals)
- Endolymphatic duct and sac.
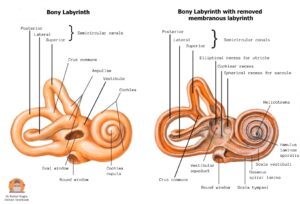
BONY LABYRINTH.
The bony labyrinth develops from the mesoderm that surrounds the membranous labyrinth which first ossifies into cartilage and then ossifies into the bone to form the bony labyrinth. This process is called as enchondral ossification.
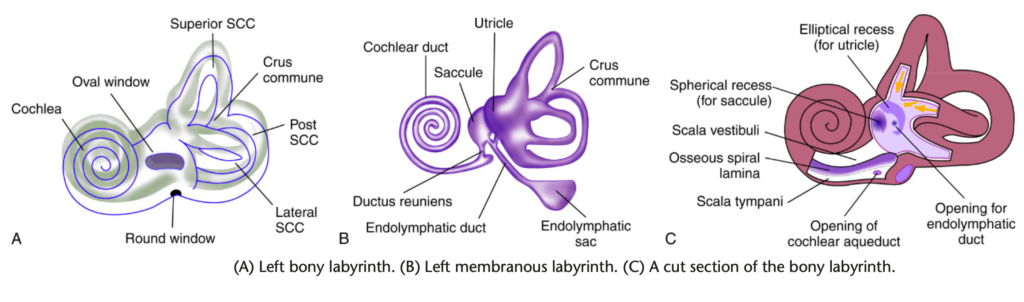
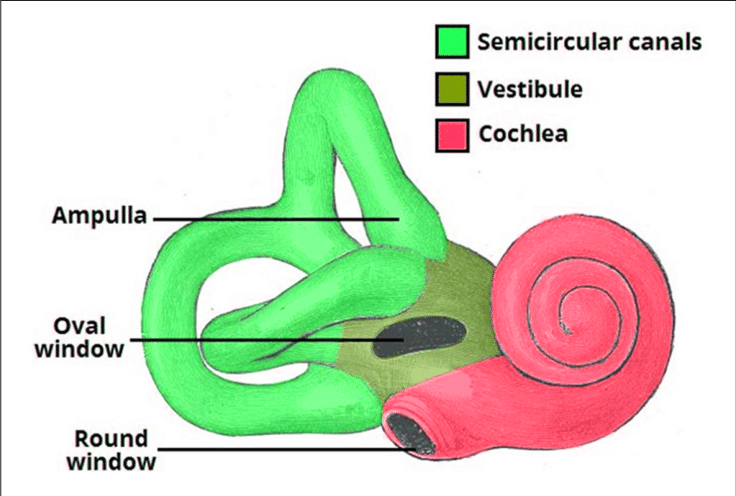
The bony labyrinth has three distinct parts:
- Vestibule (central part)
- Semicircular canals (posterior part)
- Cochlea (anterior part)
Bony labyrinth showing the vestibule, the semicircular canals and the cochlea.
Overview of Inner ear
1. Vestibule. It is a small, oval-shaped central chamber (5 mm) of the bony labyrinth.
Location and Communications:
- It lies between the middle ear laterally and the internal acoustic meatus (IAM) medially.
- Laterally: It is separated from the middle ear cavity by the oval window, which the stapes footplate closes.
- Anteriorly: It communicates with the cochlea.
- Posterosuperiorly: It communicates with the five openings of the semicircular canals.
- Posteriorly: It communicates with the posterior cranial fossa via the vestibular aqueduct, through which the endolymphatic duct passes.
Important Structures within the Vestibule:
- Lateral Wall: The oval window (fenestra vestibuli) is present over the lateral wall, which is closed by the footplate of the stapes.
- Medial Wall: Contains two important recesses that house parts of the membranous labyrinth:
- Spherical Recess: Located antero-inferiorly, it houses the saccule. It features multiple small apertures called the macula cribrosa media, allowing passage of inferior vestibular nerve filaments to the saccule.
- Elliptical Recess: Located postero-superiorly, it houses the utricle. It presents multiple apertures called the macula cribrosa superior (Mike’s dot), for the passage of superior vestibular nerve filaments to the utricle and superior/lateral semicircular ducts.
- The opening of the aqueduct of vestibule (vestibular aqueduct) is also present below the elliptical recess, through which the endolymphatic duct passes.
2. Semicircular canals. There are three semicircular canals.
Orientation and Function: All three semicircular canals lie in planes at right angles to one another. The angle formed by the three semicircular canals is called the solid angle. Each canal has a diameter of 0.8 mm and occupies 2/3rd of a circle.
- Superior (Anterior) Canal – 15-20 mm long, oriented perpendicular to the petrous bone. It detects the rotation of the head in the sagittal plane (e.g., nodding “yes”).
- Lateral (Horizontal) Canal – 12-15 mm long (the shortest SCC), forming a bulge in the medial wall of the aditus ad antrum. It detects the rotation of the head in the transverse plane (vertical axis) (e.g., shaking head “no”). It is set at an angle of about 30 degrees to the horizontal plane. This canal is notably related to the middle ear, making it susceptible to erosion in chronic middle ear disease (e.g., cholesteatoma).
- Posterior (Vertical) Canal – 18-22 mm long (the longest SCC), running parallel to the posterior part of the temporal bone. It detects the rotation of the head in the coronal plane (e.g., tilting the head to the shoulder).
Openings into the Vestibule: Each semicircular canal has two ends opening into the vestibule:
- Ampullated End: One end of each canal is dilated to form an ampulla, which houses the sensory receptor (crista ampullaris) for movement detection. These three ampullated ends open separately into the vestibule.
- Non-ampullated End:
- The non-ampullated ends of the superior and posterior canals typically join to form a common opening called the crus commune (approximately 4 mm in length), which then opens into the medial part of the vestibule.
- The non-ampullated end of the lateral canal opens separately into the vestibule.
- Total Openings: Therefore, the three semicircular canals open into the vestibule by five openings, not six (three ampullated openings + two non-ampullated openings, one of which is the crus commune).
Clinical Correlate: Trautmann’s Triangle. This weak area in the petrous bone is surgically significant. This region is important because infections (e.g., from mastoiditis) can potentially spread through it to the posterior cranial fossa, leading to complications like meningitis or cerebellar abscess. However, it also serves as a surgical access point to the inner ear and posterior fossa. It is bounded by:
- Anteriorly: Bony labyrinth (posterior semicircular canal).
- Posteriorly: Sigmoid sinus.
- Superiorly: Superior petrosal sinus.
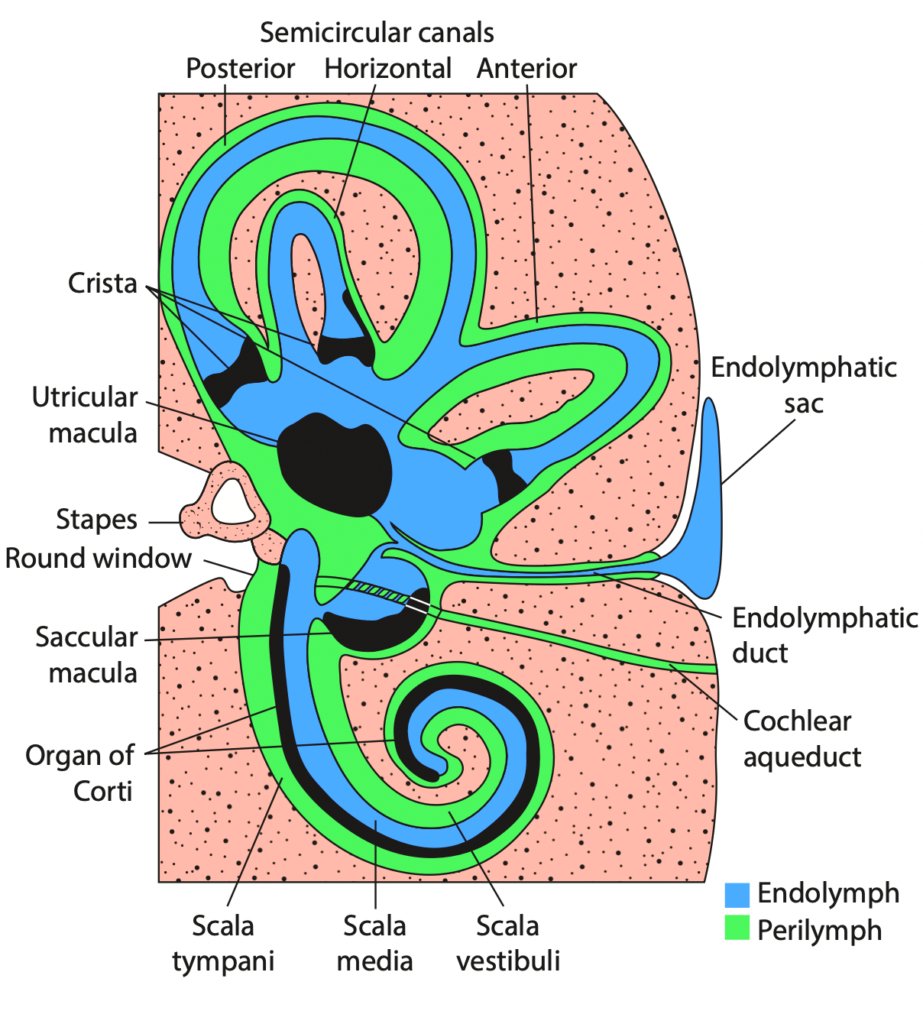
3. Bony Cochlea. It is present anterior to vestibule. It measures 5 mm in height and 9 mm in base diameter, 30 mm in length. The bony cochlea twists on itself to form a coiled tube (like a snail) making 2.5 to 2.75 turns (30 mm length) around a central pyramid of bone called modiolus. The wide base of modiolus is directed towards the internal acoustic meatus and transmits vessels and nerves to the cochlea. A thin plate of bone called osseous spiral lamina, winds spirally like the thread of a screw around the modiolus. The spiral ganglions are present in Rosenthal’s canal, which runs along the osseous spiral lamina. This osseous spiral lamina gives attachment to the basilar membrane and divides the bony cochlear tube into three compartments:
- Scala vestibuli or vestibular duct (upper chamber) – The scala vestibuli is in continuity with the vestibule at the oval window and is closed by the footplate of the stapes.
- Scala tympani or tympanic duct (lower chamber) – The scala vestibuli and scala tympani communicate with each other through an opening called helicotrema at the apex of the cochlear duct. The scala tympani runs parallel to the scala vestibule. The secondary tympanic membrane also known as the round window membrane closes the scala tympani separating it from the middle ear.
- Scala media or cochlear duct (middle chamber) – The cochlear duct (scala media) is separated from the scala vestibule by the Reissner membrane and from the scala tympani by the basilar membrane. It houses the organ of Corti, the primary sensory organ of hearing. It is a part of a membranous labyrinth and not a part of bony labyrinth.
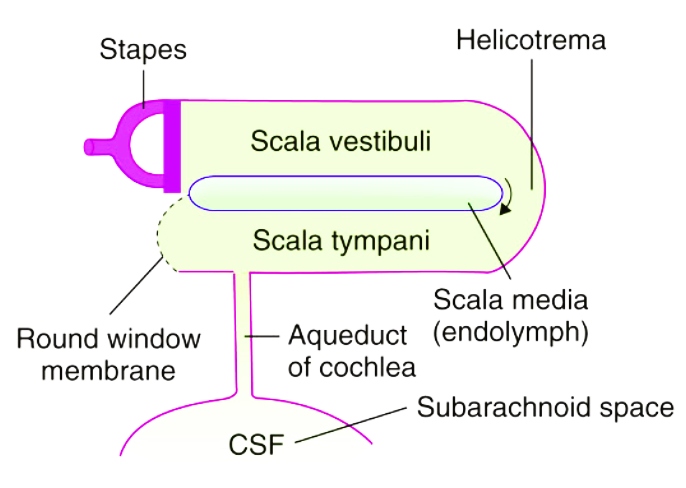
Perilymphatic system. CSF passes into the scala tympani through the aqueduct of the cochlea.
MEMBRANOUS LABYRINTH.
The membranous labyrinth is suspended/ floats inside the bony labyrinth and contains endolymph. The membranous labyrinth consists of:
- Membranous Vestibular Labyrinth: Comprising the utricle and saccule (two sacs).
- Membranous Semicircular Ducts: Three ducts.
- Membranous Cochlea (Cochlear Duct): One duct.
- Endolymphatic Duct and Sac: Connects the vestibular labyrinth to the endolymphatic sac.
The utricle, saccule, and three semicircular ducts are primarily involved in balance (equilibrium), whereas the cochlear duct is exclusively concerned with the sense of hearing.
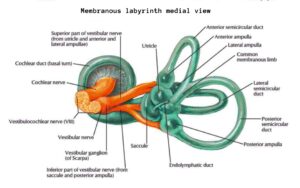
1. Membranous Vestibular Labyrinth (present inside vestibule). It includes:
- Utricle – The utricle is present in the posterior part of the bony vestibule in the elliptical recess. The five openings of the three semicircular ducts open in the utricle. The utricle is connected to the saccule through the utriculosaccular duct, which continues as the endolymphatic duct that passes through the vestibular aqueduct. The terminal part of the endolymphatic duct is dilated to form an endolymphatic sac between the two layers of the dura (intradural) on the posterior surface of the petrous bone in the posterior cranial fossa and it is not communicating with the CSF of the brain. The function of the endolymphatic sac is to absorb endolymph. The endolymphatic sac is exposed for drainage or shunt operation in Meniere’s disease.
- Saccule – The saccule is present in the spherical recess of the bony vestibule, anteroinferiorly to the utricle and opposite the stapes footplate. It detects vertical movements. The utricle is bigger than the saccule and lies superior to the saccule. The saccule is also connected to the cochlear duct (scala media/ membranous cochlea) by a thin duct, ductus reuniens. The cochlear duct empties into the saccule through the ductus reuniens. In Meniere’s disease, the distended saccule lies against the stapes footplate and can be surgically decompressed by perforating the footplate.
- Maculae – The sensory epithelium (sense organ) of both the utricle and saccule is called the macula. It contains hair cells covered by a statoconial membrane, which has calcium carbonate crystals (otoliths) that are related to linear or gravitational acceleration. The utricle responds to linear acceleration in the horizontal plane and sideways head tilts. The saccule responds to linear acceleration in the vertical plane, such as forward-backward and upward-downward movements.
2. Membranous Semicircular ducts. It includes:
- Semicircular ducts – Each membranous semicircular duct runs inside the corresponding bony semicircular canal. They are three in number and open in the utricle. Each semicircular duct is the same in shape as its complementary bony semicircular canal, including a dilated end forming the ampulla. They correspond exactly to the three bony canals.
- Cristae – The sensory epithelium (sense organ) of the three semicircular ducts is the cristae ampullaris. It consists of hair cells embedded in a gelatinous, dome-shaped mass called the cupula, which extends across the ampulla. It is present at the ampullated end of each duct, and it is related to rotational (e.g., head rotation) or angular acceleration.
3. Cochlear duct (membranous cochlea or scala media). It occupies the middle portion of the cochlear canal and it is connected to the saccule by ductus reuniens. It is a blind coiled tube.
It appears triangular on cross-section and its three walls are formed by:
- Floor – It is formed by the Basilar membrane, which supports the organ of Corti and separates the scala media endolymph from the perilymph in the scala tympani. The length of basilar membrane increases as we proceed from the basal coil (base of modiolus) to the apical coil (apex of modiolus). It is for this reason that higher frequencies of sound are heard at the basal coil while lower ones are heard at the apical coil.
- Roof – It is formed by the Reissner’s membrane, which separates it from the scala vestibule.
- Lateral wall – It is formed by the Stria vascularis, which contains vascular epithelium and is concerned with secretion of endolymph.
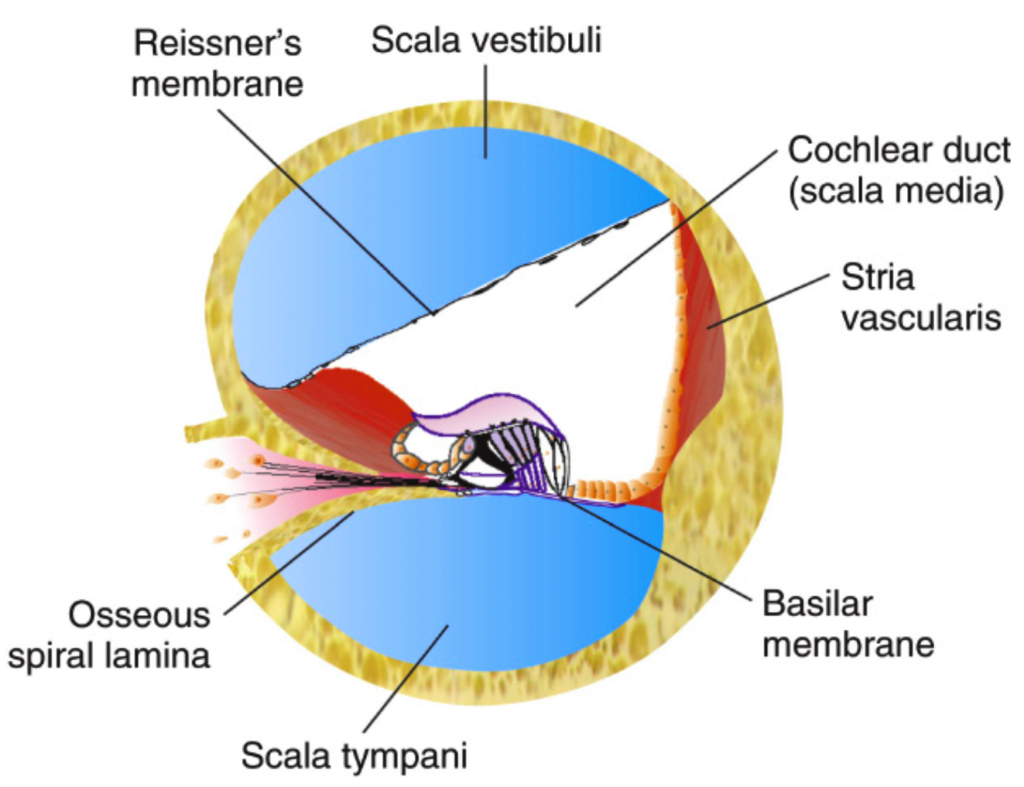
A section through the cochlea to show scala media (cochlear duct), scala vestibuli and scala tympani.
Organ of Corti (the main sensory organ for hearing).
The Organ of Corti is the primary sensory organ of hearing, located on the basilar membrane within the scala media of the cochlea. It is responsible for converting sound vibrations into electrical signals, which are then transmitted to the brain.
Key Components of the Organ of Corti
- Tunnel of Corti. It is formed by two rows of pillar (rod) cells, which separate the inner hair cells and outer hair cells. It creates a triangular structure with the basement membrane and contains cortilymph, though its exact function remains unclear.
- Inner Hair Cells (IHCs): They are arranged in a single row. They are richly supplied by afferent cochlear nerve fibres, making them crucial for transmitting auditory signals.
- Outer Hair Cells (OHCs): They are arranged in three to four rows. The tips of the outer hair cells are attached to the undersurface of the tectorial membrane. They receive efferent innervation from the olivary complex, playing a role in modulating Inner hair cells function.
- Both the IHC and OHC are supported by pillar cells, Deiters’ cells, and Hensen’s cells, which provide structural stability.
- Hair Cells – The Sensory Receptors. They are important receptor cells of hearing and transduce sound energy into electrical energy.
- Tectorial Membrane. It consists of a gelatinous material with delicate fibres that overlies the Organ of Corti. When sound waves cause vibrations of the basilar membrane, the shearing force between the hair cells and the tectorial membrane produces a stimulus to the hair cells.
- Stria Vascularis. It is located on the lateral wall of the scala media (cochlear duct), which contains vascular epithelium and is concerned with secretion of endolymph. It plays a crucial role in maintaining the ionic composition and electric potential of the endolymph, which is essential for proper hair cell function.

Clinical Significance:
- Cochlear Implants. The cochlear implant electrodes are inserted through the round window (i.e. secondary tympanic membrane) to reach the internal ear. The electrodes are placed in the scala tympani to bypass the damaged organ of Corti and directly stimulate the auditory nerve.
- Drugs. Drugs like gentamicin or steroids also pass through the round window to reach the internal ear from the middle ear.
- Infections. Infections from the brain can easily enter the internal ear through the internal acoustic meatus and the cochlear aqueduct leading to labyrinthitis. Conversely, infections from the internal ear can spread to the brain. Therefore, hearing tests, such as BERA, are recommended, particularly in pediatric patients with meningitis, to rule out hearing loss.
INNER EAR FLUIDS AND THEIR CIRCULATION. There are two fluids in the inner ear: perilymph and endolymph. Perilymph fills the space between bony and membranous labyrinth while endolymph fills the entire membranous labyrinth.
1. Perilymph. It resembles extracellular fluid and is rich in Na ions. It communicates with CSF through the aqueduct of cochlea which opens into the scala tympani near the round window. In fact this duct is not a direct communication but contains connective tissue resembling arachnoid through which perilymph percolates. There are two views regarding the formation of perilymph: (i) It is a filtrate of blood serum and is formed by capillaries of the spiral ligament and (ii) it is a direct continuation of CSF and reaches the labyrinth via the aqueduct of cochlea.
| TABLE 1.2 COMPOSITION OF INNER EAR FLUIDS | Endolymph | Perilymph | CSF |
| Na+ (mEq/L) | 5 | 140 | 152 |
| K+ (mEq/L) | 144 | 10 | 4 |
| Protein (mg/dL) | 126 | 200–400 | 20–50 |
| Glucose (mg/dL) | 10–40 | 85 | 70 |
2. Endolymph. It fills the entire membranous labyrinth and resembles intracellular fluid, being rich in K ions. It is secreted by the secretory cells of the stria vascularis of the cochlea and by the dark cells (present in the utricle and also near the ampullated ends of semicircular ducts). There are two views regarding its flow: (i) longitudinal, i.e. endolymph from the cochlea reaches saccule, utricle and endolymphatic duct and gets absorbed through the endolymphatic sac, which lies in the subdural space and (ii) radial, i.e. endolymph is secreted by stria vascularis and also gets absorbed by the stria vascularis. This view presumes that the endolymphatic sac is a vestigial structure in man and plays no part in endolymph absorption.
BLOOD SUPPLY OF LABYRINTH
The entire labyrinth receives its arterial supply through labyrinthine artery, which is a branch of anterior-inferior cerebellar artery but sometimes from the basilar.
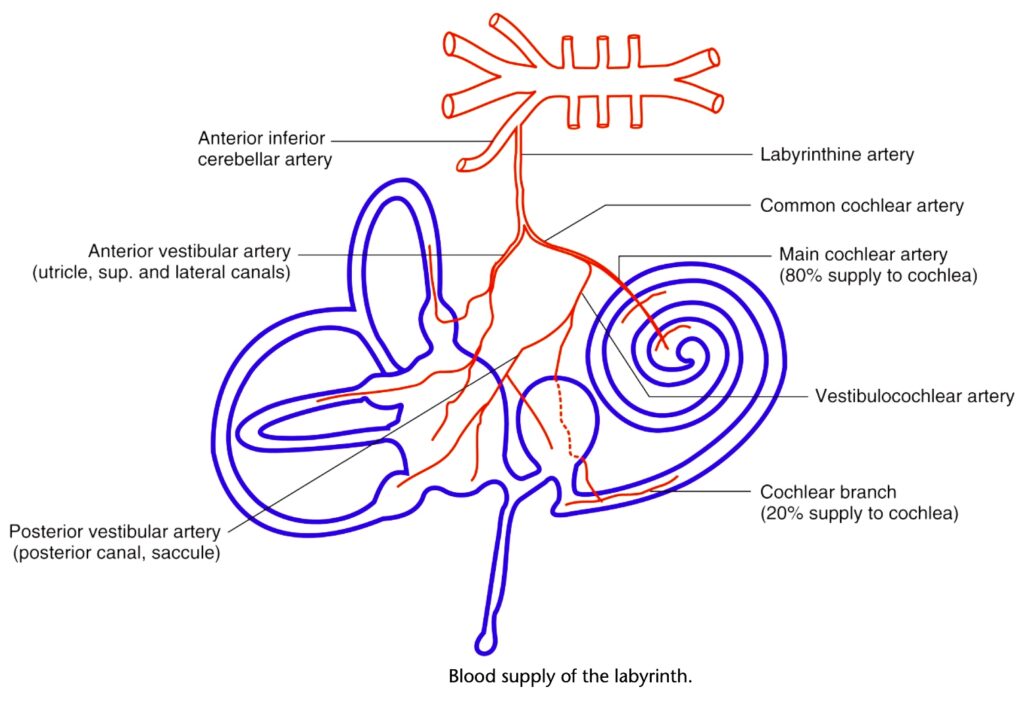
Divisions of the labyrinthine artery which supply blood to various parts of the labyrinth.
Venous drainage is through three veins, namely internal auditory vein, vein of cochlear aqueduct and vein of vestibular aqueduct, which ultimately drain into inferior petrosal sinus and lateral venous sinus.
It is to be noted that:
- Blood supply to the inner ear is independent of blood supply to middle ear and bony otic capsule, and there is no cross circulation between the two.
- Blood supply to cochlea and vestibular labyrinth is segmental, therefore, independent ischaemic damage can occur to these organs causing either cochlear or vestibular symptoms.
———— End of the chapter ————
Clinical Significance & Practical Applications
Understanding inner ear anatomy is crucial for diagnosing and managing various ENT conditions.
- Cochlear Implants: These revolutionary devices restore hearing in individuals with severe-to-profound SNHL. The electrodes of a cochlear implant are typically inserted through the round window (secondary tympanic membrane) into the scala tympani. They bypass the damaged Organ of Corti and directly stimulate the auditory nerve fibers.
- Intratympanic Drug Delivery: Medications, such as gentamicin (for Meniere’s disease) or steroids (for sudden SNHL), can be directly applied to the middle ear. These drugs then diffuse across the round window membrane (and possibly the oval window) to reach the internal ear fluids, offering targeted local therapy.
- Infections (Labyrinthitis): Infections from the brain (e.g., meningitis) can easily enter the internal ear through the internal acoustic meatus (along nerve sheaths) and the cochlear aqueduct (fluid communication), leading to labyrinthitis (inflammation of the inner ear). Conversely, infections from the internal ear (e.g., secondary to otitis media extending to the labyrinth) can spread to the brain, causing intracranial complications. Therefore, hearing tests, such as Brainstem Evoked Response Audiometry (BERA), are highly recommended, particularly in pediatric patients with meningitis, to detect and manage potential hearing loss.
- Meniere’s Disease: This condition is strongly linked to endolymphatic hydrops (excess endolymph) due to imbalance in endolymph production or absorption, impacting the endolymphatic sac.
- Sudden Sensorineural Hearing Loss (SSNHL): Often idiopathic, but vascular compromise of the labyrinthine artery (due to its end-artery nature and segmental supply) is a leading hypothesis.
- Benign Paroxysmal Positional Vertigo (BPPV): Caused by dislodged otoconia (calcium carbonate crystals from the maculae of the utricle/saccule) that migrate into the semicircular canals, disrupting endolymph movement.
High-Yield Points for NEET PG and University Exams
- Labyrinth Location: Petrous part of temporal bone.
- Windows: Oval window (stapes, to scala vestibuli), Round window (secondary TM, to scala tympani).
- IAM Contents: CN VII (Facial), CN VIII (Vestibulocochlear), Labyrinthine Artery.
- Bony Labyrinth Parts: Vestibule, 3 Semicircular Canals, Cochlea.
- Membranous Labyrinth Parts: Utricle, Saccule, 3 Semicircular Ducts, Cochlear Duct, Endolymphatic Duct & Sac.
- Vestibule Recesses: Spherical (saccule, macula cribrosa media) and Elliptical (utricle, macula cribrosa superior/Mike’s dot).
- Semicircular Canals: Detect angular acceleration. Superior (sagittal), Lateral (transverse, 30 deg to horizontal), Posterior (coronal). All open by 5 not 6 openings (crus commune).
- Cochlea:5-2.75 turns around modiolus. Houses spiral ganglion in Rosenthal’s canal.
- Cochlear Compartments: Scala Vestibuli (perilymph), Scala Media (endolymph, Organ of Corti), Scala Tympani (perilymph).
- Helicotrema: Communication between scala vestibuli and scala tympani at cochlear apex.
- Reissner’s Membrane: Separates scala vestibuli from scala media.
- Basilar Membrane: Separates scala media from scala tympani; supports Organ of Corti; tonotopy (high freq at base, low freq at apex).
- Stria Vascularis: Secretes endolymph (high K+); maintains endocochlear potential.
- Organ of Corti: Sensory organ of hearing on basilar membrane.
- IHCs: Single row, primary afferent input (90-95%).
- OHCs: 3-4 rows, efferent innervation, electromotility (amplifies basilar membrane movement, sharpens frequency tuning).
- Tectorial Membrane: Overlies hair cells, involved in shearing force.
- Endolymph: High K+, Low Na+; secreted by Stria Vascularis & dark cells; absorbed by Endolymphatic Sac.
- Perilymph: High Na+, Low K+; similar to CSF; communicates with CSF via Cochlear Aqueduct.
- Labyrinthine Artery: Branch of AICA (or basilar); end-artery system; segmental supply explains isolated auditory/vestibular loss.
- Clinical Applications: Cochlear implants (scala tympani via round window), Intratympanic injections (via round window), Labyrinthitis spread (via IAM, cochlear aqueduct), Meniere’s (endolymphatic hydrops).
Multiple Choice Questions (MCQs)
Instructions: Choose the single best answer for each question.
- Which of the following structures is part of the membranous labyrinth and is primarily responsible for detecting linear acceleration in the horizontal plane? a) Cochlear duct b) Saccule c) Utricle d) Semicircular canal e) Endolymphatic sac
- The Organ of Corti is located on which of the following membranes within the cochlea? a) Reissner’s membrane b) Tectorial membrane c) Basilar membrane d) Secondary tympanic membrane e) Stapedial membrane
- Which fluid fills the scala vestibuli and scala tympani of the cochlea? a) Endolymph b) Cortilymph c) Perilymph d) Cerebrospinal fluid e) Intracellular fluid
- The primary function of the outer hair cells in the Organ of Corti is: a) Direct transmission of auditory signals to the brain. b) Secretion of endolymph. c) Amplification of basilar membrane motion and frequency tuning. d) Detection of rotational head movements. e) Absorption of perilymph.
- The labyrinthine artery typically branches off from which major artery? a) Middle meningeal artery b) Posterior inferior cerebellar artery (PICA) c) Anterior inferior cerebellar artery (AICA) d) Internal carotid artery e) Vertebral artery
- In Meniere’s disease, the pathological hallmark is an excess of which inner ear fluid? a) Perilymph b) Cortilymph c) Cerebrospinal fluid d) Endolymph e) Plasma
- Which of the following structures connects the scala vestibuli and scala tympani at the apex of the cochlea? a) Round window b) Oval window c) Helicotrema d) Cochlear aqueduct e) Ductus reuniens
- The macula cribrosa superior (Mike’s dot) is a feature of the medial wall of the bony vestibule and transmits nerve filaments to which structure? a) Saccule b) Cochlear duct c) Inferior vestibular nerve d) Utricle and superior/lateral semicircular ducts e) Endolymphatic sac
- A cochlear implant electrode is typically inserted into which specific part of the cochlea? a) Scala vestibuli b) Scala media c) Scala tympani d) Modiolus e) Organ of Corti
- The crus commune is formed by the fusion of the non-ampullated ends of which two semicircular canals? a) Superior and lateral b) Lateral and posterior c) Superior and posterior d) All three semicircular canals e) It opens separately
MCQ Answers and Explanations:
- c) Utricle
- Explanation: The utricle is an otolithic organ within the membranous vestibular labyrinth. Its macula detects linear acceleration in the horizontal plane and static head tilt. The saccule detects vertical linear acceleration.
- c) Basilar membrane
- Explanation: The Organ of Corti, the sensory receptor for hearing, sits directly on the basilar membrane within the scala media (cochlear duct).
- c) Perilymph
- Explanation: The scala vestibuli and scala tympani, parts of the bony labyrinth, are filled with perilymph, which resembles extracellular fluid and CSF. The scala media (cochlear duct) is filled with endolymph.
- c) Amplification of basilar membrane motion and frequency tuning.
- Explanation: Outer hair cells exhibit electromotility, actively contracting and expanding to amplify the vibrations of the basilar membrane. This enhances the sensitivity and frequency selectivity of the cochlea, which is crucial for hearing soft sounds and fine frequency discrimination. Inner hair cells are the primary transducers.
- c) Anterior inferior cerebellar artery (AICA)
- Explanation: The labyrinthine artery (internal auditory artery) is usually a branch of the AICA. Less commonly, it can arise directly from the basilar artery.
- d) Endolymph
- Explanation: Meniere’s disease is pathologically characterized by endolymphatic hydrops, an excess accumulation of endolymph within the membranous labyrinth.
- c) Helicotrema
- Explanation: The helicotrema is the only point of communication between the scala vestibuli and scala tympani, located at the apex of the cochlea.
- d) Utricle and superior/lateral semicircular ducts
- Explanation: The macula cribrosa superior transmits nerve filaments from the superior vestibular nerve to the utricle and the ampullae of the superior and lateral semicircular ducts. The macula cribrosa media transmits fibers to the saccule.
- c) Scala tympani
- Explanation: Cochlear implant electrodes are specifically designed to be inserted into the scala tympani, typically via the round window, to directly stimulate the auditory nerve fibers while minimizing trauma to remaining cochlear structures.
- c) Superior and posterior
- Explanation: The non-ampullated ends of the superior (anterior) and posterior semicircular canals join to form the crus commune before opening into the vestibule.
Clinical-Based Questions
Instructions: Analyse the following scenarios and answer the questions, applying your knowledge of internal ear anatomy.
- Scenario: A 55-year-old patient presents with new-onset hearing loss and severe vertigo. MRI reveals an ischemic event affecting the labyrinthine artery.
- a) Explain why an ischemic event to the labyrinthine artery can cause both hearing loss and vertigo.
- Answer: The labyrinthine artery is the sole arterial supply to the entire inner ear, supplying both the cochlea (responsible for hearing) and the vestibular system (responsible for balance). Since it’s an end-artery system with segmental supply, an ischemic event can simultaneously impair blood flow to both the auditory and vestibular portions, leading to a combination of hearing loss (cochlear dysfunction) and vertigo (vestibular dysfunction).
- b) What is the most common anatomical origin of the labyrinthine artery?
- Answer: The labyrinthine artery most commonly originates as a branch of the anterior inferior cerebellar artery (AICA).
- c) If the patient experienced only hearing loss but no vertigo, what might that suggest about the specific vascular insult within the inner ear?
- Answer: This might suggest a more localised ischemic event affecting primarily the common cochlear artery or its branches, preserving the blood supply to the vestibular labyrinth. This demonstrates the segmental nature of inner ear blood supply.
- a) Explain why an ischemic event to the labyrinthine artery can cause both hearing loss and vertigo.
- Scenario: A 4-year-old child who recently recovered from bacterial meningitis is undergoing a hearing assessment. The audiologist recommends a Brainstem Evoked Response Audiometry (BERA) test.
- a) Why is hearing assessment crucial for a child post-meningitis, considering the anatomy of the inner ear?
- Answer: Meningitis, an infection of the meninges surrounding the brain, can cause hearing loss due to the spread of infection to the inner ear. The cerebrospinal fluid (CSF) communicates with the perilymphatic space of the inner ear via the cochlear aqueduct and along the nerve sheaths in the internal acoustic meatus. This anatomical connection allows bacteria or inflammatory mediators from the meninges to reach the cochlea, causing labyrinthitis and potentially irreversible sensorineural hearing loss.
- b) Which specific inner ear fluid would primarily be affected by the spread of infection from CSF?
- Answer: The perilymph, which fills the scala vestibuli and scala tympani, would primarily be affected, as it communicates with the CSF.
- c) If hearing loss is confirmed, what are the long-term management considerations for this child?
- Answer: Long-term management would primarily involve hearing aids for mild-to-moderate loss. For severe-to-profound bilateral hearing loss, a cochlear implant would be the gold standard, often requiring prompt implantation to maximize speech and language development in children with post-meningitic deafness due to potential cochlear ossification.
- a) Why is hearing assessment crucial for a child post-meningitis, considering the anatomy of the inner ear?
- Scenario: A patient with long-standing, severe Meniere’s disease is being considered for an endolymphatic sac decompression surgery to alleviate debilitating vertigo.
- a) What is the underlying pathology in Meniere’s disease that makes the endolymphatic sac a surgical target?
- Answer: The underlying pathology is endolymphatic hydrops, an overaccumulation or malabsorption of endolymph within the membranous labyrinth. The endolymphatic sac is thought to be the primary site of endolymph absorption. Decompressing it aims to restore endolymphatic fluid homeostasis and reduce pressure.
- b) Describe the location of the endolymphatic sac relative to the temporal bone and cranial fossae.
- Answer: The endolymphatic sac is located on the posterior surface of the petrous part of the temporal bone, between the two layers of the dura mater (intradural), within the posterior cranial fossa. It is reached via the vestibular aqueduct from the utricle.
- c) Which specific inner ear fluid would be drained during an endolymphatic sac decompression, and what is its unique ionic composition?
- Answer: Endolymph would be drained. Its unique ionic composition is high in K+ ions and low in Na+ ions, resembling intracellular fluid. This is crucial for hair cell function.
- a) What is the underlying pathology in Meniere’s disease that makes the endolymphatic sac a surgical target?
Frequently Asked Questions in Viva
- Q: What are the two main parts of the internal ear?
- A: The two main parts are the rigid, protective bony labyrinth (filled with perilymph) and the delicate, sensory-containing membranous labyrinth (filled with endolymph).
- Q: What is the primary function of the cochlea?
- A: The cochlea is the primary organ for hearing, responsible for converting sound vibrations into electrical signals that the brain can interpret.
- Q: Which structures detect linear acceleration versus rotational acceleration?
- A: The utricle and saccule (otolithic organs) detect linear acceleration and head tilt, while the semicircular canals detect rotational (angular) acceleration.
- Q: What is the Organ of Corti and where is it located?
- A: The Organ of Corti is the main sensory organ for hearing, located on the basilar membrane within the scala media (cochlear duct) of the cochlea.
- Q: What is the crucial role of the stria vascularis?
- A: The stria vascularis, located on the lateral wall of the scala media, is responsible for the secretion of endolymph and maintaining its unique ionic composition and electrical potential, vital for hair cell function.
- Q: How do inner ear fluids differ from each other?
- A: Perilymph is high in Na+ (like CSF/extracellular fluid) and fills the bony labyrinth space, while endolymph is high in K+ (like intracellular fluid) and fills the membranous labyrinth.
- Q: Why is the labyrinthine artery clinically important?
- A: The labyrinthine artery is the sole blood supply to the entire inner ear and is an end-artery, making the inner ear highly vulnerable to ischemic damage, which can cause sudden hearing loss or vertigo.
Practical Tips for Viva and Clinical Exam Scenarios
- Presenting Internal Ear Anatomy in Viva:
- Start with the Big Picture: “The internal ear, or labyrinth, is located in the petrous temporal bone, responsible for hearing and balance. It comprises a bony and a membranous labyrinth.”
- Layer by Layer: Describe the bony labyrinth first (vestibule, SCCs, cochlea), then the membranous labyrinth (utricle, saccule, SCC ducts, cochlear duct, endolymphatic sac). For each, mention their contents, key features, and function.
- Focus on Relationships: Emphasize how bony and membranous parts relate (e.g., membranous within bony, perilymph vs. endolymph).
- Key Landmarks: Be precise with locations like oval/round windows, IAM, modiolus, helicotrema, crus commune.
- Sensory Receptors: Clearly state what the maculae detect (linear) and what the cristae detect (angular), and where the Organ of Corti is located.
- Fluid Dynamics: Explain perilymph and endolymph composition and circulation, especially the role of stria vascularis and endolymphatic sac.
- Blood Supply: Highlight the labyrinthine artery’s origin and its significance as an end-artery.
- Common Examiner Questions (Viva):
- “Differentiate between perilymph and endolymph.”
- “Describe the detailed anatomy of the Organ of Corti.” (Be ready for IHCs vs OHCs, tectorial membrane, basilar membrane).
- “How does sound transduction occur at the hair cell level?”
- “What is the significance of the endolymphatic sac?”
- “What are the anatomical connections of the inner ear to the middle ear and the brain?”
- “Explain the function of each of the semicircular canals.”
- “Which structures pass through the internal acoustic meatus?”
- “Why is the blood supply of the inner ear important clinically?”
- “Where do you insert cochlear implant electrodes?”
- Clinical Exam Scenarios (Applying Anatomy):
- Patient with vertigo post-head injury: “Could this be BPPV? Explain the anatomical basis.” (Dislodged otoconia from utricle/saccule migrating into SCCs).
- Patient with sudden onset unilateral hearing loss: “What is the likely vessel involved, and why is the inner ear so vulnerable?” (Labyrinthine artery, end-artery, segmental supply).
- Child with meningitis and hearing loss: “Trace the anatomical pathway of infection from meninges to the cochlea.” (Cochlear aqueduct, IAM).
Download full PDF Link:
Anatomy of Internal Ear Best Lecture Notes Dr Rahul Bagla ENT Textbook
Download PPT:
Anatomy of Ear Best PPT Notes Lectures Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Helicotrema, Endolymphatic sac, Endolymph, Perilymph, Ductus Reunions, Macula, Saccule, Cristae, Cochlear aqueduct, Anatomy of Internal ear, Internal ear anatomy, Structure of the inner ear, Parts of the internal ear, Function of the inner ear, Cochlea and vestibular system, Detailed anatomy of the internal ear, How does the inner ear work? Bony labyrinth and membranous labyrinth explained, Role of the cochlea in the hearing process, Vestibular system and balance control, What are the parts of the inner ear? How does the cochlea help in hearing? What is the function of semicircular canals? How does the vestibular system maintain balance? What is the difference between the bony and membranous labyrinth? Anatomy of the Internal Ear: Structure, Function, and Clinical Significance, How the Inner Ear Works: Understanding Cochlea & Vestibular System, Complete Guide to Inner Ear Anatomy – Bony & Membranous Labyrinth Explained, Hearing and balance system, Auditory pathway of the inner ear, Sensory organs of the ear, Inner ear fluid dynamics, Ear equilibrium function/p>

inter
Very todo,and,graphical presentación,Dr.khumal
i want alwes study y… noot
Dr Rahul, your content is better than most paid books. The diagrams and flow are excellent.
Ahmed El-Tayeb, Surgical Intern, Cairo University, Egypt
Regards
“Thank you, Ahmed! Your feedback motivates me to keep refining the content