Definition
Myringoplasty, also called Type I tympanoplasty, is the surgical repair of the tympanic membrane perforation without any ossicular reconstruction or mastoid surgery.

Large central perforation in the tympanic membrane
Historical Background
The practice of myringoplasty has evolved significantly over the centuries.
- 1640s – Earliest attempts used animal material plugs.
- Yearsley – Described using moistened cotton wool as an artificial eardrum.
- Toynbee – Introduced gutta‑percha disc supported by silver wire.
- Wilde & Roosa – Used cautery (silver nitrate, trichloroacetic acid) on the remnant TM to stimulate closure.
- 1887, Blake – Employed paper patch technique.
- Joynt (1919) – Combined cautery + paper patch.
- Berthold (1878) – Introduced full-thickness skin grafting and coined “myringoplasty.”
- 1950s – Major advances:
• Wullstein introduced the split-skin graft method
• Zollner used pedicled grafts - In 1956, Wullstein classified tympanoplasty; myringoplasty became Type I tympanoplasty.
Indications for Myringoplasty
The primary indications for myringoplasty include:
- Recurrent Otorrhea: Persistent ear discharge.
- Hearing Loss: Resulting from chronic tympanic membrane perforation.
- Desire for Recreational Activities: Such as swimming, without the need for ear protection.
Contraindications for Myringoplasty
- Cholesteatoma or Complicated CSOM: These require a full tympanomastoidectomy (e.g., MRM or CAT), not just myringoplasty.
- Actively Allergic or Acute Discharge/Infection: ASOM, Otitis Externa, or a currently discharging ear must resolve completely before surgery.
- Contralateral dead ear is a contraindication because the patient is functionally relying on the ear to be operated on, making the risk of surgical sensorineural hearing loss unacceptable.
- Eustachian Tube Dysfunction (Severe): Myringoplasty success rate relies on a functioning Eustachian tube for middle ear ventilation. If dysfunction is severe and uncorrected, the graft failure rate is high due to negative pressure in the middle ear.
- Malignant tumours or Malignant Otitis Externa: These require a more radical excision/management.
- Patient medically unfit
Grafting Materials
The most commonly used graft materials in myringoplasty include the temporalis fascia or perichondrium (tragal or conchal) harvested from the patient.
- Temporalis fascia is the most commonly used graft for all perforations, given it is available in plenty, has low BMR, thickness is almost the same thickness as TM, and is easy to use. Ideal for large perforations and standard approaches (Postaural/Endaural).
- Tragal perichondrium is preferred for the permeatal (transcanal) approach.
- Cartilage from the tragus or concha is gaining popularity as a reliable material for repairing tympanic membrane perforations. One effective technique for smaller perforations, those less than 6mm, involves creating a cartilage “butterfly.” In this method, a cartilage disc is circumferentially incised by 1mm. This groove is then fitted into the perforation rim, stabilising the graft and ensuring a secure fit.
- Occasionally, homografts such as dura mater, vein, fascia, or cadaver tympanic membrane may be utilised.
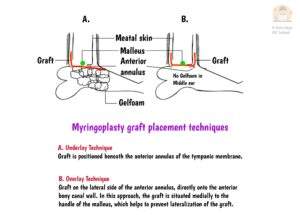
Graft Placement Techniques
- Underlay Technique: The graft is positioned medial to the inner mucosal layer (below all three layers of the TM remnant) and hence below the fibrous annulus. It is stabilised by placing gelfoam in the middle ear. The underlay technique is considered superior for several reasons. It offers technical ease during the procedure, results in a shorter post-operative healing time, has fewer complications, and provides better hearing gain for patients. This technique may lead to complications like graft medialization, reduced middle ear space, danger of leaving residual epithelium and anterior blunting. It is essential to avoid nitrous oxide gas during graft placement, as it can diffuse into the middle ear and displace the graft.
- Interlay Technique: The graft is placed between the mucosal and fibrous layers of the TM remnant. This approach offers superior stability, effectively preventing both graft medialization and lateralisation (unlike underlay and overlay). Consequently, it boasts a high success rate (over 90%) with minimal complications like formation of epithelial pearls, anterior blunting and reduced middle ear space.
- Overlay Technique: The graft is placed lateral to the middle fibrous layer of the tympanic membrane remnant and hence over the fibrous annulus. This technique requires careful removal of the outer epithelial layer of the tympanic membrane remnant. Although the overlay technique can provide good results, it is associated with a higher incidence of complications, including the formation of epithelial pearls, anterior sulcus blunting, granulation tissue formation, and graft lateralisation. It is considered a more technically demanding procedure. Best suited for large/subtotal/anterior perforations.
- Inlay Technique/ Butterfly Cartilage: In this method, a cartilage or cartilage-perichondrium disc is circumferentially incised by 1mm. This groove is then fitted into the perforation rim, stabilising the graft and ensuring a secure fit. There is no need to tympanomeatal flap in this technique. Best suited for perforations less than 6mm.
Procedural Steps:
- EUM: Examination under the microscope is done to confirm the clinical findings.

- For local anaesthesia, 2% xylocaine with adrenaline is injected in the postaural region (from the root of the helix to the mastoid tip) and external auditory canal.

- Wilde’s incision: A postaural incision is given from the root of the helix to the mastoid tip.


- Temporalis fascia graft is harvested.

- The margins of the perforation are freshened by removing the epithelial margins of the perforation to create a bleeding bed conducive to graft adherence.

- A tympanomeatal flap, consisting of the posterior meatal canal skin, is elevated which is made in continuity with the tympanic membrane after dislocating the annulus from the sulcus.

- The incision is given in the middle ear mucosa below the annulus and the tympanomeatal flap is elevated.

- The handle of the malleus is denuded.

- The middle ear and ossicular chain are inspected and repaired as necessary.
- Any posterosuperior overhang of the bony meatus, if present, is removed to enhance the visibility of the ossicles.
- The middle ear is packed with gelfoam.

- The graft is placed medial to the tympanic membrane remnant or tympanic annulus, and lateral to the manubrium of the malleus. (Underlay technique)
- The tympanomeatal flap is returned to its original position, and the medial aspect of the ear canal is packed with gelfoam impregnated with antibiotic ointment.
- The postaural incision is closed in two layers.
Complications of Myringoplasty
Potential complications associated with myringoplasty include:
- Intraoperative Bleeding: Often due to a high and uncovered jugular bulb.
- Myringitis: Inflammation of the tympanic membrane.
- Wound Infection: Including perichondritis.
- Wound Hematoma: Accumulation of blood in the wound area.
- Injury to Chorda Tympani: A nerve that can be affected during surgery.
- Graft Failure: The potential for the graft to not adhere or integrate properly.
- Sensorineural Hearing Loss or Dizziness: Possible adverse effects following the procedure.
———— End of the chapter ————
High-Yield Points for Quick Revision (NEET PG MCQs)
- Myringoplasty = Type I Tympanoplasty.
- Coiner of “Myringoplasty”: Berthold (1878).
- Most Common Graft Material: Temporalis Fascia.
- Preferred Graft for Permeatal Approach: Tragal Perichondrium.
- Underlay Technique: Graft is medial to the TM remnant (easier, less complication, preferred). N2O use is contraindicated.
- Overlay Technique: Graft is lateral to the TM remnant (requires epithelial removal, higher risk of lateralization/blunting).
- Contraindication: Operating on an actively discharging ear or a patient with a contralateral dead ear.
- Complication: Graft failure is the most frequent surgical failure.
Clinical Scenarios and Viva Voce
Scenario 1: Pre-operative Assessment
A 40-year-old male presents with a history of recurrent ear discharge 5 years ago, which resolved. Otoscopy shows a dry, medium-sized central perforation. PTA shows a 30 dB conductive hearing loss. CT scan confirms a clear mastoid.
Viva Questions and Answers:
- Q: Is this patient fit for myringoplasty, and which approach is best?
- A: Yes, the patient is an ideal candidate because the ear is dry, and there is no evidence of cholesteatoma. Given the central perforation, a Postaural approach using a Temporalis Fascia underlay graft is the most conventional and reliable method.
- Q: If the perforation was small, what simple procedure could you attempt first?
- A: For perforations <3 mm, we could attempt a chemical cautery (e.g., Trichloroacetic Acid) of the perforation edge followed by a paper patch application in the clinic.
Scenario 2: Postoperative Complication
Three months after an underlay myringoplasty, the patient complains of persistent altered taste on the tongue on the operated side.
Viva Questions and Answers:
- Q: What is the most likely cause of this symptom?
- A: Injury to the Chorda Tympani nerve, which supplies taste sensation to the anterior two-thirds of the tongue. The surgeon might have accidentally stretched or injured it during the elevation of the tympanomeatal flap near the posterior annulus.
- Q: Is the chorda tympani injury permanent?
- A: No, typically not. Since it is a sensory nerve, most taste disturbances resolve spontaneously, usually within 6–12 months.
Multiple Choice Questions (MCQs) for NEET PG
- Myringoplasty is classified as which type of tympanoplasty according to Wullstein? A. Type II B. Type I C. Type III D. Type IV
- Which of the following conditions is considered a contraindication for elective myringoplasty? A. Dry central perforation B. Contralateral dead ear C. Mild conductive hearing loss D. Desire for swimming
- The most common graft material used in modern myringoplasty is: A. Vein graft B. Cartilage C. Temporalis fascia D. Tragal perichondrium
- In the underlay technique of myringoplasty, the graft is placed: A. Lateral to the malleus handle. B. Lateral to the TM remnant. C. Over the fibrous layer only. D. Medial to the TM remnant and annulus.
- The major disadvantage associated with the overlay technique compared to the underlay technique is a higher risk of: A. SNHL B. Graft medialization C. Injury to the facial nerve D. Anterior sulcus blunting
- The primary purpose of freshening the edges of the tympanic membrane perforation before grafting is to: A. Reduce the size of the perforation. B. Access the middle ear space. C. Remove epithelium and promote new blood vessel growth. D. Visualize the ossicles.
- Who is credited with coining the term “myringoplasty” after describing the use of a full-thickness skin graft? A. Wullstein B. Toynbee C. Blake D. Berthold
- Which graft material is becoming popular for high-risk perforations due to its resistance to negative pressure? A. Temporalis fascia B. Vein C. Cartilage D. Dura mater
- Postoperative taste disturbance after myringoplasty is most commonly due to injury to the: A. Facial nerve B. Vestibular nerve C. Chorda tympani nerve D. Glossopharyngeal nerve
- Which statement is TRUE regarding Nitrous Oxide (N2O) anesthesia during myringoplasty with an underlay graft? A. N2O is safe to use as it aids visibility. B. N2O helps stabilize the graft. C. N2O can diffuse into the middle ear and displace the graft. D. N2O is only contraindicated if the ossicles are being repaired.
Answers and Explanations:
- B. Type I is repair of the TM only; the remaining types involve ossicular repair.
- B. A contralateral dead ear makes the risk of SNHL (though rare) on the operated ear unacceptable as it is the patient’s only hearing ear.
- C. Temporalis fascia is the traditional and most widely used graft due to its excellent healing properties and accessibility.
- D. The graft is placed under the remnant and over the annulus/fibrous layer.
- D. Anterior sulcus blunting (thickening/rounding of the angle between the TM and the anterior canal wall) is a characteristic complication of the overlay technique due to the large epithelial removal required.
- C. Freshening removes the epithelial layer that has grown over the edges, creating a raw surface to allow the new graft to epithelialize and take.
- D. Berthold coined the term in 1878.
- C. Cartilage is inherently stronger and more rigid, making it less likely to retract or fail under negative middle ear pressure.
- C. The chorda tympani is exposed and susceptible to trauma during the elevation of the tympanomeatal flap.
- C. N2O is highly diffusible and can build up pressure in the middle ear, leading to graft displacement, so it must be avoided during graft placement.
Frequently Asked Questions in Viva
- What is the definition of Myringoplasty? Myringoplasty is the surgical repair of the tympanic membrane perforation without simultaneously operating on the ossicles or mastoid.
- What is the most common reason for myringoplasty graft failure? The most common reason for myringoplasty graft failure is poor or persistent Eustachian tube dysfunction (ETD), which causes continuous negative pressure in the middle ear.
- Which surgical technique is generally preferred, underlay or overlay? The underlay technique is generally preferred because it is technically easier, has a shorter healing time, and is associated with fewer major complications like blunting.
- How long does it take for a myringoplasty graft to heal? While initial healing is visible within weeks, the graft usually takes 3 to 6 months to fully stabilize and for hearing to reach its final level.
- Is myringoplasty the same as tympanoplasty? No, myringoplasty is a Type I Tympanoplasty. Tympanoplasty is the broader term covering all surgical procedures to reconstruct the eardrum and/or ossicles.
———-End———–
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Comprehensive guide on myringoplasty (eardrum repair) for MBBS and ENT PG students — covering indications, techniques (underlay, overlay, butterfly, cartilage), complications, MCQs, clinical cases, mnemonics, and high-yield facts, Myringoplasty technique and indications, Underlay vs overlay myringoplasty, Butterfly cartilage myringoplasty, Graft materials in tympanoplasty, Success rate of myringoplasty 2025, Endoscopic myringoplasty without flap, NEET PG ENT myringoplasty MCQ’s, Complications of myringoplasty procedure, ENT topics for NEET PG, MBBS ENT notes Myringoplasty, ENT viva questions tympanoplasty, Myringoplasty underlay vs overlay, Type 1 tympanoplasty procedure steps, Graft materials for eardrum repair, Contraindications for myringoplasty, Complications of ear drum surgery, Myringoplasty Technique And Indications, Underlay Vs Overlay Myringoplasty, Butterfly Cartilage Myringoplasty, Graft Materials In Tympanoplasty, Success Rate Of Myringoplasty 2025, Endoscopic Myringoplasty Without Flap, NEET PG ENT Myringoplasty MCQ, Complications Of Myringoplasty Procedure

excellent