|
The following CBME core competencies are covered in this chapter.
|
Physiology of Hearing: From Sound Waves to Neural Perception
Hearing involves the neural perception of sound energy, which includes the identification (what?) and localisation (from where?) of sounds. The ear is composed of the external ear, middle ear, and cochlea in the inner ear, all of which are crucial for hearing. The inner ear’s semicircular canals, utricle, and saccule are responsible for maintaining equilibrium or balance.
What is Sound?
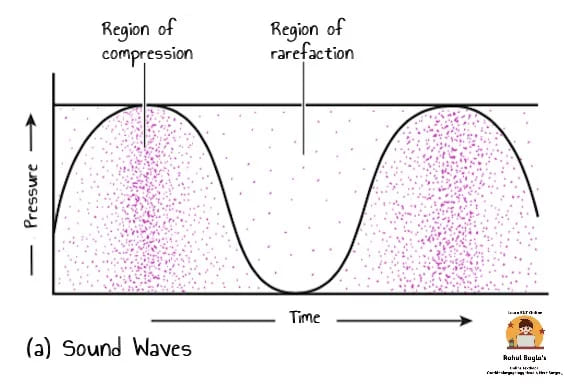
Sound waves are produced by the compression and decompression of air molecules by a vibrating object.
Formation and Structure of Sound Waves:
- Structure of Sound Waves: Sound waves are composed of alternating areas of compressed and spread-out air molecules.
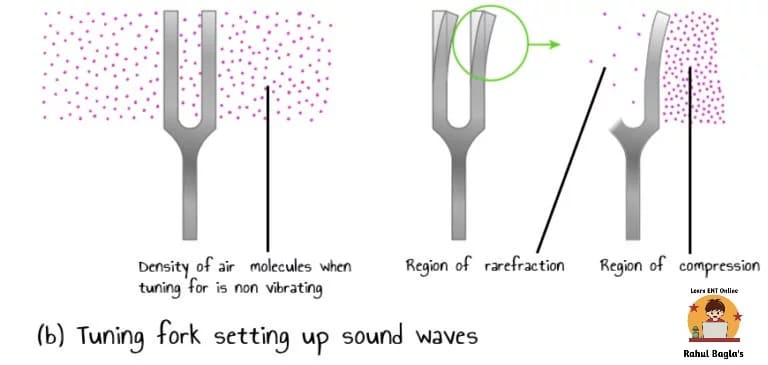
- Tuning Fork Example: A vibrating tuning fork compresses air molecules in front of it and spreads out molecules behind it, creating sound waves.
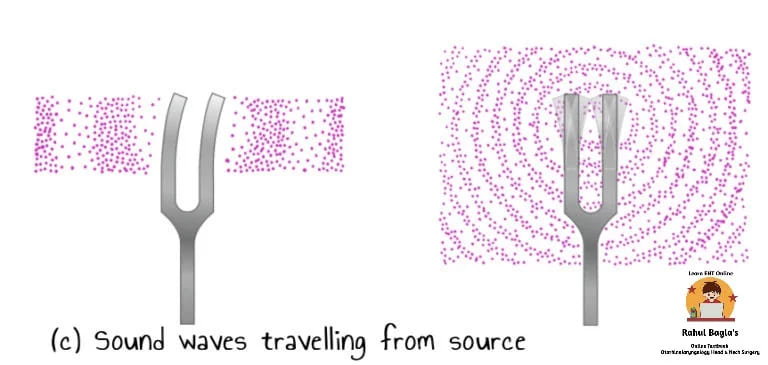
- Propagation of Sound Waves: Disturbed air molecules collide with further molecules, causing new areas of disturbance and allowing sound waves to travel progressively further from the source. Sound waves eventually fade when they become too weak to affect the surrounding region.
Speed of Sound
- In Air: Sound travels at 344 meters (1120 feet) per second in air at 20°C and at sea level.
- In Liquids and Solids: Sound moves faster in liquids and solids than in the air.
- Transition from Air to Liquid: Sound waves don’t travel efficiently from air to a liquid medium due to reflection caused by the high inertia of the liquid.


Mechanism of Hearing: A Three-Fold Process
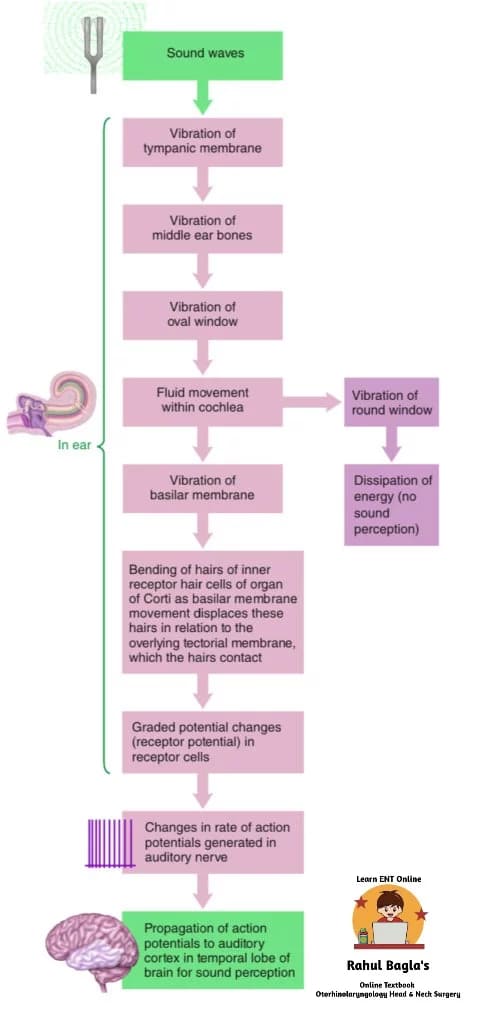
The complex mechanism of hearing can be broadly divided into three principal stages:
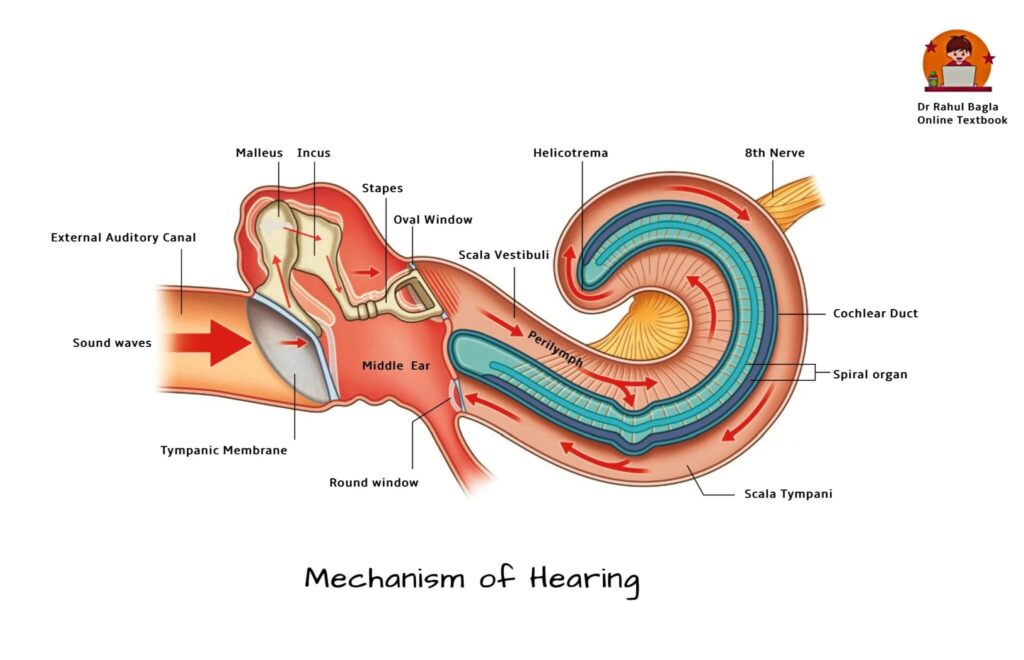
- Mechanical Conduction of Sound (Conduction Apparatus): This initial stage involves the collection and transmission of sound waves through the external and middle ear.
- Transduction of Mechanical Energy to Electrical Impulses (Sensory System of Cochlea): Here, the mechanical vibrations are converted into electrical signals by specialized hair cells within the cochlea.
- Conduction of Electrical Impulses to the Brain (Neural Pathways): Finally, these electrical impulses travel along specific neural pathways to the auditory centers in the brain for interpretation.
1. Mechanical Conduction of Sound (Conduction Apparatus)
This phase ensures that sound energy efficiently reaches the inner ear despite changes in the transmitting medium.
A. Role of the External Ear in Mechanical Conduction
The external ear, comprising the pinna and the external auditory meatus, plays a vital role in capturing and directing sound.
- Pinna (Auricle): This visible, cartilaginous part of the ear plays a crucial role in localising sound, particularly in the vertical plane. It effectively captures sound waves and funnels them into the external auditory meatus. Therefore, its unique shape contributes to our ability to discern the direction of a sound source.
- External Auditory Meatus (Ear Canal): This canal efficiently conducts sound waves to the tympanic membrane. Moreover, it acts as a resonating tube, amplifying sound frequencies between 2000 Hz and 5000 Hz, which are particularly important for speech perception.
- Tympanic Membrane (Eardrum): This essential component functions as a sensitive pressure receiver, converting airborne sound waves into mechanical vibrations. It also acts as a resonator and critically dampens vibrations, thus ensuring efficient sound processing and preventing excessive movement that could distort the signal.
B. Role of the Middle Ear in Mechanical Conduction
The middle ear, a small air-filled cavity, performs four critical functions that significantly enhance hearing. These mechanisms overcome the impedance mismatch between air and the inner ear fluids.
- Impedance Matching Mechanism (Transformer Action):
-
- The Challenge: The acoustic impedance (resistance to sound propagation) of the inner ear fluids (perilymph and endolymph) is significantly higher than that of air in the middle ear. Consequently, if sound directly struck the oval window from the air, approximately 99.9% of the sound energy would reflect away from the liquid’s surface, resulting in a profound hearing loss of about 30 dB.
- The Solution: To overcome this substantial energy loss, the tympanic membrane and the ear ossicles (malleus, incus, stapes) collaborate. They effectively convert sound from a low-force, high-amplitude vibration in the air to a high-force, low-amplitude vibration suitable for the fluid-filled inner ear. This crucial function is known as the “impedance matching mechanism” or “transformer action.”
- How it is Accomplished: This mechanism is primarily achieved through three synergistic actions:
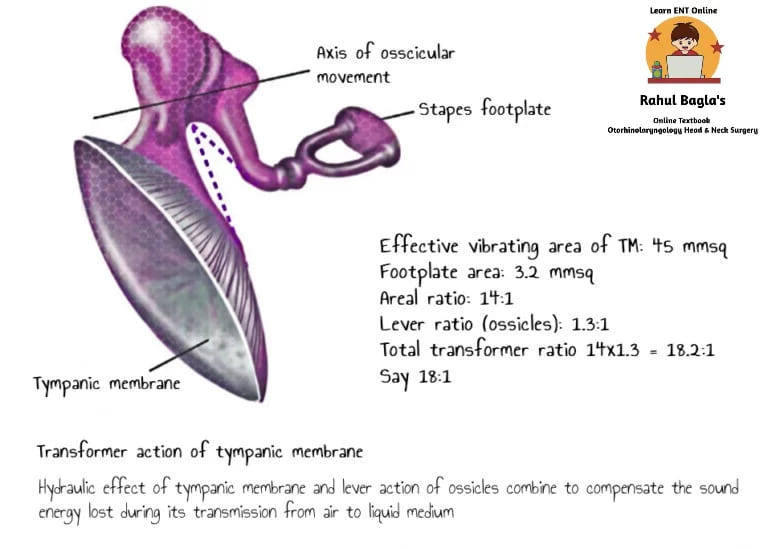
- Lever Action of Ossicles: The handle of the malleus is approximately 1.3 times longer than the long process of the incus. This anatomical difference provides a mechanical advantage, increasing the force exerted on the stapes by 1.3 times.
- Hydraulic Action of the Tympanic Membrane (Areal Ratio): The surface area of the tympanic membrane is much larger than the surface area of the stapes footplate. While the anatomical ratio is roughly 21:1 (tympanic membrane: 90 mm², stapes footplate: 3.2 mm²), the effective vibratory area of the tympanic membrane is only about two-thirds of the total surface area (approximately 55 mm²). Therefore, the effective areal ratio becomes approximately 17:1 (55 mm² / 3.2 mm²). This significant size difference concentrates the force produced by sound over a much smaller area, thereby amplifying the pressure exerted on the oval window by approximately 17 times.
- Combined Amplification: The total transformer ratio, which represents the combined amplification from the lever action and the hydraulic action, is approximately 18:1 (1.3 × 14 ≈ 18) using the classic calculation, or up to 22.1:1 (1.3 × 17 ≈ 22.1) using the more refined Wever and Lawrence calculation. This substantial amplification (about 25-30 dB) is vital for efficient sound transmission to the inner ear.
- Curved Tympanic Membrane Effect: The conical shape and elasticity of the tympanic membrane also contribute a small amount of leverage. Movements are more pronounced at the periphery than at the center where the malleus handle attaches, further enhancing force transmission.
- Attenuation Reflex (Acoustic Reflex):
-
- Nature: This is a vital protective reflex that safeguards the inner ear from damage caused by excessively loud sounds.
- Mechanism: When exposed to loud sounds (typically 70-80 dB above the hearing threshold), two tiny muscles within the middle ear contract reflexively. The tensor tympani muscle pulls the malleus inwards, tightening the tympanic membrane. Simultaneously, the stapedius muscle pulls the stapes outwards, restricting its movement at the oval window. This combined action makes the ossicular chain more rigid and significantly reduces the transmission of intense sound energy to the inner ear. Interestingly, this reflex also plays a minor role in opening the Eustachian tube.
- Advantages:
- It prevents cochlear damage from prolonged exposure to loud music or occupational noise (e.g., jet aircraft).
- It selectively masks low-frequency environmental sounds, allowing us to concentrate on higher-frequency sounds (above 1000 Hz), which are crucial for speech understanding.
- It reduces the intensity of sounds generated intrinsically, such as during vocalization or chewing, preventing these internal noises from overwhelming our hearing.
- Important Note: The attenuation reflex is a slow protective reflex with a latent period of approximately 40 milliseconds. This delay means it offers limited protection against sudden, extremely loud sounds like a gunshot or bomb explosion, which can still cause acute cochlear damage. Therefore, it primarily protects against prolonged intense sounds. A historical example of applying this principle was the design of anti-aircraft guns during World War II, which produced a loud pre-firing sound to trigger the reflex and protect the gunner’s ears from the subsequent, much louder actual firing sound.
- Phase Differential Between Cochlear Windows:
-
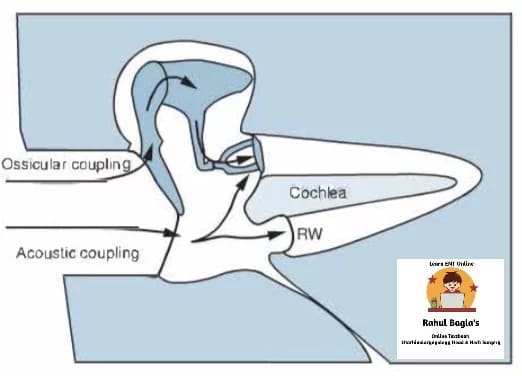
- The Principle: The fluids within the inner ear (perilymph and endolymph) are largely incompressible. For fluid movement and subsequent hearing to occur, there must be a pressure differential across the cochlea. This is achieved because the round window vibrates in the opposite phase to the oval window.
- Mechanism: When the stapes footplate pushes inwards on the oval window, creating a wave of compression in the perilymph of the scala vestibuli, the round window simultaneously bulges outwards, accommodating the fluid displacement. Conversely, when the stapes pulls outwards, the round window moves inwards. If sound waves were to strike both the oval and round windows simultaneously and in the same phase, they would cancel each other out, resulting in no perilymph movement and, consequently, no hearing.
- Contribution to Hearing: This critical phase differential between the windows contributes approximately 4 dB to sound transmission when the tympano-ossicular system is intact. This acoustic separation is attributed to two effects:
- Ossicular Coupling Effect: An intact tympano-ossicular system creates a preferential pathway for sound transmission to the oval window.
- Acoustic Coupling Effect: A cushion of air within the middle ear space surrounding the round window also helps maintain the phase difference.
- Natural Resonance of External and Middle Ear:
-
- Concept: The external and middle ear, owing to their inherent anatomical and physiological properties, preferentially transmit certain frequencies of sound to the inner ear. This phenomenon is known as natural resonance.
- Resonant Frequencies:
- External Auditory Canal: Resonates optimally around 3000 Hz.
- Tympanic Membrane: Resonates efficiently between 800–1600 Hz.
- Middle Ear Cavity: Has a natural resonance of approximately 800 Hz.
- Ossicular Chain: Resonates optimally between 500–2000 Hz.
- Overall Impact: Due to these combined resonant characteristics, the human auditory system exhibits its greatest sensitivity and efficient sound transmission between 500 and 3000 Hz. This frequency range is crucial as it encompasses most speech and daily conversation sounds.
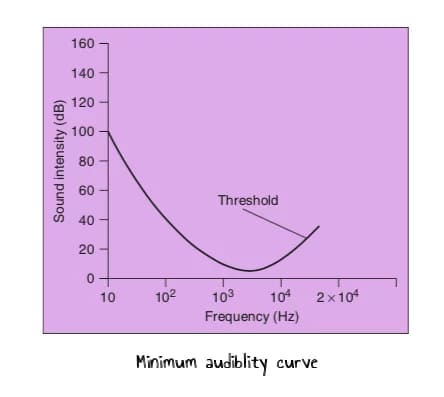
Minimum Audibility Curve (Audiogram): The minimum audibility curve, or audiogram, graphically depicts the lowest sound intensity (in dB HL, Hearing Level) that a person can hear at various frequencies. It illustrates that:
- The amplification of sound intensity is highest between 1000 and 3000 Hz, reflecting the combined resonance of the ear’s conductive components.
- Sounds below 16 Hz (infrasound) or above 20,000 Hz (ultrasound) are typically not amplified or perceived by the human ear. This is why the human ear can generally perceive the pitch of sound only between 16 Hz and 20,000 Hz, with maximum sensitivity occurring between 1000 and 3000 Hz.
2. Transduction of Mechanical Energy to Electrical Impulses (Sensory System of the Cochlea)
The process of converting mechanical energy (vibrations) into electrical nerve impulses occurs within the hair cells of the organ of Corti, located in the cochlea. This critical step is known as auditory transduction.
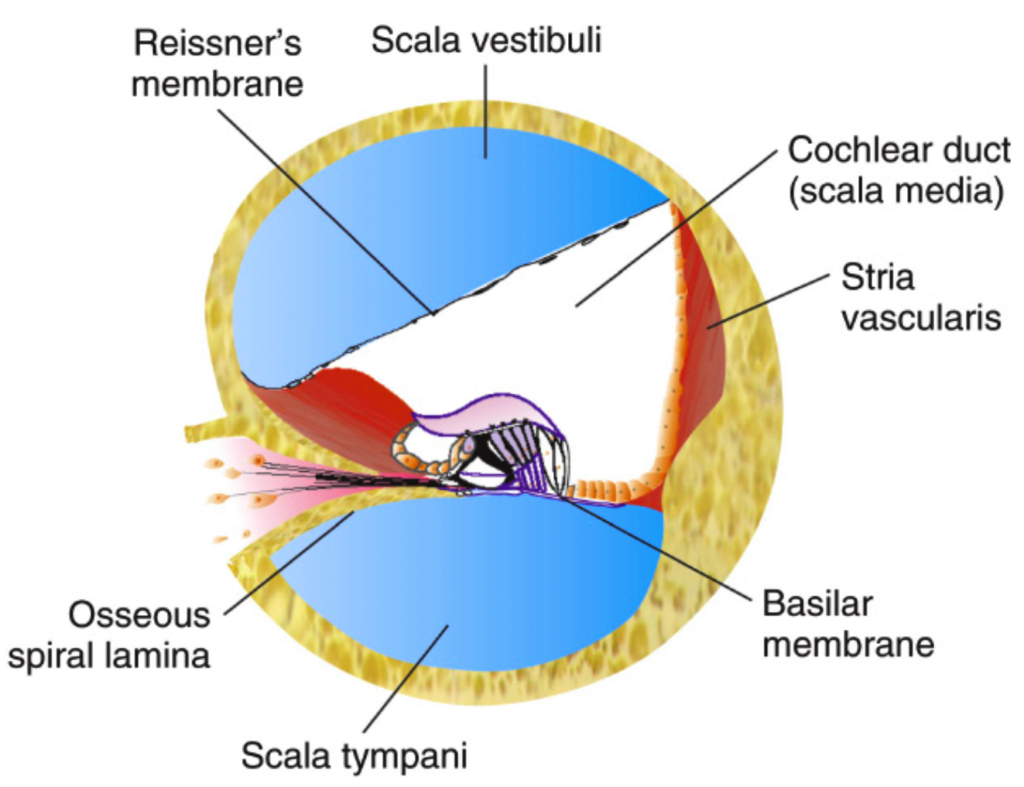
- Initial Mechanical Input: The stapes footplate is intimately connected to the oval window, which is in direct contact with the scala vestibuli, filled with perilymph.
- Fluid Movement: Movements of the stapes footplate create pressure changes in the perilymph of the scala vestibuli. These pressure waves are then transmitted across Reissner’s membrane to the scala media, which contains endolymph.
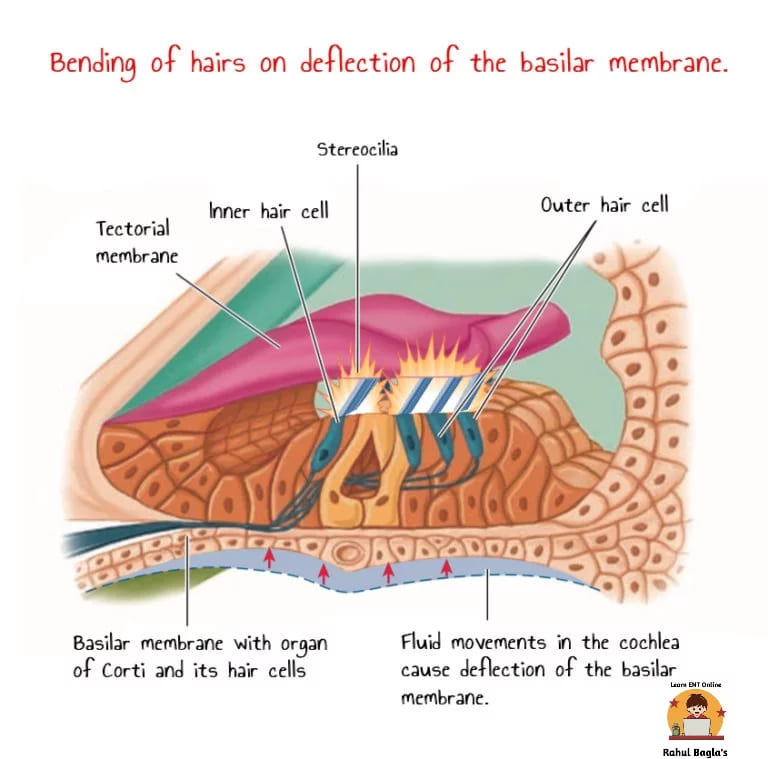
- Basilar Membrane Deflection: The pressure wave in the endolymph causes the basilar membrane to deflect relative to the relatively stationary tectorial membrane. This differential movement generates shearing forces that distort and bend the stereocilia (hairs) of the hair cells.
- Ion Channel Opening and Receptor Potential: The bending of stereocilia mechanically opens cation channels (primarily K+ and Ca+) located at their tips. This opening leads to an influx of these ions, particularly K+ from the endolymph (which has a high K+ concentration of 150 mEq/L due to the stria vascularis’s Na+/K+-ATPase pump). This ion movement results in a change in the hair cell’s membrane potential, generating a receptor potential.
- Depolarization and Hyperpolarization:
- When the organ of Corti moves upward (due to a compression wave), the tectorial membrane slides forward relative to the basilar membrane. This action bends the stereocilia away from the limbus (towards the outer wall), causing depolarization of the hair cell (the resting membrane potential of -60mV shifts to approximately -50mV).
- Conversely, when the organ of Corti moves downward (due to a rarefaction wave), the tectorial membrane slides backward relative to the basilar membrane. This bends the stereocilia towards the limbus, causing hyperpolarization of the hair cell.
- Neurotransmitter Release: Depolarization of the hair cell leads to the release of neurotransmitters (e.g., glutamate) from the hair cell onto the afferent nerve fibers of the cochlear nerve. This initiates action potentials in these auditory neurons.
Electrical Responses of Hair Cells (Cochlear Potentials)
Specialised microelectrodes can record four distinct electrical potentials from the ear, which are crucial for diagnosing various auditory disorders.
- Endocochlear Potential:
-
- Nature: This is a stable direct current (DC) potential of approximately +80 mV recorded from the scala media. It exists continuously under resting conditions, even without any external auditory stimulus.
- Source: The stria vascularis within the scala media actively maintains this potential by pumping K+ ions into the endolymph. The endolymph consequently has a significantly higher concentration of K+ (150 mEq/L) compared to the perilymph (3 mEq/L).
- Function: This substantial positive potential acts as a vital energy source or “battery” for cochlear transduction, providing the electrochemical gradient necessary for K+ influx into the hair cells upon stereocilia deflection.
- Cochlear Microphonic Potential (CM):
-
- Nature: This is an alternating current (AC) potential that mirrors the waveform of the auditory stimulus. It is recorded extracellularly when sound is presented to the ear.
- Source: The CM represents the sum of the receptor potentials from a large number of hair cells. When the basilar membrane moves in response to a sound stimulus, the electrical resistance at the tips of the hair cells changes, allowing the flow of K+ through them and producing these voltage fluctuations.
- Diagnostic Use: CM can be recorded in response to sound stimuli and is used in electrocochleography (ECoG) to assess hair cell function.
- Summating Potential (SP):
-
- Nature: This is a direct current (DC) potential that appears superimposed on the auditory nerve action potential.
- Source: Like CM, SP is also a receptor potential generated by the hair cells, reflecting the sustained DC shifts in hair cell membrane potential.
- Diagnostic Use: The SP, particularly the ratio of SP to the Compound Action Potential (SP/AP ratio), is significantly elevated in the diagnosis of Meniere’s disease.
- Key Differences from Action Potentials: Both Cochlear Microphonics and Summating Potentials are receptor potentials, similar to those seen in other sensory end-organs. However, they fundamentally differ from action potentials:
- They are graded potentials, not all-or-none action potentials.
- They are not propagated along nerve fibers.
- They exhibit no post-response refractory period.
- They have no latency (they occur instantaneously with the stimulus).
- Compound Action Potential (CAP):
-
- Nature: This is an all-or-none response that reflects the synchronous firing of a large population of auditory nerve fibers in response to an auditory stimulus.
- Source: CAP is generated by the first-order neurons (bipolar cells of the spiral ganglion) of the auditory pathway.
- Diagnostic Use: CAP is a fundamental component of Auditory Brainstem Response (ABR) testing, which assesses the integrity of the auditory nerve and brainstem pathways.
Table: Cochlear Potentials
| Potential | Nature | Location Recorded | Characteristics | Clinical Significance |
|---|---|---|---|---|
| Endocochlear Potential | DC | Scala Media | +80 mV, present at rest; Maintained by Stria Vascularis (K+ pump). | Provides energy for transduction. |
| Cochlear Microphonic (CM) | AC | Extracellularly (e.g., Scala Media vs. Tympani) | Mirrors sound waveform; Sum of hair cell receptor potentials; Graded, non-propagated. | Assesses hair cell function (ECoG). |
| Summating Potential (SP) | DC | Superimposed on AP | Sustained DC shift; Hair cell receptor potential; Graded, non-propagated. | Elevated SP/AP ratio in Meniere's disease (ECoG). |
| Compound Action Potential (CAP) | All-or-none | Auditory Nerve Fibers | Synchronous firing of 1st order neurons; Propagated. | Used in ABR testing (Auditory Brainstem Response). |
3. Conduction of Electrical Impulses to the Brain (Neural Pathways)
Once the hair cells transduce mechanical vibrations into electrical signals, these impulses travel along a complex series of neural pathways to reach the auditory cortex for processing and interpretation. This pathway involves a sequence of critical relay stations.
Mnemonics for Auditory Pathway: “E COLI-MA”
- Eight nerve (Auditory/Vestibulocochlear Nerve)
- Cochlear Nucleus (in medulla)
- Olivary complex (Superior Olivary Nucleus in pons)
- Lateral Lemniscus (tract in pons/midbrain)
- Inferior Colliculus (in midbrain)
- Medial Geniculate Body (in thalamus)
- Auditory Cortex (in temporal lobe)
Detailed Neural Transmission within the Auditory Pathways:
- First-Order Neurons (Bipolar Cells of the Spiral Ganglion):
-
- The dendrites of the bipolar cells located in the spiral ganglion (within the modiolus of the cochlea) directly innervate the hair cells.
- The axons of these bipolar cells coalesce to form the cochlear division of the eighth cranial nerve (vestibulocochlear nerve).
- These axons terminate and synapse in the cochlear nuclei (dorsal and ventral) located in the upper part of the medulla oblongata of the brainstem.
- Second-Order Neurons (Superior Olivary Nucleus Complex and Nucleus of the Lateral Lemniscus):
-
- From the cochlear nuclei, fibers primarily cross to the contralateral side of the brainstem. However, some fibers also ascend ipsilaterally. This decussation is crucial for sound localization.
- These fibers synapse in the superior olivary nucleus complex, located in the pons. The superior olivary complex is particularly important for sound localization by comparing interaural time differences and intensity differences.
- Some fibers also synapse in the nucleus of the lateral lemniscus.
- Third-Order Neurons:
-
- These neurons, with cell bodies in the superior olivary complex, trapezoid nucleus, and nucleus of the lateral lemniscus, project rostrally.
- They ascend through the lateral lemniscus, a major auditory tract in the brainstem.
- These fibers terminate and synapse in the inferior colliculus, located in the midbrain. The inferior colliculus serves as a major integrative center for auditory information.
- Fourth-Order Neurons:
-
- Neurons located in the inferior colliculus send their projections to the medial geniculate body (MGB) of the thalamus. The MGB acts as the final subcortical relay station for auditory information before it reaches the cerebral cortex.
- Fifth-Order Neurons:
-
- These are the final relay of neurons. Their axons originate from the medial geniculate body and project to the auditory cortex (Brodmann’s areas 41 and 42) in the temporal lobe (specifically, the transverse temporal gyri of Heschl).
- Primary Auditory Cortex (Area 41, 42): This area is responsible for the conscious perception of sound, including its basic characteristics like pitch and loudness.
- Auditory Association Areas (Areas 22, 21, and 20): These areas surround the primary auditory cortex and are crucial for the interpretation and understanding of sounds, including speech, music, and complex environmental sounds. For instance, Wernicke’s area (part of area 22) is critical for language comprehension.
Table: Auditory Pathway Relay Stations (E COLI-MA)
| Neuron Order | Relay Station | Location | Key Function |
|---|---|---|---|
| 1st Order | Spiral Ganglion Cells | Modiolus (Cochlea) | Innervate hair cells; Axons form Cochlear Nerve (part of CN VIII); Terminate in Cochlear Nuclei. |
| 2nd Order | Cochlear Nuclei | Medulla Oblongata | Receive input from 1st order neurons; Begin processing of sound features. |
| Superior Olivary Complex | Pons | Crucial for sound localization (interaural time/intensity differences); Receives input from both cochlear nuclei. | |
| 3rd Order | Nucleus of Lateral Lemniscus | Pons/Midbrain | Ascends through Lateral Lemniscus; Some fibers from Cochlear Nuclei may bypass SOC and go directly here. |
| Inferior Colliculus | Midbrain | Major integrative center; Involved in auditory reflexes, sound localization, and frequency processing. | |
| 4th Order | Medial Geniculate Body (MGB) | Thalamus (Ventral part) | Final subcortical relay; Projects to auditory cortex; Involved in attention to sound. |
| 5th Order | Auditory Cortex | Temporal Lobe (Brodmann's areas 41, 42, 22, 21, 20) | Conscious perception of sound (pitch, loudness); Interpretation of complex sounds (speech, music, Wernicke's area). |
Neural Processing of Auditory Information
The human auditory system is remarkably sophisticated, capable of detecting sounds within the frequency range of 20-20,000 Hz. Furthermore, it can perform complex analyses of sound attributes:
- Sound Intensity Encoding: Sound intensity (loudness) is encoded at the level of the cochlear nerve fibers. This involves various mechanisms, including the rate of firing of individual nerve fibers and the number of active fibers, allowing higher auditory centers to accurately perceive loudness.
- Sound Localization: The auditory system possesses an impressive ability to distinguish sounds from sources separated by as little as 1 degree. It primarily achieves this by utilizing two key cues:
- Interaural Time Difference (ITD): For low-frequency sounds (below 3000 Hz), the brain detects minute time lags between the sound arriving at each ear. If a sound originates from the right, it reaches the right ear slightly before the left ear.
- Interaural Intensity Difference (IID): For high-frequency sounds (above 3000 Hz), the head acts as an acoustic shadow, causing the sound to be slightly louder in the ear closer to the source.
- Clinical Correlation: Lesions in the auditory cortex can significantly disrupt a person’s ability to localize sounds, even if their basic hearing thresholds remain relatively intact.
Key Terminologies
- Amplitude (Intensity): Refers to the loudness of the sound, measured in decibels (dB).
- Frequency: Indicates the number of sound waves produced per second, measured in hertz (Hz). Human hearing ranges from approximately 20 to 20,000 Hz, with normal speech frequencies ranging from 2000 to 5000 Hz.
- Pitch: The subjective sensation corresponding to the frequency of sound. Higher frequencies result in higher pitches. The average male voice has a pitch of 120 Hz, while the average female voice has a pitch of 250 Hz. An average individual can distinguish approximately 2000 different pitches.
- Pure Tone: A sound with a single frequency, such as 250, 500, or 1000 Hz. Pure tone audiometry measures the hearing threshold in decibels for various pure tones ranging from 125 to 8000 Hz.
- Complex Sound: Comprises multiple frequencies. The human voice is an example of a complex sound.
- Sound Pressure: Expressed in decibels (dB), a relative measure on a logarithmic scale.
- Overtones: A complex sound consists of a mixture of pure tones. The lowest frequency at which a source vibrates is termed the fundamental (or primary) frequency. Other frequencies, which are multiples of the fundamental frequency, are called overtones or harmonics. Overtones determine the quality or timbre of sound, enabling the identification of different musical instruments playing the same pitch.
———— End of the chapter ————
High-Yield Points for Quick Revision
- Hearing Mechanism Stages: Mechanical conduction (external/middle ear), Transduction (cochlea), Neural conduction (auditory pathway).
- Sound Transmission Loss: ~30 dB lost when sound moves from air to liquid, overcome by impedance matching.
- Impedance Matching Components: Lever action of ossicles (1.3x), Hydraulic action of tympanic membrane (17x effective ratio).
- Total Amplification: ~18-22 times (25-30 dB gain).
- Attenuation Reflex (Acoustic Reflex): Protective, triggered by loud sounds (>70-80 dB HT), involves tensor tympani and stapedius.
- Attenuation Reflex Latency: ~40 ms, provides protection against prolonged loud sounds, not sudden impulses.
- Phase Differential: Oval and round windows vibrate out of phase, crucial for cochlear fluid movement (adds ~4 dB).
- Resonant Frequencies: EAC (~3000 Hz), Tympanic membrane (~800-1600 Hz), Middle ear (~800 Hz), Ossicular chain (~500-2000 Hz).
- Human Hearing Range: 20 Hz – 20,000 Hz; maximum sensitivity 1000-3000 Hz.
- Auditory Transduction: Mechanical bending of stereocilia opens K+ channels, leading to depolarization.
- Endocochlear Potential: +80mV DC potential in scala media, maintained by stria vascularis (K+ pump), provides driving force for transduction.
- Cochlear Microphonic (CM): AC potential, mirrors sound waveform, sum of hair cell receptor potentials.
- Summating Potential (SP): DC potential, hair cell receptor potential, elevated SP/AP ratio diagnostic for Meniere’s disease.
- Compound Action Potential (CAP): All-or-none response of auditory nerve fibers (first-order neurons).
- Auditory Pathway Mnemonic: E COLI-MA (Eight nerve, Cochlear nucleus, Olivary complex, Lateral lemniscus, Inferior colliculus, Medial geniculate body, Auditory cortex).
- Sound Localization Cues: Interaural Time Difference (ITD) for low frequencies, Interaural Intensity Difference (IID) for high frequencies.
- Superior Olivary Complex: Key brainstem nucleus for sound localization.
- Medial Geniculate Body (MGB): Thalamic relay for auditory information.
- Primary Auditory Cortex: Brodmann’s areas 41, 42 in temporal lobe (Heschl’s gyri).
MCQs: Physiology of Hearing – For NEET PG & University Exams
- What is the primary function of the external auditory meatus in hearing?
A. Amplify sound intensity
B. Conduct sound waves to the tympanic membrane
C. Localize sound source
D. Protect the inner ear - What is the speed of sound in air at 20°C and sea level?
A. 300 m/s
B. 344 m/s
C. 400 m/s
D. 500 m/s - Which mechanism primarily addresses the 99.9% sound energy reflection at the air-liquid interface?
A. Attenuation reflex
B. Impedance matching
C. Phase differential
D. Natural resonance - What is the total amplification factor of the middle ear due to lever and hydraulic actions, as per the primary text?
A. 14:1
B. 17:1
C. 18:1
D. 22.1:1 - Which muscle contracts during the attenuation reflex to restrict ossicular movement?
A. Tensor veli palatini
B. Stapedius
C. Levator tympani
D. Mylohyoid - What is the human auditory system’s frequency detection range?
A. 10–10,000 Hz
B. 20–20,000 Hz
C. 50–50,000 Hz
D. 100–100,000 Hz - In auditory transduction, what causes depolarization of hair cells?
A. Oval window vibration
B. Stereocilia bending
C. Round window movement
D. Perilymph flow - Which potential is used diagnostically for Meniere’s disease?
A. Endo-cochlear potential
B. Cochlear microphonic
C. Summating potential
D. Compound action potential - According to the E COLI-MM mnemonic, which structure follows the cochlear nucleus in the auditory pathway?
A. Eighth nerve
B. Olivary complex
C. Inferior colliculus
D. Medial geniculate body - What is the natural resonance frequency of the ossicular chain?
A. 800 Hz
B. 1600 Hz
C. 3000 Hz
D. 500–2000 Hz - Clinical Scenario: A 28-year-old male presents with sudden sensorineural hearing loss after exposure to a loud explosion at a construction site. Which mechanism’s failure likely contributed to his cochlear damage?
A. Impedance matching
B. Attenuation reflex
C. Phase differential
D. Auditory transduction - Clinical Scenario: A 45-year-old female reports episodic vertigo, tinnitus, and hearing loss. Electrocochleography reveals an elevated summating potential. What is the most likely diagnosis?
A. Otosclerosis
B. Meniere’s disease
C. Acoustic neuroma
D. Presbycusis - Clinical Scenario: A 35-year-old male with chronic otitis media presents with conductive hearing loss. Which middle ear component is most likely affected, disrupting sound conduction?
A. Pinna
B. Ossicular chain
C. Cochlea
D. Semicircular canals - Clinical Scenario: A patient’s otoscopy shows a non-vibrating tympanic membrane during loud sound exposure, suggesting attenuation reflex dysfunction. Which muscle is primarily implicated?
A. Tensor tympani
B. Sternocleidomastoid
C. Masseter
D. Buccinator - Clinical Scenario: A 30-year-old female reports difficulty localizing sounds in crowded places. An MRI reveals a temporal lobe lesion. Which cortical area is most likely affected?
A. Brodmann’s area 41
B. Brodmann’s area 17
C. Brodmann’s area 4
D. Brodmann’s area 8 - Clinical Scenario: A 40-year-old male undergoes pure tone audiometry, revealing a hearing threshold elevation at 4000 Hz. What is the most likely underlying cause?
A. External auditory canal obstruction
B. Ossicular chain fixation
C. Cochlear hair cell damage
D. Auditory cortex lesion - Clinical Scenario: A 55-year-old factory worker presents with difficulty understanding speech in noisy environments. Which frequency range, critical for conversation, is most likely affected?
A. 100–500 Hz
B. 1000–3000 Hz
C. 5000–8000 Hz
D. 10,000–15,000 Hz - Clinical Scenario: A patient with suspected ossicular discontinuity is evaluated. What is the expected effect on sound transmission to the cochlea?
A. Increased sound pressure
B. Reduced oval window pressure
C. Enhanced phase differential
D. Unaltered transduction - Clinical Scenario: A 32-year-old female with tinnitus and unilateral hearing loss shows an abnormal compound action potential on testing. Which structure is most likely affected?
A. Tympanic membrane
B. Auditory nerve
C. External auditory meatus
D. Tectorial membrane - Clinical Scenario: During stapedectomy, an ENT surgeon notes a fixed stapes footplate. Which hearing mechanism is primarily disrupted?
A. Attenuation reflex
B. Impedance matching
C. Neural conduction
D. Natural resonance
- Which of the following contributes to the phase differential between the oval and round windows?
Tensor tympani contraction
B. Ossicular coupling
C. Cochlear microphonic potential
D. Endo-cochlear potential - A patient with noise-induced hearing loss shows a dip at 4000 Hz on audiometry. Which structure is primarily damaged?
Tympanic membrane
B. Ossicular chain
C. Organ of Corti
D. Auditory cortex - The auditory cortex is located in which Brodmann’s area?
Area 17
B. Area 41
C. Area 4
D. Area 8 - Which of the following potentials is a graded, non-propagated response used in diagnosing Meniere’s disease?
Compound action potential
B. Endo-cochlear potential
C. Summating potential
D. Action potential - A patient with conductive hearing loss has a disrupted ossicular chain. What is the primary mechanism affected?
Auditory transduction
B. Impedance matching
C. Neural conduction
D. Sound localization
Answers with Detailed Explanations
- B. Conduct sound waves to the tympanic membrane: The external auditory meatus channels sound waves to the tympanic membrane, causing it to vibrate. Amplification (A) occurs in the middle ear, localization (C) is primarily the pinna’s role, and protection (D) is secondary.
- B. 344 m/s: The text specifies sound travels at 344 m/s in air at 20°C and sea level. Options A, C, and D are incorrect as they deviate from this value.
- B. Impedance matching: Impedance matching overcomes the 99.9% sound energy reflection at the air-liquid interface using ossicular lever action (1.3x), hydraulic action (14:1), and curved tympanic membrane effect. Attenuation reflex (A) protects against loud sounds, phase differential (C) aids fluid movement, and natural resonance (D) enhances frequencies, but none address reflection.
- C. 18:1: The text states the product of the areal ratio (14:1) and lever action (1.3x) yields 18:1 amplification. Option D (22.1:1) is from Wever and Lawrence’s study, not the primary text. Options A and B are incorrect ratios.
- B. Stapedius: The stapedius muscle, along with tensor tympani, contracts during the attenuation reflex to restrict ossicular movement for loud sounds (>70 dB). Other options (A, C, D) are unrelated to the middle ear.
- B. 20–20,000 Hz: The text confirms the human auditory range is 20–20,000 Hz. Other options are either too narrow or too broad.
- B. Stereocilia bending: Stereocilia bending in the organ of Corti opens cation channels, causing depolarization during auditory transduction. Oval window (A) initiates perilymph movement, round window (C) facilitates fluid dynamics, and perilymph flow (D) is indirect.
- C. Summating potential: The summating potential, a DC receptor potential, is used to diagnose Meniere’s disease. Endo-cochlear potential (A) is resting, cochlear microphonic (B) is AC, and compound action potential (D) is neural.
- B. Olivary complex: The mnemonic E COLI-MM (Eighth nerve, Cochlear nucleus, Olivary complex, Lateral lemniscus, Inferior colliculus, Medial geniculate body, Auditory cortex) indicates the olivary complex follows the cochlear nucleus. Other options are incorrect in sequence.
- D. 500–2000 Hz: The ossicular chain’s natural resonance is 500–2000 Hz, contributing to conversational frequency amplification. Other options refer to different structures or are incorrect.
- B. Attenuation reflex: The attenuation reflex (stapedius, tensor tympani) protects against loud sounds (>70 dB) but has a 40 ms latency, failing to shield the cochlea from sudden noises like explosions, causing sensorineural hearing loss. Impedance matching (A) amplifies sound, phase differential (C) aids fluid movement, and transduction (D) is a cochlear process, none protective.
- B. Meniere’s disease: Elevated summating potential on electrocochleography, with vertigo, tinnitus, and hearing loss, indicates Meniere’s disease due to endolymphatic hydrops. Otosclerosis (A) causes conductive loss, acoustic neuroma (C) affects the auditory nerve, and presbycusis (D) is age-related, none linked to summating potential.
- B. Ossicular chain: Chronic otitis media can erode the ossicular chain, disrupting impedance matching and causing conductive hearing loss. Pinna (A) and meatus (C) are external, cochlea (C) causes sensorineural loss, and semicircular canals (D) affect balance.
- A. Tensor tympani: A non-vibrating tympanic membrane during loud sounds suggests attenuation reflex dysfunction, primarily involving the tensor tympani, which pulls the malleus inward. Stapedius (not an option) also contributes, but other muscles (B, C, D) are irrelevant.
- A. Brodmann’s area 41: The auditory cortex (Brodmann’s area 41) processes sound localization; lesions impair this ability. Area 17 (B) is visual, area 4 (C) is motor, and area 8 (D) controls eye movement.
- C. Cochlear hair cell damage: A 4000 Hz dip on audiometry indicates sensorineural hearing loss from cochlear hair cell damage, common in noise exposure. External canal obstruction (A) or ossicular fixation (B) cause conductive loss, and cortical lesions (D) affect localization.
- B. 1000–3000 Hz: The minimum audibility curve shows peak sensitivity at 1000–3000 Hz, critical for conversational speech. Noise exposure likely damages this range. Other ranges (A, C, D) are less relevant for speech.
- B. Reduced oval window pressure: Ossicular discontinuity disrupts impedance matching, reducing pressure transmission to the oval window, causing conductive hearing loss. It doesn’t increase pressure (A), enhance phase differential (C), or affect transduction (D).
- B. Auditory nerve: An abnormal compound action potential indicates auditory nerve dysfunction, common in tinnitus and hearing loss (e.g., acoustic neuroma). Other structures (A, C, D) affect earlier stages.
- B. Impedance matching: A fixed stapes (e.g., otosclerosis) disrupts impedance matching, reducing pressure transfer to the oval window. Attenuation reflex (A), neural conduction (C), and resonance (D) are unaffected.
- Ossicular coupling: Ossicular coupling, part of the intact tympano-ossicular system, ensures the oval window vibrates preferentially, creating a phase differential with the round window (+4 dB gain). Tensor tympani (A) is for attenuation, cochlear microphonic (C) is a transduction potential, and endo-cochlear potential (D) powers transduction.
- Organ of Corti: A 4000 Hz dip indicates noise-induced sensorineural hearing loss due to organ of Corti hair cell damage. Tympanic membrane (A) and ossicles (B) cause conductive loss, and auditory cortex (D) affects localization.
- Area 41: The primary auditory cortex is Brodmann’s area 41, per the text. Area 17 (A) is visual, area 4 (C) is motor, and area 8 (D) controls eye movement.
- Summating potential: Summating potential, a graded, non-propagated DC potential, is diagnostic for Meniere’s disease. Compound action potential (A) is neural, endo-cochlear (B) is resting, and action potential (D) is generic.
- Impedance matching: Ossicular chain disruption impairs impedance matching, reducing sound transmission to the cochlea, causing conductive hearing loss. Transduction (A), neural conduction (C), and localization (D) are unaffected.
FAQ’s in Viva
- Q: What is impedance matching in hearing? A: Impedance matching is the process by which the middle ear, through the hydraulic action of the tympanic membrane and the lever action of the ossicles, amplifies sound pressure to overcome the energy loss that occurs when sound travels from air to the fluid-filled inner ear.
- Q: What is the function of the attenuation (acoustic) reflex? A: The attenuation reflex is a protective reflex involving the contraction of the middle ear muscles (tensor tympani and stapedius) in response to loud sounds, thereby stiffening the ossicular chain and reducing sound transmission to the inner ear, thus protecting the cochlea.
- Q: Which structures are involved in sound localization? A: Sound localization primarily involves the superior olivary complex in the brainstem, which analyzes interaural time differences (for low frequencies) and interaural intensity differences (for high frequencies) between the two ears.
- Q: What is the endocochlear potential? A: The endocochlear potential is a stable positive direct current (+80 mV) within the endolymph of the scala media, maintained by the stria vascularis, which provides the electrochemical gradient necessary for auditory transduction.
- Q: What is the significance of an elevated SP/AP ratio in ECoG? A: An elevated Summating Potential (SP) to Compound Action Potential (AP) ratio in electrocochleography (ECoG) is a key diagnostic indicator for Meniere’s disease, reflecting endolymphatic hydrops.
- Q: Name the main relay stations in the auditory pathway to the brain. A: The main relay stations in the auditory pathway are the cochlear nuclei, superior olivary complex, inferior colliculus, medial geniculate body (thalamus), and finally the auditory cortex in the temporal lobe.
- Q: Why do sound waves not travel efficiently from air to liquid? A: Sound waves are largely reflected when moving from air to liquid because liquids have a much higher acoustic impedance (resistance to sound propagation) compared to air, leading to significant energy loss at the interface.
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: PPT Free Download, Mechanism, Flowchart, Diagram, Notes, Auditory physiology, Cochlear function, Basilar membrane movement, Sound transduction, Hair cell depolarization, Auditory neural pathway, Endolymphatic potential, Cochlear microphonics, Tonotopic organization, Middle ear amplification, Oval window vibration, Inner ear hair cells, Otolithic membrane, Stereocilia deflection, Auditory nerve action potential, Brainstem auditory processing, Temporal coding in hearing, Physiology of Hearing


Dear Dr. Rahul,
I am a retired professor from Kerala Veterinary & Animal Sciences University. Even though my specialization is Dairy quality control (Basically Veterinary graduate)I am interested to teach basic science to school children. Came across your online text. Very useful for learners. Your generation should come up with such contents. Congratulations and keep in touch
Thank you so much sir.
Regards
Dr Rahul Bagla
Layyah
Sir can u upload a PPT as well. The topic is very good for reading.
An invaluable resource for understanding the physiology, Very Good.
Hello sir
I am James Otieno, PG Resident, Kenyatta University, Kenya.
Good book for academic and practical learning.
I’m grateful to have found yor book.
Thanks
Buenos dias estimado soy residente de otorrinolringologia, en Arequipa Peru, primeramente felicitarlo por su excelente trabajo, quisiera saber donde puedo conseguir el libro completo en PDF