Basic Clinical & Tuning Fork Tests for Hearing Assessment
I. Clinical Hearing Tests
Hearing assessments are crucial for diagnosing auditory function and identifying potential hearing impairments. Several clinical tests are employed to evaluate hearing thresholds and sound localisation. The Finger Friction Test, the Watch Test, and the Free Field Voice/Speech Test are among these tests.
i. Finger Friction Test
The Finger Friction Test is a simple, qualitative screening tool to assess gross hearing thresholds and sound localisation.
- Procedure: The examiner gently snaps their thumb and middle finger together, producing a soft clicking sound. They present this sound near the patient’s ear. The patient closes their eyes and indicates when they hear the sound.
- Interpretation: This test subjectively evaluates a patient’s ability to perceive faint, high-frequency sounds.
ii. Watch Test
Historically, the Watch Test was a common method used to estimate auditory sensitivity before audiometers became widely available.
- Procedure: The examiner brings a ticking watch close to the patient’s ear, gradually moving it closer or further away. The distance at which the patient can reliably hear the ticking sound is noted.
- Interpretation: A shorter distance suggests a hearing impairment, whereas a longer distance indicates better auditory sensitivity.
iii. Free Field Voice/Speech Test
The Free Field Voice/Speech Test is a structured, yet simple, assessment conducted in a clinical environment. It evaluates hearing in each ear separately.
- Procedure:
- Environment: Conduct this test in a quiet room to minimise ambient noise interference.
- Patient Positioning: The patient stands 6 meters (20 feet) away from the examiner. The examiner faces the test ear, while the patient keeps their eyes closed to prevent visual cues from lip-reading.
- Masking: An assistant or the examiner masks the non-test ear to prevent sound interference. They achieve this by rubbing an index finger on the patient’s tragus or by using a Barany noise box, which delivers a masking noise.
- Testing:
- The examiner speaks spondee words (e.g., “iceberg,” “sunlight,” “bathroom”) or alphanumeric combinations (e.g., “Y3G,” “6BZ”) at a conversational voice level. The examiner gradually moves closer to the patient until the patient can correctly hear the words. The distance is then recorded.
- Subsequently, the examiner whispers spondee words, and the distance at which the whispered voice is heard is also measured.
- Interpretation:
- If a patient can hear a conversational voice from 6 meters, their hearing is likely within normal limits.
- A patient with a hearing loss greater than 30 dB HL typically cannot hear a whispered voice from a distance of 2 feet (approximately 60 cm) from the test ear.
- The test’s reported sensitivity is around 95%, with a 10% false-positive rate. Therefore, if a patient can hear a whispered voice from 2 feet away, it suggests their pure tone threshold is better than 30 dB HL.
- Disadvantages: Despite its utility, the Free Field Voice/Speech Test has limitations. The standardisation of the intensity and pitch of the voice used during testing is often questioned, and external ambient noise can interfere with the accuracy of results. These factors can affect the reliability of the test outcomes, highlighting the need for careful consideration during clinical assessments.
II. Tuning Fork Tests
Tuning fork tests are quick, inexpensive, and highly valuable clinical tools for differentiating between conductive and sensorineural hearing loss. They are indispensable for ENT residents and MBBS students in the outpatient setting.
Selection of Tuning Fork. The selection of an appropriate tuning fork is crucial.
- Frequencies: Tuning forks are available in various frequencies, including 128 Hz, 256 Hz, 512 Hz, 1024 Hz, 2048 Hz, and 4096 Hz.
- Clinical Preference: In clinical practice, a tuning fork of 512 Hz is preferred due to its optimal decay time and minimal overtones, making it ideal for accurate testing.
- Frequency-Specific Considerations:
- Lower frequency forks (e.g., 128 Hz) tend to produce a tactile sensation of bone vibration, which patients might confuse with sound, thus leading to unreliable results.
- Higher frequency forks (e.g., 4096 Hz) have shorter decay times, making them less practical for prolonged testing and prone to rapid sound dissipation, which can also affect test outcomes.
Setting the tuning fork into vibration:
- Technique: The practitioner should hold the tuning fork by its stem. Gently strike one of its prongs against a firm yet yielding surface, such as the examiner’s elbow or the heel of their hand.
- Optimal Strike Point: For optimal results, strike the prong approximately one-third of its length from the free end. This technique minimises undesirable overtones and produces a purer tone.
Pre-requisites for tuning fork tests: Before conducting the tests, it is essential to explain the procedure to the patient, instructing them to raise a finger when they can no longer hear the sound. Additionally, the practitioner should stabilise the patient’s head to ensure accurate results.
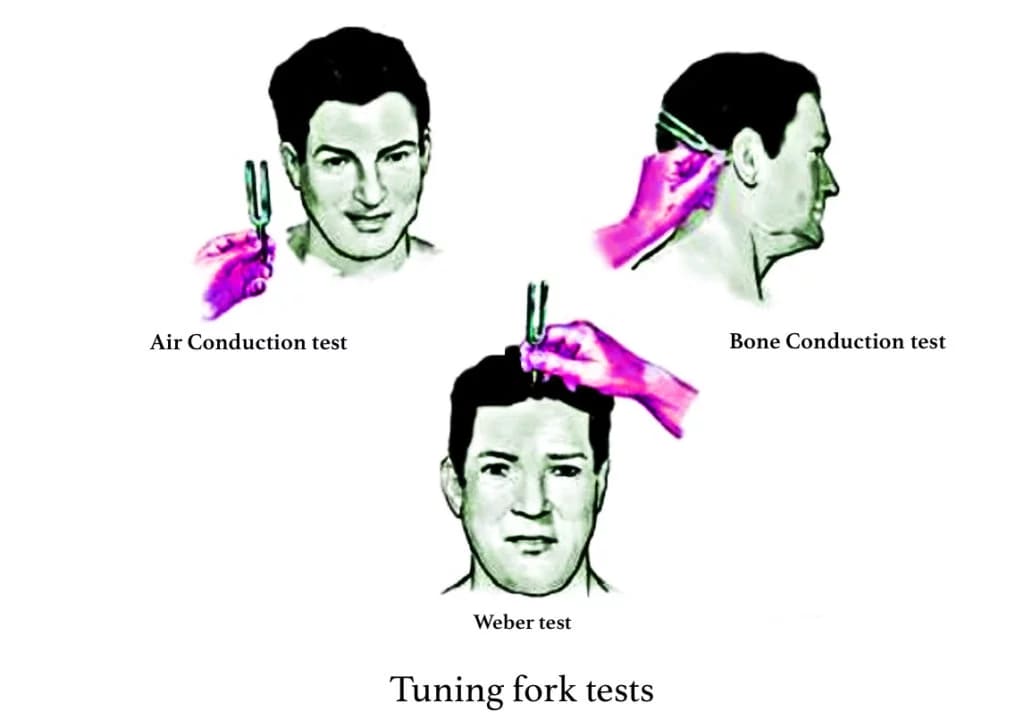
Testing Methods. The tuning fork tests primarily assess two types of conduction: air conduction (AC) and bone conduction (BC).
- Air Conduction (AC) Test: The vibrating tuning fork is placed vertically about 2 cm from the external auditory canal. Sound waves travel through the tympanic membrane, middle ear, and ossicles to the inner ear, allowing evaluation of both the conducting mechanism and cochlear function. Typically, sound heard through air conduction is louder and lasts longer than through bone conduction.
- Bone Conduction (BC) Test: The footplate of the vibrating tuning fork is placed on the mastoid bone. This method bypasses the outer and middle ear and stimulates the cochlea directly through vibrations transmitted via the skull bones, measuring cochlear function alone.
The clinically useful tuning fork tests include:
1. Rinne’s Test: In this test, the base of the vibrating tuning fork is placed on the mastoid bone. When the patient can no longer hear the sound, the fork is moved 2.5 cm in front of the external auditory canal. If the patient still hears the sound, it indicates that air conduction is better than the bone conduction.
- Interpretation:
-
- Positive Rinne: AC > BC, indicating normal hearing or sensorineural deafness.
- Negative Rinne: BC > AC, indicating conductive deafness.
- False Negative: In cases of severe unilateral sensorineural hearing loss, the patient may hear the sound on the mastoid but not in front of the ear. This can be confirmed with masking techniques and the Weber test.
The degree of air-bone gap can be assessed using tuning forks of 256, 512, and 1024 Hz, with specific interpretations for each frequency.
- A Rinne test equal or negative for 256 Hz but positive for 512 Hz indicates an air-bone gap of 20–30 dB.
- A Rinne test negative for 256 and 512 Hz but positive for 1024 Hz indicates an air-bone gap of 30–45 dB.
- A Rinne negative for all three tuning forks of 256, 512 and 1024 Hz indicates an air-bone gap of 45–60 dB.
Remember that a negative Rinne for 256, 512 and 1024 Hz indicates a minimum AB gap of 15, 30, and 45 dB, respectively.
2. Weber’s Test: This test involves placing the vibrating 512 Hz tuning fork in the middle of the forehead/vertex/ central incisors or mandibular symphysis, from where it will be conducted directly to the cochlea, bypassing the outer and middle ear. The patient is asked to identify which ear they hear the sound better or louder.
- Interpretation:
- Normal Hearing: The sound is heard equally in both ears and does not lateralize (patient says, “It’s in the middle”).
- Conductive Hearing Loss: The sound lateralizes to the affected (poorer) ear. This happens because:
- Occlusion Effect: In a conductive loss, the affected middle ear acts as a barrier, preventing ambient noise from entering the inner ear via the normal air conduction pathway. This makes the bone-conducted sound from the tuning fork relatively louder in the affected ear (autophony).
- Mass Effect: A fixed or stiff ossicular chain (e.g., in otosclerosis) or middle ear fluid may enhance bone conduction by impeding sound energy dissipation.
- Sensorineural Hearing Loss (SNHL): The sound lateralizes to the unaffected (better) ear. In SNHL, the damaged cochlea in the affected ear cannot efficiently process sound, regardless of whether it arrives via air or bone. Therefore, the bone-conducted sound from the tuning fork is better perceived by the healthy cochlea of the unaffected ear.
3. Absolute Bone Conduction Test: This test compares the bone conduction of the patient to that of the examiner, assuming the examiner has normal hearing. Occlude the patient’s ear canal (test ear) by firmly pressing the tragus over the meatus (this eliminates air conduction, focusing purely on bone conduction). Place the vibrating 512 Hz tuning fork on the patient’s mastoid bone. When the patient reports no longer hearing the sound, immediately transfer the still-vibrating tuning fork to the examiner’s own mastoid (with their ear also occluded). The examiner then notes if they can still hear the sound.
- Interpretation:
-
- Normal or conductive deafness: Both the patient and the examiner hear the sound for the same duration.
- Sensorineural deafness: The examiner continues to hear the sound longer than the patient. This indicates that the patient’s bone conduction is reduced compared to a normal ear.
4. Schwabach Test: The procedure is similar to the absolute bone conduction test, but without occluding the ear canal. It also compares the patient’s bone conduction to the examiner’s.
- Interpretation:
- Normal Hearing: Patient and examiner hear for similar durations.
- Conductive Hearing Loss: Patient hears the sound for a longer duration than the examiner (lengthened Schwabach), due to the occlusion effect and lack of sound dissipation from the middle ear.
- Sensorineural Hearing Loss: Patient hears the sound for a shorter duration than the examiner (shortened Schwabach), due to inner ear damage.
5. Bing Test: This test assesses the presence of the occlusion effect of the ear canal. Place the vibrating 512 Hz tuning fork on the patient’s mastoid process while the examiner alternately closes and opens the ear canal by pressing on the tragus inwards. The patient is asked if the sound changes (gets louder or softer).
- Interpretation:
- Normal Hearing or Sensorineural Hearing Loss: The sound heard by bone conduction increases (gets louder) when the ear canal is blocked (Bing positive). This is due to the occlusion effect, where blocking the ear canal prevents sound energy from escaping, thus enhancing bone-conducted sound perception.
- Conductive Hearing Loss: There is no significant change in sound perception when the ear canal is blocked (Bing negative). This is because the conductive pathology (e.g., fixed or disconnected ossicular chain, middle ear fluid) already prevents sound dissipation, so further blocking the ear canal offers no additional “occlusion.”
6. Gelle’s Test: This test assesses the functional status of the ossicular chain by altering air pressure in the external auditory canal. Normally, when air pressure is increased in the ear canal by Siegel’s speculum, it pushes the tympanic membrane and ossicles inwards, raises the intralabyrinthine pressure and causes immobility of the basilar membrane and decreased hearing, but no change in hearing is observed when the ossicular chain is fixed or disconnected. Place the vibrating 512 Hz tuning fork on the patient’s mastoid process while altering air pressure in the ear canal by pneumatic otoscope or impedance probe. Ask the patient if the loudness of the sound changes.
- Interpretation:
- Normal Subjects: With increased air pressure (pushing the tympanic membrane inward), the loudness increases. This happens because the ossicular chain is stiffened by the pressure change, reducing the transmission of bone-conducted sound.
- Conductive Hearing Loss (Ossicular Fixation/Discontinuity): Patients show no change in sound perception. If the ossicular chain is already fixed (e.g., otosclerosis) or discontinuous, changes in external ear canal pressure will not affect its mobility or the transmission of sound to the inner ear.
Table: TUNING FORK TESTS AND THEIR INTERPRETATION
| Test | Normal | Conductive deafness | SN deafness |
| Rinne | AC > BC (Rinne positive) | BC > AC (Rinne negative) | AC>BC |
| Weber | Not lateralized | Lateralizes to the poorer ear | Lateralizes to the better ear |
| ABC | Same as the examiner’s | Same as the examiner’s | Reduced (patient hears less) |
| Schwabach | Equal | Lengthened (patient hears longer) | Shortened (patient hears shorter) |
| Bing | Positive (sound increases with occlusion) | Negative (no change with occlusion) | Positive (sound increases with occlusion) |
| Gelle’s | Sound increases with a pressure change | No change with pressure change | Sound increases with a pressure change |
Special Tuning Fork Tests for Malingering and Non-Organic Deafness
1. Stenger’s Test. Stenger’s test is based on the principle that when two identical sounds are presented to a person with one healthy ear and one deaf ear, the individual will only perceive the sound in the ear that is closer to the sound source.
Procedure: In this test, the patient is blindfolded. The examiner uses two similar tuning forks, typically of 512 Hz, struck to moderate intensity and held approximately 25 cm from each ear. If the patient is malingering, he will only hear the sound in the normal ear. The tuning fork on the deaf side is then moved closer by 3 inches. A malingerer will not perceive the sound at all, confirming the suspicion of non-organic deafness.
2. Chimani Moos Test. The Chimani Moos test is a modification of the Weber test, designed to identify non-organic hearing loss.
Procedure: When a vibrating tuning fork is placed on the forehead, a malingerer will often report hearing the sound in their better ear, which simulates sensorineural deafness. If the ear canal of the better ear is occluded, a genuinely deaf patient will still hear the sound in the occluded ear, while a malingerer will claim they cannot hear it.
3. Teal Test. The Teal test specifically evaluates the validity of claims where patients assert they can only hear through bone conduction (a pattern highly suspicious of non-organic hearing loss, as pure bone conduction hearing without any air conduction is rare).
Procedure: This test involves presenting a vibrating tuning fork to the mastoid and then alternately to the external ear canal while the patient’s ear is occluded and unoccluded. A malingerer will typically maintain that they only hear the sound via bone conduction, even when conditions are optimal for air conduction.
Voice Tests for Malingering and Non-Organic Deafness
1. Erhard’s Test. Erhard’s test is utilised to detect total unilateral hearing loss. In this procedure, the ear canal of the normal ear is occluded, which reduces speech perception by 30 dB or less. The suspected malingerer is instructed to close their eyes and repeat words they hear. The examiner occludes the normal ear by pressing on the tragus and then speaks words into the suspected ear. If the patient fails to repeat the words, it suggests malingering, as even with the head shadow effect, the other ear should still be able to hear.
2. Lombard’s Test. Lombard’s test is grounded in the observation that individuals typically raise their voice when speaking in noisy environments. During this test, the patient is asked to read prose aloud. Noise is then introduced to the good ear. If there is an organic loss in the suspected ear, the patient will raise their voice. Conversely, if the hearing loss is feigned, the patient will show no change in speech volume, indicating normal monitoring of their voice.
———— End of the chapter ————
High-Yield Points for Quick Revision
These are critical concepts often tested in NEET PG MCQs and university exams. Ensure you understand them thoroughly.
- 512 Hz tuning fork is preferred due to optimal decay time and minimal overtones.
- Rinne’s Test: AC > BC is positive (Normal/SNHL), BC > AC is negative (Conductive). Always remember the false negative Rinne in severe unilateral SNHL.
- Weber’s Test: Lateralizes to the poorer ear in conductive loss (due to occlusion effect and mass effect). Lateralizes to the better ear in sensorineural loss.
- Occlusion Effect is when blocking the ear canal makes bone-conducted sound louder. It’s present in normal hearing and SNHL, but absent in conductive loss.
- Bing Test assesses the occlusion effect: Positive (sound increases with occlusion) in normal/SNHL; Negative (no change) in conductive loss.
- Gelle’s Test assesses ossicular chain mobility. Sound decreases with pressure changes in normal ears, but no change in conductive loss (fixed ossicular chain).
- Stenger’s Principle is the basis for detecting malingering. The louder sound is perceived; a malingerer will deny hearing anything if the louder sound is in the “deaf” ear.
- Lombard Effect: Involuntary increase in voice volume in noise. Used to detect malingering by observing if voice volume changes when noise is introduced to the “good” ear.
NEET PG-style MCQs
Practice these questions to test your understanding and prepare for competitive exams.
- A patient presents with a history of recurrent ear discharge and reduced hearing in the right ear. Rinne’s test on the right ear is negative (BC > AC), and Weber’s test lateralizes to the right ear. Which of the following is the most likely diagnosis? A) Right sensorineural hearing loss B) Right conductive hearing loss C) Left sensorineural hearing loss D) Normal hearing
- Which frequency tuning fork is generally preferred for clinical hearing tests due to its optimal decay time and minimal overtones? A) 128 Hz B) 256 Hz C) 512 Hz D) 1024 Hz
- In the Free Field Voice/Speech Test, masking of the non-test ear is typically achieved by: A) Asking the patient to hum loudly B) Applying a deafening sound from a distant speaker C) Rubbing an index finger on the patient’s tragus or using a Barany noise box D) Placing cotton wool tightly in the non-test ear canal
- The Bing test is performed, and the patient reports no change in sound perception when the ear canal is occluded. This result is characteristic of: A) Normal hearing B) Sensorineural hearing loss C) Conductive hearing loss D) Malingering
- Which of the following is a disadvantage of the Free Field Voice/Speech Test? A) It is too expensive to perform. B) It requires highly specialized equipment. C) Standardization of voice intensity and ambient noise interference are common issues. D) It cannot be used to assess speech perception.
- A 25-year-old male is suspected of having non-organic hearing loss. During the Lombard’s Test, noise is introduced into his better ear, but there is no change in his speech volume while reading aloud. This finding suggests: A) Organic sensorineural hearing loss B) Organic conductive hearing loss C) Malingering or non-organic hearing loss D) Normal hearing
- In a positive Rinne’s test, which of the following relationships between air conduction (AC) and bone conduction (BC) is observed? A) AC = BC B) AC < BC C) AC > BC D) AC is not heard at all
- Which tuning fork test compares the patient’s bone conduction to the examiner’s, with the patient’s ear canal occluded? A) Rinne’s test B) Weber’s test C) Schwabach test D) Absolute Bone Conduction test
- A patient claiming profound unilateral deafness is subjected to the Stenger’s Test. If they deny hearing any sound when a louder tone is presented to the “deaf” ear and a softer tone to the “good” ear, what does this indicate? A) True profound unilateral deafness B) Presence of a conductive hearing loss C) Malingering or non-organic hearing loss D) A false negative Rinne’s test
MCQ Answers and Explanations:
- B) Right conductive hearing loss. A negative Rinne (BC > AC) indicates conductive hearing loss in the tested ear. Weber lateralizing to the poorer ear (in this case, the right ear) further confirms a conductive loss.
- C) 512 Hz. The 512 Hz tuning fork is universally preferred for clinical use due to its ideal decay characteristics and purity of tone.
- C) Rubbing an index finger on the patient’s tragus or using a Barany noise box. These are standard methods for masking the non-test ear during free field speech testing to prevent cross-over hearing.
- C) Conductive hearing loss. In conductive hearing loss, the occlusion effect is absent, meaning blocking the ear canal does not change the perception of bone-conducted sound.
- C) Standardization of voice intensity and ambient noise interference are common issues. These factors significantly impact the reliability and accuracy of the Free Field Voice/Speech Test.
- C) Malingering or non-organic hearing loss. A patient with genuine hearing loss will exhibit the Lombard effect (raise voice in noise). If there’s no change, it suggests they are feigning the hearing loss as they can still monitor their own speech.
- C) AC > BC. A positive Rinne indicates that air conduction is heard longer and/or louder than bone conduction, characteristic of normal hearing or sensorineural hearing loss.
- D) Absolute Bone Conduction test. This test specifically compares the patient’s bone conduction to the examiner’s with the patient’s ear canal occluded to isolate bone conduction.
- C) Malingering or non-organic hearing loss. According to the Stenger principle, the louder sound should be perceived. If the patient denies hearing anything when the louder sound is presented to the “deaf” ear, they are demonstrating a volitional response inconsistent with genuine hearing loss.
Clinical-Based Questions
Apply your knowledge to these patient scenarios, which are typical for practical exams and viva.
- Scenario: A 45-year-old male presents with a chief complaint of difficulty hearing in his left ear for the past 3 months, accompanied by intermittent ear fullness. On examination, the tympanic membrane is dull and retracted. You perform tuning fork tests. Rinne’s test in the left ear is negative, and Weber’s test lateralizes to the left.
- Diagnosis: What is your most likely diagnosis based on these findings?
- Management: Briefly outline your initial management plan for this patient.
- Viva Tips: How would you differentiate this from otosclerosis during viva?
Answer:
- Diagnosis: Left conductive hearing loss, likely due to serous otitis media (effusion in the middle ear) given the history of ear fullness and retracted tympanic membrane. The negative Rinne (BC > AC) and Weber lateralizing to the affected (poorer) ear are classic signs of conductive loss.
- Management:
- Clinical Assessment: Confirm the diagnosis with otoscopy (look for fluid, air-fluid levels).
- Audiometry: Advise pure tone audiometry and tympanometry. Tympanometry (Type B curve) would confirm middle ear effusion and decreased compliance.
- Medical Management: Nasal decongestants, antihistamines (if allergic etiology), Valsalva maneuvers (if eustachian tube dysfunction suspected).
- Follow-up: Re-evaluate after 4-6 weeks. If persistent, consider surgical options like myringotomy with grommet insertion.
- Viva Tips: In viva, you would differentiate from otosclerosis:
- Age: Otosclerosis typically presents in younger adults (20s-30s), while serous otitis media can occur at any age, often following URTI or allergy.
- Tympanic Membrane: In otosclerosis, the tympanic membrane is usually normal. In serous otitis media, it is dull, retracted, and may show fluid.
- History: Serous otitis media might have a history of recent URTI, allergies, or nasal obstruction. Otosclerosis typically has a gradual, progressive hearing loss, sometimes with a family history, and often associated with paracusis Willisii (better hearing in noise).
- Tympanometry: Type B curve for serous otitis media; Type As (shallow) or Type A (normal but with reduced compliance) for otosclerosis.
- Scenario: A 60-year-old patient complains of progressive hearing loss bilaterally over several years, worse in the high frequencies. He reports difficulty understanding speech in noisy environments. On tuning fork tests, Rinne’s test is positive bilaterally, and Weber’s test is midline.
- Diagnosis: What is the most likely diagnosis?
- Management: What would be your next step in managing this patient?
- Practical Tips: How would you explain to the patient that this type of hearing loss cannot be “fixed” surgically?
Answer:
- Diagnosis: Bilateral sensorineural hearing loss (presbycusis). The positive Rinne’s test bilaterally and midline Weber are characteristic of sensorineural loss or normal hearing. Progressive high-frequency loss and difficulty in noise strongly suggest presbycusis.
- Management:
- Comprehensive Audiometry: Advise pure tone audiometry (PTA) to confirm the degree and configuration of SNHL and speech audiometry (SRT, SDS).
- Hearing Aids: Recommend bilateral hearing aids as the primary treatment.
- Counseling: Provide counseling on communication strategies and realistic expectations.
- Rule out other causes: Consider advanced imaging (MRI) if asymmetric loss or retrocochlear pathology is suspected.
- Practical Tips (Explaining to Patient): “Sir/Madam, based on our tests, you have a type of hearing loss called sensorineural hearing loss. This means the tiny hair cells in your inner ear, which are responsible for converting sound vibrations into electrical signals for the brain, are not working as efficiently as they used to. This is often part of the natural aging process, much like vision changes with age. Unfortunately, there isn’t a surgical procedure that can repair these inner ear cells. However, we have excellent solutions like hearing aids that can amplify sounds, making them audible again and significantly improving your ability to communicate and participate in daily activities.”
- Scenario: During a medical college viva exam, the examiner asks you to demonstrate the Weber test and then asks, “Why does sound lateralize to the deaf ear in conductive hearing loss?”
- Demonstration: Briefly describe how you would demonstrate the Weber test.
- Explanation: Provide a clear, concise explanation of the phenomenon.
Answer:
- Demonstration: “Sir/Madam, to perform the Weber test, I would strike a 512 Hz tuning fork and place its base firmly on the patient’s forehead (midline). I would then ask the patient to indicate in which ear they hear the sound louder, or if they hear it equally in both ears.”
- Explanation: “The sound lateralizes to the deaf (affected) ear in conductive hearing loss primarily due to two reasons:
- Occlusion Effect: In a conductive hearing loss, the problem in the outer or middle ear (e.g., ear wax, fluid, ossicular chain fixation) prevents ambient noise from entering the inner ear via air conduction. This effectively ‘occludes’ the ear. When the bone-conducted sound from the tuning fork reaches the inner ear, there’s less competing background noise from the outside, making the bone-conducted sound relatively louder and more noticeable in the affected ear.
- Mass Effect/Impedance Mismatch: In some conductive pathologies (like otosclerosis or middle ear fluid), the impedance of the middle ear system changes. This altered impedance can actually enhance the transmission of bone-conducted sound energy to the inner ear by preventing its dissipation, making it seem louder in the affected ear.”
Frequently Asked Questions (FAQs) in Viva
These FAQs are structured for Google Rich Snippets, providing concise answers to common queries.
- What is the purpose of tuning fork tests in audiology? Tuning fork tests are rapid, inexpensive clinical tools used to differentiate between conductive and sensorineural hearing loss at the bedside, offering initial diagnostic insights.
- Why is the 512 Hz tuning fork preferred for hearing tests? The 512 Hz tuning fork is preferred because its frequency falls within the speech range, it has an optimal decay time, and it produces minimal overtones, ensuring more accurate and clinically relevant results.
- What does a “negative Rinne test” indicate? A negative Rinne test (Bone Conduction > Air Conduction) indicates a conductive hearing loss, suggesting a problem in the outer or middle ear.
- How does the Weber test help diagnose hearing loss? The Weber test helps diagnose hearing loss by indicating whether sound lateralizes to one ear; lateralization to the poorer ear suggests conductive loss, while lateralization to the better ear suggests sensorineural loss in the opposite ear.
- What is the “occlusion effect” in hearing? The occlusion effect describes the phenomenon where blocking the ear canal makes bone-conducted sound appear louder, typically observed in normal hearing and sensorineural hearing loss, but absent in conductive hearing loss.
- What is the Lombard effect and how is it used in hearing assessment? The Lombard effect is an involuntary vocal reflex where individuals raise their voice volume in noisy environments; it is used in the Lombard’s Test to detect malingering by observing if speech volume changes when noise is introduced to the “good” ear.
- Can tuning fork tests alone definitively diagnose hearing loss? No, tuning fork tests are screening tools that provide valuable preliminary information but cannot definitively diagnose or quantify hearing loss; they should always be followed by comprehensive audiometric testing.
Download full PDF Link:
Assessment of Hearing Chimani moos, Stenger’s, Teal Test Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/

Wonderful !✌️✌️✌️👍👍👍👍
Excellent explanation sir. Better than most online lectures and standard books.
Easy to understand with detailed explanation, must read .
Easy to understand!
Simple and smooth understanding, easy to relate and understand the concept… Best reference book for ENT 🔥
Explanation of each topic is very clear and easy to understand. Very helpful in writing answers in exams as well.