|
The following CBME core competencies are covered in this chapter.
|
Hearing Loss
Hearing is one of our most important senses, which connects us to the world and facilitates communication. Hearing loss is defined as an impairment of auditory function, which can significantly impact an individual’s quality of life. This impairment can range from mild to profound, or even result in total loss of hearing, often referred to as deafness. The term “deafness” refers to a condition characterised by little to no hearing ability.
Understanding the various types of hearing loss, their underlying mechanisms, and appropriate management strategies is fundamental for every medical student and future ENT specialist. Therefore, this chapter provides a clear, comprehensive, and exam-oriented overview, ensuring you master this critical topic.
Types of Hearing Loss
Hearing loss is categorised into distinct types based on the anatomical location of the pathology:
- Conductive Hearing Loss (CHL): Outer or middle ear.
- Sensorineural Hearing Loss (SNHL): Inner ear (cochlea) or auditory nerve.
- Mixed Hearing Loss: Combination of both.
- Central Hearing Loss: Auditory processing centres in the brain.
- Non-organic/Functional Hearing Loss: No organic cause (psychogenic or malingering).
WHO Classification of Hearing Loss
The World Health Organisation (WHO) established a grading system for hearing loss in 1980. This system is based on pure tone audiometry, which measures the average hearing threshold at frequencies of 500, 1000, and 2000 Hertz in the better ear. The following table summarises the WHO grading of hearing loss:

Assessment of Hearing Loss
To diagnose the specific type of loss, a clinical evaluation determines four key factors:
- Type of Hearing Loss: Differentiating between conductive, sensorineural, or mixed.
- Degree of Hearing Loss: Categorised from mild to total loss (as per the WHO table above).
- Site of the Lesion:
- Conductive: External ear, tympanic membrane, middle ear, ossicles, or eustachian tube.
- Sensorineural: Cochlear (sensory), Retrocochlear (neural, 8th nerve), or Central (affecting higher auditory pathways).
- Cause of Hearing Loss: Congenital, traumatic, infective, neoplastic, etc. A comprehensive patient history and laboratory investigations are crucial for identifying the underlying cause.
Key Diagnostic Tools:
- Tuning Fork Tests: Differentiate CHL from SNHL.
- Pure Tone Audiometry (PTA): The gold standard for quantifying loss.
- Tympanometry: Useful for identifying middle ear fluid or ossicular issues.
- Special Tests: ABR (Auditory Brainstem Response) or OAE (Otoacoustic Emissions) for retrocochlear or difficult-to-test cases.
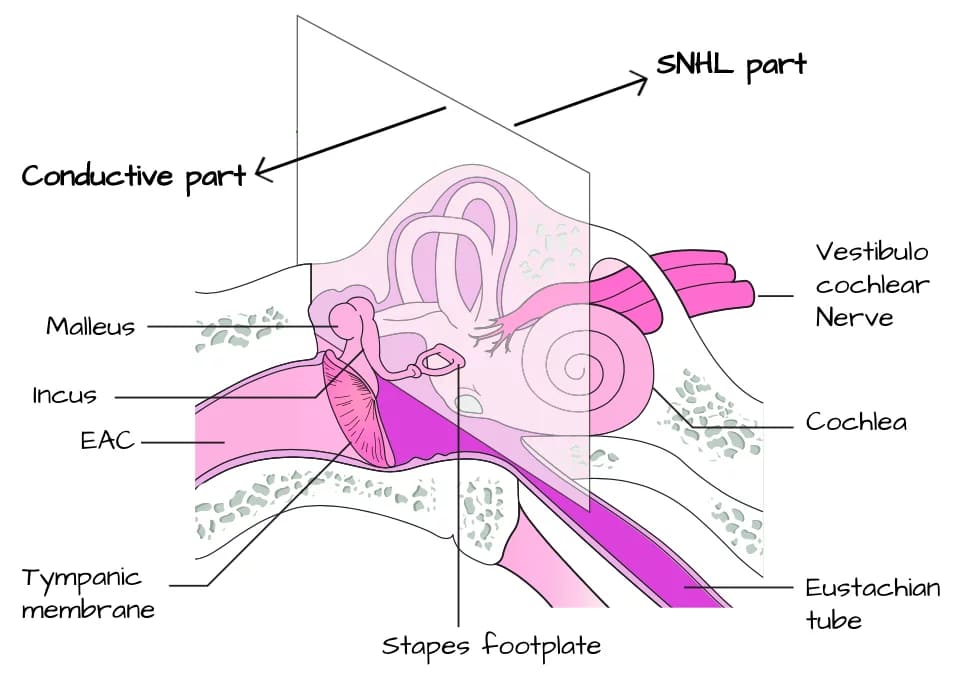
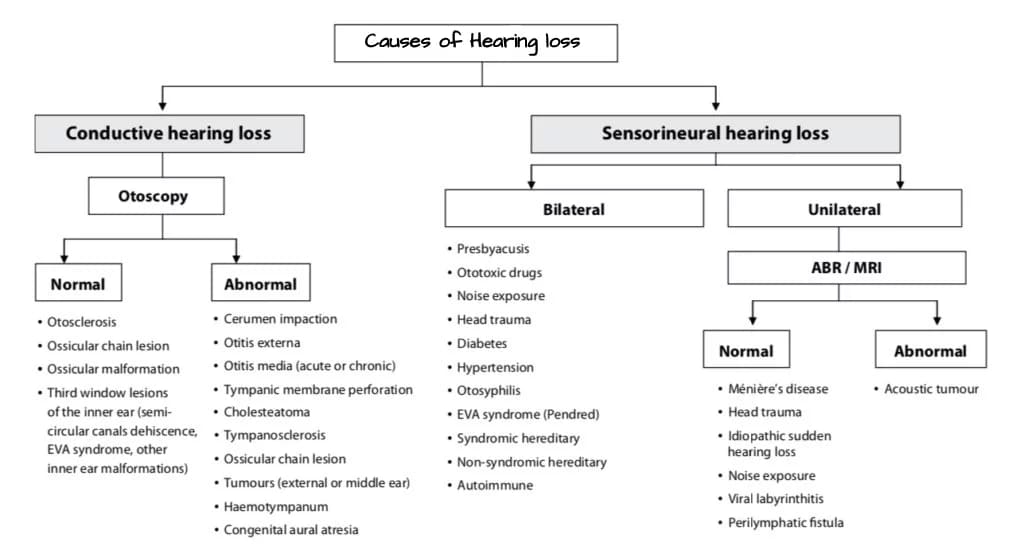
Conductive Hearing Loss (CHL)
Conductive hearing loss arises from obstructions in the transmission of sound waves along the auditory pathway, which extends from the external ear to the cochlea, specifically at the stapediovestibular joint.
Common causes of conductive hearing loss include: (Mnemonic: O-T-M-E-O)
- Obstruction in External Ear Canal: Impacted cerumen (earwax) is the most common cause, Foreign bodies, Osteomas or exostoses (bony growths in the canal), Keratotic masses (e.g., cholesteatoma of EAC), Benign or malignant tumours of the EAC, Meatal atresia (congenital narrowing or absence of the canal).
- Tympanic Membrane (TM) Pathology: Perforations (due to trauma, infection), Tympanosclerosis (scarring/calcification of TM), Retraction pockets.
- Middle Ear Disorders: Presence of fluid: Otitis Media with Effusion (OME), also known as “glue ear.” Acute otitis media (AOM) or Chronic Suppurative Otitis Media (CSOM), Hemotympanum (blood in the middle ear, often post-traumatic).
- Ossicular Chain Pathology: Ossicular fixation: Most commonly otosclerosis (fixation of stapes footplate). Also, malleus head fixation, fibrous ankylosis. Ossicular disruption/discontinuity: Due to trauma (e.g., temporal bone fracture), cholesteatoma erosion, or chronic infection.
- Eustachian Tube Dysfunction: Obstructions affecting pressure equalisation in the middle ear, leading to fluid accumulation (OME), Barotrauma.
Characteristics of Conductive Hearing Loss:
| Feature | Conductive Hearing Loss Characteristics |
|---|---|
| Rinne Test | Negative (BC > AC in affected ear). This is a hallmark. |
| Weber Test | Lateralizes to the poorer (affected) ear. The sound is perceived louder in the ear with the conductive loss. |
| Absolute Bone Conduction | Normal (or near normal) levels. The cochlea and nerve are intact. |
| Frequency Impact | Greater impact on low frequencies. (However, large perforations can affect all frequencies). |
| Degree of Loss | Typically does not exceed 60 dB HL. This is because bone conduction is intact. |
| Speech Discrimination | Remains good. Patients hear speech but find it difficult to hear quiet sounds. They often speak softly themselves. |
| Hearing Aid Benefit | Excellent candidates for hearing aid amplification as the inner ear can effectively process amplified sound. |
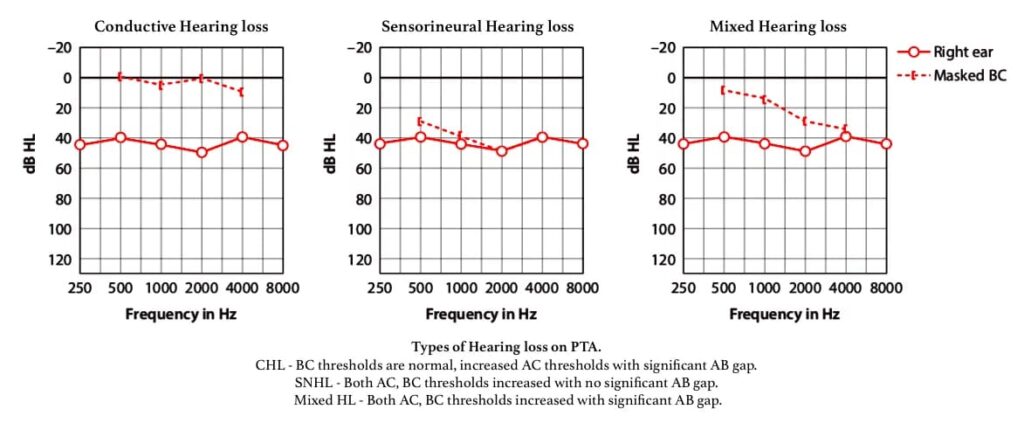
Characteristics of Conductive Hearing Loss on Pure Tone Audiometry (PTA)
- A difference of more than 10 dB between AC and BC thresholds at any frequency.
- BC thresholds are generally at normal hearing levels (equal to or better than 20 dB HL) in cases of pure conductive hearing loss.
- If BC thresholds exceed 20 dB HL with a significant air-bone gap (ABG), this condition is classified as mixed hearing loss.
Management of Conductive Hearing Loss
Management strategies for conductive hearing loss include:
- Removal of Canal Obstructions:
- Impacting cerumen or foreign bodies: Removal through irrigation or suction clearance.
- Osteomas/Exostoses: Surgical excision.
- Meatal atresia: Canaloplasty (surgical reconstruction of the EAC).
- Benign or malignant tumours: Surgery
- Medical Management:
- Otitis Media with Effusion (OME): Decongestants, antihistamines, and watchful waiting.
- Acute Otitis Media: Antibiotics.
- Surgical Interventions:
- Myringotomy with or without grommet insertion: To drain fluid from the middle ear (e.g., in OME).
- Myringoplasty: Surgical repair of the tympanic membrane perforation.
- Tympanoplasty: A broader operation to (i) eradicate disease from the middle ear and (ii) reconstruct the hearing mechanism, potentially with or without mastoid surgery and with or without tympanic membrane grafting.
- Ossiculoplasty: Surgical reconstruction of the ossicular chain (e.g., using prostheses or autologous ossicles).
- Stapedectomy/Stapedotomy: For otosclerosis, replacing the fixed stapes with a prosthesis.
- Hearing Aids:
- These devices are utilised when surgical options are not feasible, declined by the patient, or have previously failed.
Sensorineural Hearing Loss (SNHL)
Sensorineural hearing loss is the result of damage to the cochlea (sensory type) or the eighth cranial nerve and its central auditory pathways (neural type). This damage disrupts the process of cochlear transduction, where mechanical energy is converted into electrical impulses for transmission to the brain.
Subtypes:
- Sensory SNHL (Cochlear): It results from damage to the hair cells or other structures within the cochlea. This is the most common type of SNHL.
- Neural SNHL (Retrocochlear): It is caused by lesions affecting the eighth cranial nerve (vestibulocochlear nerve).
- Central Deafness: It results from lesions in the central auditory pathways. (Sometimes classified separately or as a subtype of SNHL).
Characteristics of Sensorineural Hearing Loss:
| Feature | Sensorineural Hearing Loss Characteristics |
|---|---|
| Rinne Test | Positive (AC > BC), but both are reduced. The sound is heard better by air, but softly, in the affected ear. |
| Weber Test | Lateralizes to the better (unaffected) ear. Sound is perceived louder in the ear with better cochlear function. |
| Bone Conduction | Reduced on Schwabach and absolute bone conduction tests. This reflects inner ear or neural damage. |
| Speech Discrimination | Poor speech discrimination. Patients often report, "I can hear people talking, but I can't understand what they're saying." |
| Hearing in Noise | Significant difficulty in hearing in the presence of background noise. |
| Recruitment Phenomenon | May be present (abnormal loudness growth). Loud sounds become disproportionately louder, often painful. Typical of cochlear SNHL. |
| Tinnitus | Frequently accompanied by tinnitus (ringing or buzzing in the ears). |
| Degree of Loss | Can range from minimal to profound or total loss, and is usually permanent. |
The characteristics of sensorineural hearing loss on PTA:
- AC and BC thresholds being within 10dB of each other.
- High frequencies are mostly involved.
- Loss may exceed 60 dB, generally complete hearing loss.
Aetiology of Sensorineural Hearing Loss:
SNHL can be broadly categorised into congenital (present at birth) and acquired (developing later in life) causes.
A. Congenital SNHL:
Congenital SNHL can result from inner ear anomalies (e.g., Mondini dysplasia) or prenatal/perinatal damage to the hearing apparatus.
TABLE: Syndromes associated with SNHL (Congenital)

B. Acquired SNHL:
Acquired SNHL develops after birth. It can have genetic (non-syndromic or syndromic) or non-genetic causes.
Common Causes of Acquired SNHL (CBME Focus):
- Infections of Labyrinth:
- Viral: Mumps, Measles, Rubella (congenital), Cytomegalovirus (CMV, congenital or acquired), Herpes Zoster Oticus (Ramsay Hunt syndrome – often unilateral, with facial paralysis and vesicles).
- Bacterial: Labyrinthitis as a complication of otitis media or meningitis.
- Spirochaetal: Syphilis, Lyme disease.
- Noise-Induced Hearing Loss (NIHL):
- Chronic exposure to loud noise (e.g., occupational, recreational). Typically presents as a notch at 4000 Hz on audiometry.
- Acoustic trauma (single loud blast).
- Ototoxic Drugs:
- Aminoglycosides (e.g., gentamicin, amikacin) – affect high frequencies initially.
- Loop diuretics (e.g., Furosemide) – usually reversible.
- Salicylates (e.g., aspirin in high doses) – usually reversible.
- Chemotherapeutic agents (e.g., cisplatin, carboplatin).
- Antimalarials (e.g., quinine, chloroquine).
- Presbycusis: Age-related hearing loss. The most common cause of SNHL in adults. Typically bilateral, symmetrical, and affecting high frequencies first.
- Sudden Sensorineural Hearing Loss (SSNHL): Acute onset SNHL (≥30 dB loss over ≥3 contiguous frequencies within 72 hours). Often idiopathic. Requires urgent evaluation.
- Meniere’s Disease: Characterised by episodic vertigo, fluctuating SNHL (typically low-frequency), tinnitus, and aural fullness. Due to endolymphatic hydrops.
- Acoustic Neuroma (Vestibular Schwannoma): Benign tumour of the vestibular division of the 8th cranial nerve. Typically causes unilateral, progressive SNHL, often with tinnitus and disequilibrium. Asymmetrical SNHL mandates an MRI brain with IAC protocol.
- Trauma to Labyrinth or VIIIth Nerve:
- Temporal bone fractures (especially trans-labyrinthine fractures).
- Barotrauma (e.g., diving injuries leading to perilymph fistula).
- Familial Progressive SNHL: Genetically inherited SNHL that develops and progresses over time.
- Systemic Disorders:
- Metabolic: Diabetes Mellitus, Hypothyroidism, Kidney disease.
- Autoimmune: Systemic lupus erythematosus (SLE), Rheumatoid arthritis, Cogan’s syndrome.
- Vascular: Vasculitis, stroke.
- Neurological: Multiple Sclerosis.
- Haematological: Sickle cell anaemia, polycythemia.
Management of Sensorineural Hearing Loss:
For most SNHL, medical or surgical interventions are very limited, as the damage to the cochlea or nerve is often irreversible.
- Hearing Aids: The primary mode of rehabilitation for most SNHL. These amplify sound to compensate for the reduced sensitivity.
- Cochlear Implants: For severe-to-profound SNHL where hearing aids provide insufficient benefit. These surgically implanted devices bypass the damaged cochlea and directly stimulate the auditory nerve.
- Auditory Brainstem Implants (ABIs): For SNHL caused by damage to the auditory nerve (e.g., bilateral acoustic neuromas due to Neurofibromatosis Type 2), bypassing the nerve and directly stimulating the brainstem.
- Medical Management (for specific causes):
- Sudden SNHL: Oral corticosteroids (often with intratympanic steroids).
- Meniere’s Disease: Dietary modifications (low salt), diuretics, intratympanic steroids/gentamicin, sacculotomy, endolymphatic sac decompression.
- Autoimmune inner ear disease: Immunosuppressants (e.g., steroids).
- Infections: Appropriate antimicrobials.
- Acoustic Neuroma: Observation, Stereotactic Radiosurgery, or Surgical Excision.
- Aural Rehabilitation: Speech therapy, auditory training, communication strategies.
Table: Causes of Bilateral vs. Unilateral SNHL (CBME Focus)
| Causes of Bilateral SNHL | Causes of Unilateral SNHL |
|---|---|
| Presbycusis | Chronic Suppurative Otitis Media (CSOM) - if labyrinth involved |
| Noise-induced hearing loss | Mumps (can be unilateral SNHL) |
| Ototoxic drugs | Herpes Zoster Oticus |
| Systemic disorders (e.g., diabetes, autoimmune) | Acoustic Neuroma (Vestibular Schwannoma) |
| Familial progressive SNHL | Sudden Sensorineural Hearing Loss (often unilateral) |
| Congenital SNHL (syndromic/non-syndromic) | Meniere's Disease (initially unilateral, can become bilateral) |
| Bilateral temporal bone fractures | Unilateral temporal bone fracture |
Table: Congenital and Acquired causes of conductive hearing loss

Mixed Hearing Loss.
Mixed hearing loss is diagnosed when both conductive and sensorineural components coexist in the same ear. This implies a problem in sound conduction to the inner ear and a problem within the inner ear or auditory nerve itself.
Identification on Audiometry: Mixed hearing loss is characterised by:
- The presence of an air-bone gap (ABG > 15-20 dB), indicating a conductive component.
- Impaired bone conduction thresholds (BC > 20 dB HL), indicating a sensorineural component.
- Therefore, in mixed hearing loss, both AC and BC thresholds are elevated, but AC thresholds are significantly poorer than BC thresholds, creating the ABG.
Common Causes of Mixed Hearing Loss: This type often arises from conditions that can affect both conductive and sensorineural mechanisms.
- Otosclerosis with Cochlear Involvement: While primarily conductive (stapes fixation), prolonged otosclerosis can sometimes lead to secondary cochlear damage (cochlear otosclerosis).
- Chronic Suppurative Otitis Media (CSOM) with Labyrinthine Fistula/Involvement: Chronic middle ear infection can erode ossicles (conductive component) and, if it extends to the labyrinth (inner ear), cause sensorineural damage.
- Temporal Bone Fracture: Can cause ossicular disruption (conductive) and inner ear/nerve damage (sensorineural).
- Head Trauma: Similar to temporal bone fractures.
- Ageing with Earwax Impaction: Presbycusis (SNHL) coexisting with cerumen impaction (CHL).
Management of Mixed Hearing Loss: Management involves addressing both components where possible.
- Prioritise Conductive Component: Often, addressing the conductive component first (e.g., surgery for CSOM, stapedectomy for otosclerosis) can significantly improve hearing.
- Address Sensorineural Component: Hearing aids or cochlear implants may be necessary if the SNHL component is significant.
Central Hearing Loss / Auditory Processing Disorder (APD).
Individuals with central hearing loss, more accurately termed Auditory Processing Disorder (APD), typically have normal pure-tone hearing thresholds and pass other standard hearing tests. However, they exhibit difficulties in processing distorted or unclear speech, particularly in challenging listening environments such as the presence of background noise (e.g., in social settings or classrooms). Consequently, these individuals struggle to follow verbal instructions, understand rapid speech, or distinguish similar-sounding words. These challenges are attributed to deficits in the processing of auditory information within the higher auditory pathways of the brain, rather than problems with the peripheral auditory system (ear or auditory nerve).
Key Features:
- Normal pure tone audiogram.
- Difficulty understanding speech, especially in noise.
- Difficulty localising sound.
- Problems with auditory memory or sequencing.
- Can hear, but cannot understand.
Diagnosis:
- Specialised audiometric tests are designed to assess central auditory function (e.g., speech-in-noise tests, dichotic listening tests).
Management:
- Auditory training.
- Environmental modifications (e.g., reducing background noise).
- Compensatory strategies.
- Frequency modulation (FM) systems in educational settings.
Non-Organic / Functional Hearing Loss.
Functional hearing loss, also known as non-organic hearing loss, describes a situation where an individual exaggerates or feigns hearing impairment without a corresponding organic pathology that fully explains the observed hearing thresholds. Various terms have describe this phenomenon, including pseudo-hyperacusis, malingering (conscious feigning for gain), and factitious hearing loss (unconscious feigning). However, it is crucial to recognise that in many instances, individuals may indeed possess an underlying organic hearing loss that is then intentionally or unintentionally exaggerated. In other cases, particularly following trauma or for compensation claims, the individual may entirely feign hearing loss. Given the potential presence of an organic component, functional hearing loss is best understood as an exaggerated hearing loss or a functional overlay to an existing organic loss.
Clinical Presentations: Patients may present in any of the following three scenarios:
- Total hearing loss in both ears
- Total hearing loss in one ear
- Exaggerated hearing loss in one or both ears
Diagnosis:
1. High Index of Suspicion: Watch for exaggerated behaviours, such as frequently requesting repetition of questions, cupping the ear excessively and inconsistent complaints with clinical findings. These actions raise red flags for functional overlay.
2. Inconsistent Audiometry Results: In pure tone and speech audiometry, normal variation on repeat testing is ±5 dB. A variation greater than 15 dB strongly suggests NOHL. Audiometric Zig-zag” or “Saucer” Pattern is sometimes seen on PTA.
3. Absence of Shadow Curve in Bone Conduction. In unilateral deafness without masking, a shadow curve should appear on bone conduction due to transcranial sound transmission. If this shadow curve is absent, despite claims of total unilateral hearing loss, it is diagnostic of functional hearing loss.
4. Discrepancy Between PTA and SRT. Normally, the Pure Tone Average (PTA) at 500, 1000, and 2000 Hz closely matches the Speech Reception Threshold (SRT) (within 10 dB). If SRT is better than PTA by more than 10 dB, this suggests exaggeration or malingering.
5. Acoustic Reflex Threshold. Normally, the stapedial (acoustic) reflex is present at 70–100 dB SL. If a patient claims total deafness but the reflex is still elicited, it clearly indicates functional hearing and NOHL.
6. Electric Response Audiometry (ERA). ERA evaluates auditory evoked potentials, bypassing the patient’s conscious effort. It can accurately estimate the hearing threshold within 5–10 dB, even in cases of suspected malingering. Highly reliable in children, non-cooperative patients, and suspected NOHL cases.
7. Stenger Test (Diagnostic for Unilateral Malingering).
Principle:
When the same tone is played in both ears with different intensities, the patient will only perceive the louder tone.
Procedure: Always blindfold the patient during the test to avoid bias.
- Take two identical tuning forks or use a two-channel audiometer.
- Strike the forks and hold both 25 cm away from each ear.
- The patient will report hearing in the normal ear.
- Now, bring the tuning fork closer (8 cm) to the suspected ear, keeping the normal side unchanged.
- A malingering patient will now claim to hear nothing, even though the louder stimulus should be heard in the “deaf” ear.
- A truly deaf patient will continue hearing in the normal ear.
Interpretation:
- Positive Stenger (patient says he hears nothing): Indicates malingering.
- Negative Stenger (hears in one ear): Likely genuine loss.
Management of non-organic hearing loss:
- Requires a sensitive, non-confrontational approach.
- Counseling and psychological support are often beneficial.
- Reassurance that hearing is better than reported.
———— End of the chapter ————
High-Yield Points for NEET PG and University Exams
- WHO Classification: Based on pure tone average (500, 1000, 2000 Hz) in the better ear.
- Conductive Hearing Loss (CHL): Problem in sound transmission (external ear to stapediovestibular joint).
- Rinne Test: Negative (BC > AC).
- Weber Test: Lateralizes to the affected (poorer) ear.
- BC: Normal (≤ 20 dB HL).
- Low Frequencies are more affected.
- Speech Discrimination: Good.
- Max CHL: Around 60 dB HL.
- Causes: Cerumen, TM perforation, OME, Otosclerosis, Ossicular discontinuity.
- Sensorineural Hearing Loss (SNHL): Problem in cochlea or 8th nerve/central pathways.
- Rinne Test: Positive (AC > BC), but both are reduced.
- Weber Test: Lateralizes to the unaffected (better) ear.
- BC: Reduced.
- High Frequencies are usually more affected.
- Speech Discrimination: Poor.
- Recruitment: Common in cochlear SNHL.
- Tympanometry: Normal (Type A).
- Causes: Presbycusis, NIHL (4KHz notch), Ototoxic drugs, SSNHL, Meniere’s, Acoustic Neuroma (unilateral SNHL, requires MRI), Congenital syndromes (Waardenburg, Usher, Pendred).
- Mixed Hearing Loss: Both conductive (ABG) and sensorineural (elevated BC) components. Common in Otosclerosis with cochlear involvement, CSOM with labyrinthine involvement, and Temporal bone fracture.
- Non-Organic Hearing Loss: Inconsistent audiometric results; objective tests (ABR, OAE) may be normal.
- Central Hearing Loss (APD): Normal PTA, but difficulty processing speech, especially in noise.
Multiple Choice Questions (MCQs)
Instructions: Choose the single best answer for each question.
- A 55-year-old male presents with difficulty understanding speech in noisy environments, although his pure tone audiogram shows normal hearing thresholds. Which type of hearing loss is most likely present? a) Conductive hearing loss b) Sensorineural hearing loss c) Mixed hearing loss d) Central hearing loss e) Non-organic hearing loss
- A patient undergoes a Rinne test, and the tuning fork is heard louder by bone conduction than by air conduction in the right ear. The Weber test lateralizes to the right ear. What is the most likely diagnosis? a) Right sensorineural hearing loss b) Left sensorineural hearing loss c) Right conductive hearing loss d) Left conductive hearing loss e) Bilateral mixed hearing loss
- Which of the following conditions is most likely to cause a typical 4000 Hz notch on a pure tone audiogram? a) Otosclerosis b) Presbycusis c) Noise-induced hearing loss d) Meniere’s disease e) Chronic otitis media with effusion
- A 30-year-old female presents with fluctuating hearing loss, episodic vertigo, tinnitus, and aural fullness. Which of the following conditions is characterised by this constellation of symptoms? a) Acoustic neuroma b) Otosclerosis c) Sudden sensorineural hearing loss d) Meniere’s disease e) Presbycusis
- In pure conductive hearing loss, the bone conduction (BC) thresholds on pure tone audiometry are typically: a) Greater than 60 dB HL b) Equal to air conduction (AC) thresholds c) Significantly elevated (poor hearing) d) Normal (equal to or better than 20 dB HL) e) Absent
- Which of the following is a characteristic feature of sensorineural hearing loss but is usually absent in pure conductive hearing loss? a) Negative Rinne test b) Weber lateralizes to the poorer ear c) Good speech discrimination d) Recruitment phenomenon e) Max hearing loss of 60 dB
- A child presents with a white forelock, widely spaced eyes, and bilateral profound hearing loss. This presentation is most consistent with which syndrome? a) Usher Syndrome b) Pendred Syndrome c) Alport Syndrome d) Waardenburg Syndrome e) Jervell and Lange-Nielsen Syndrome
- An elderly patient with known diabetes mellitus is prescribed a high dose of an antibiotic for a severe infection. Following treatment, they report worsening hearing. Which class of antibiotics is most notorious for causing ototoxicity? a) Penicillins b) Cephalosporins c) Macrolides d) Aminoglycosides e) Fluoroquinolones
- An audiogram shows elevated air conduction thresholds with an air-bone gap of 20 dB across most frequencies, and elevated bone conduction thresholds (greater than 20 dB HL). This pattern indicates: a) Pure conductive hearing loss b) Pure sensorineural hearing loss c) Mixed hearing loss d) Non-organic hearing loss e) Central hearing loss
- The management of severe-to-profound sensorineural hearing loss in children who receive inadequate benefit from hearing aids often involves: a) Myringotomy and grommet insertion b) Stapedectomy c) Cochlear implantation d) Ossiculoplasty e) Tympanoplasty
MCQ Answers and Explanations:
- d) Central hearing loss
- Explanation: Normal pure tone thresholds with difficulty processing speech, especially in noise, are classic symptoms of central hearing loss or Auditory Processing Disorder (APD).
- c) Right Conductive hearing loss
- Explanation: A negative Rinne (BC > AC) indicates a conductive component. Weber lateralizing to the poorer ear (right in this case) confirms a conductive loss in that ear.
- c) Noise-induced hearing loss
- Explanation: Noise-induced hearing loss characteristically presents with a “notch” at 4000 Hz (or sometimes 3000-6000 Hz) due to specific damage to the hair cells in that frequency region of the cochlea.
- d) Meniere’s disease
- Explanation: The classic triad of fluctuating SNHL, episodic vertigo, and tinnitus with aural fullness is diagnostic of Meniere’s disease.
- d) Normal (equal to or better than 20 dB HL)
- Explanation: In pure conductive hearing loss, the inner ear and auditory nerve function normally, so bone conduction (which bypasses the conductive mechanism) will be within normal limits.
- d) Recruitment phenomenon
- Explanation: Recruitment is an abnormal growth in loudness perception, a characteristic feature of cochlear (sensory) SNHL. Conductive hearing loss typically does not exhibit recruitment.
- d) Waardenburg Syndrome
- Explanation: Waardenburg Syndrome is characterised by pigmentation abnormalities (e.g., white forelock, heterochromia iridis) and sensorineural hearing loss.
- d) Aminoglycosides
- Explanation: Aminoglycoside antibiotics (e.g., gentamicin, amikacin, streptomycin) are well-known for their ototoxic effects, causing irreversible sensorineural hearing loss, particularly affecting high frequencies and vestibular function.
- c) Mixed hearing loss
- Explanation: An air-bone gap (AC > BC) indicates a conductive component, while elevated bone conduction thresholds (BC > 20 dB HL) indicate a sensorineural component. The presence of both defines mixed hearing loss.
- c) Cochlear implantation
- Explanation: For severe-to-profound SNHL where conventional hearing aids are insufficient, cochlear implants are the gold standard to provide auditory input by directly stimulating the auditory nerve.
Clinical-Based Questions (CBQs)
Instructions: Apply your knowledge of hearing loss types to the following patient scenarios.
- Scenario: A 6-year-old child is brought to the ENT clinic by his parents, who report that he frequently asks for repetition, struggles to hear in school, and has had recurrent ear infections. On otoscopy, bilateral dull tympanic membranes with decreased mobility are noted. Tympanometry shows bilateral Type B curves.
- a) What type of hearing loss is most likely present?
- Answer: Conductive hearing loss.
- b) What is the most probable diagnosis for the underlying cause?
- Answer: Otitis Media with Effusion (OME), also known as “glue ear.”
- c) Briefly outline the initial management strategy for this child.
- Answer: Initial management often involves watchful waiting (OME can resolve spontaneously), considering decongestants/antihistamines (though evidence is limited for efficacy), and if persistent with significant hearing loss affecting development, myringotomy with grommet insertion to drain fluid and equalise middle ear pressure.
- a) What type of hearing loss is most likely present?
- Scenario: A 70-year-old retired factory worker complains of progressive difficulty hearing, especially conversations in crowded places like restaurants. His wife often says he turns the TV volume too high. He denies ear pain or discharge. Pure tone audiometry reveals bilateral, symmetrical high-frequency sensorineural hearing loss.
- a) What is the most likely diagnosis for his hearing loss?
- Answer: Presbycusis (age-related hearing loss), likely exacerbated by noise-induced hearing loss from his occupational history.
- b) Explain why he struggles in noisy environments despite perhaps “hearing” sounds.
- Answer: High-frequency SNHL impairs speech discrimination, particularly consonant sounds (which carry much of speech clarity). In noisy environments, the brain struggles to filter out background noise and focus on the degraded speech signal, making understanding very challenging. This is a classic symptom of SNHL.
- c) What are the primary rehabilitation options for this patient?
- Answer: The primary rehabilitation option is hearing aids, specifically programmed to compensate for his high-frequency loss. Aural rehabilitation (auditory training, communication strategies) can also be very beneficial.
- a) What is the most likely diagnosis for his hearing loss?
- Scenario: A 40-year-old male suddenly experienced severe dizziness, ringing in his left ear, and a feeling of fullness in the ear this morning. He also reports a significant decrease in hearing on that side. There’s no history of head trauma or ear infection.
- a) What is the most probable diagnosis given this constellation of acute symptoms?
- Answer: Sudden Sensorineural Hearing Loss (SSNHL) associated with Meniere’s disease (given the vertigo, tinnitus, fullness, and fluctuating nature implied). Or, less likely but still a consideration, isolated SSNHL (idiopathic).
- b) What urgent diagnostic test is crucial to rule out a potentially serious retrocochlear pathology?
- Answer: An urgent MRI of the brain with contrast, focusing on the internal auditory canals (IACs), is crucial to rule out an acoustic neuroma (vestibular schwannoma) or other retrocochlear lesions, especially given the unilateral SNHL and vestibular symptoms.
- c) What is the immediate medical management consideration for this patient if SSNHL is confirmed?
- Answer: High-dose oral corticosteroids (e.g., prednisone taper) should be initiated as soon as possible, ideally within 72 hours of onset, as this can improve prognosis for hearing recovery. Intratympanic steroid injections are also an option.
- a) What is the most probable diagnosis given this constellation of acute symptoms?
- Scenario: A 10-year-old boy presents with a history of inconsistent responses to sound. His parents report that he seems to hear but not others, and sometimes gives exaggerated responses. Pure tone audiometry shows varying thresholds on repeat testing, and the pattern does not fit a typical organic hearing loss. Objective tests like OAEs are normal.
- a) What type of hearing loss should be suspected?
- Answer: Non-organic (Functional) hearing loss.
- b) Why are consistent test results important in diagnosing hearing loss, and what do inconsistent results suggest?
- Answer: Consistent test results are crucial because they reflect a stable and predictable auditory response from a true organic pathology. Inconsistent results suggest a non-organic component, where the patient’s responses are not genuinely indicative of their hearing ability, often implying exaggeration or feigning.
- c) How should a clinician approach the management of this patient?
- Answer: The clinician should approach this with a non-confrontational, empathetic, and supportive manner. The management involves carefully explaining the test results to the parents and child, providing reassurance about their hearing ability, and considering counselling or psychological support if underlying psychosocial factors are suspected. The focus is on guiding them toward more consistent and appropriate responses.
- a) What type of hearing loss should be suspected?
Frequently Asked Questions (FAQs) in Viva
- Q: What is the difference between conductive and sensorineural hearing loss?
- A: Conductive hearing loss results from problems in sound transmission to the inner ear, while sensorineural hearing loss arises from damage to the inner ear (cochlea) or the auditory nerve.
- Q: What is the significance of a negative Rinne test?
- A: A negative Rinne test (bone conduction heard louder than air conduction) is a hallmark sign of conductive hearing loss.
- Q: How does the Weber test help differentiate hearing loss types?
- A: In conductive hearing loss, the Weber test lateralizes (sound heard louder) to the poorer ear; in sensorineural hearing loss, it lateralizes to the better ear.
- Q: What does an air-bone gap on an audiogram indicate?
- A: An air-bone gap (AC thresholds significantly worse than BC thresholds) indicates the presence of a conductive component to the hearing loss.
- Q: Can hearing loss be cured?
- A: Conductive hearing loss is often medically or surgically treatable, but sensorineural hearing loss is typically permanent and managed with hearing aids or cochlear implants, though some acute cases (like SSNHL) may respond to steroids.
- Q: What are some common causes of sensorineural hearing loss in adults?
- A: Common causes include age-related hearing loss (presbycusis), noise exposure (noise-induced hearing loss), ototoxic medications, and Meniere’s disease.
- Q: Why is it important to investigate unilateral sensorineural hearing loss?
- A: Unilateral sensorineural hearing loss, especially if progressive or associated with other symptoms, must be thoroughly investigated with an MRI to rule out a retrocochlear lesion like an acoustic neuroma.
Practical Tips for Viva and Clinical Exam Scenarios
Presenting Hearing Loss in Viva:
- Define Hearing Loss: Start with a clear, concise definition and mention the WHO classification briefly.
- Categorisation: Immediately list the five types.
- Clinical Tools: Emphasise the role of Tuning Fork Tests (Rinne, Weber) and Pure Tone Audiometry (PTA) as foundational diagnostic tools.
- Systematic Approach per Type: For each type:
- Definition/Mechanism: How does it occur?
- Clinical Characteristics: How does the patient present (e.g., speech discrimination, difficulty in noise)?
- Tuning Fork Findings: Crucial for viva.
- Audiometric Profile (PTA): What does the audiogram look like (ABG, BC thresholds, frequency affected)?
- Common Causes: List the most frequent etiologies.
- Management: Briefly outline key medical/surgical options and rehabilitation.
- Focus on Differentiation: Be prepared to compare and contrast CHL vs. SNHL repeatedly.
- Be Ready to Draw: Practice drawing basic audiograms for each type of hearing loss.
Common Examiner Questions (Viva):
- “Differentiate between conductive and sensorineural hearing loss using Rinne and Weber tests.”
- “Describe the audiometric findings in mixed hearing loss.”
- “Enumerate the causes of conductive hearing loss.”
- “What is recruitment? In which type of hearing loss is it seen?”
- “What are the red flags for unilateral SNHL?” (Acoustic neuroma!)
- “Name five syndromes associated with congenital SNHL.”
- “How do you manage a patient with profound bilateral SNHL who doesn’t benefit from hearing aids?” (Cochlear implant).
- “Explain the 4000 Hz notch.”
- “What is functional hearing loss, and how do you diagnose it?”
Clinical Exam Scenarios (Applying Knowledge):
- Patient Presentation: “A patient comes to you with X symptoms. What initial tests would you do, and what type of hearing loss are you suspecting?” (E.g., “Child with speech delay and recurrent cold -> suspect OME -> otoscopy, tympanometry”).
- Audiogram Interpretation: “Here is an audiogram. Interpret it and give me the type and degree of hearing loss.” (Practice reading audiograms!)
- Management Plan: “How would you manage this patient with [specific type] hearing loss?” (Think medical, surgical, amplification, rehabilitation).
- Counselling: “How would you counsel a patient with presbycusis about their hearing loss?” (Emphasise hearing aids, communication strategies, managing expectations).
———— End ————
Download full PDF Link:
Types of Hearing Loss Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page:https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Juvenile Angiofibroma. https://www.entlecture.com/juvenile-angiofibroma/
- Please read. Tumours of Hypopharynx . https://www.entlecture.com/tumours-of-the-hypopharynx/
- Please read. Anatomy of Oesophagus. https://www.entlecture.com/anatomy-of-oesophagus/
Keywords: Understand the different types of hearing loss – conductive, sensorineural, mixed, non-organic, and central. This detailed guide, optimised for MBBS and ENT PG students, covers causes, characteristics, diagnosis, and management, aligning with the CBME curriculum for university exams, viva, practicals, and NEET PG. Types of Hearing Loss, Conductive Hearing Loss, Sensorineural Hearing Loss, Mixed Hearing Loss, Functional Hearing Loss, Central Hearing Loss, Auditory Processing Disorder, WHO Hearing Loss Classification, Pure Tone Audiometry Interpretation, Rinne Test Weber Test, Air-Bone Gap Audiogram, Causes of Hearing Loss, Management of Hearing Loss, Otosclerosis Hearing Loss, Noise-Induced Hearing Loss, Presbycusis Symptoms, Sudden Sensorineural Hearing Loss, Meniere’s Disease Symptoms, Acoustic Neuroma Hearing Loss, Congenital SNHL Syndromes, Ototoxic Drugs Hearing Loss, ENT Hearing Loss MBBS, ENT PG Hearing Loss, NEET PG ENT Topics, Hearing Loss Viva Questions, Clinical Scenarios Hearing Loss, Hearing Loss Treatment Options, Hearing Aids Cochlear Implants, CBME ENT Curriculum Hearing Loss, Causes of conductive hearing loss, conductive hearing loss treatment options, diagnosing conductive hearing loss, conductive vs sensorineural hearing loss differences, sensorineural hearing loss symptoms, inner ear hearing loss causes, sensorineural hearing loss management, reversible sensorineural hearing loss, what is mixed hearing loss, causes of mixed hearing loss, treating mixed hearing loss, functional hearing loss definition, diagnosing non-organic hearing loss, management of functional hearing loss, central auditory processing disorder causes, central auditory processing disorder symptoms, auditory processing disorder diagnosis, central hearing loss treatment options, different types of hearing loss explained for students, audiological classification of hearing loss

Thanks for this 🙏 discussion..
I want to ask how can we know Central form neural by Audiometry
Easy to understand. Amazing book.