|
The following CBME core competencies are covered in this chapter.
|
Vestibular Function Tests.
The central nervous system receives information from the vestibular system (inner ear), visual (eye) and proprioceptive sensory inputs (body position sense). The human brain uses all of this information and regulates the equilibrium and body posture by coordinating the eyes, head, and body during movements. The equilibrium and body posture system is like a two-sided push and pull system, which is equal on both sides during the neutral position. As a result, any disruption in these inputs—whether from trauma, disease, or degeneration—can lead to symptoms like dizziness or vertigo.
Vestibular function tests are broadly divided into two groups:
- Clinical tests (Bedside Examination): These are simple, quick tests performed in the clinic without specialised equipment.
- Laboratory Tests (Instrumental Evaluation): These quantitative tests use specialised equipment to objectively measure and analyse vestibular system responses, offering precise diagnostic information.
| Type | Tests |
|---|---|
| Clinical tests (Bedside Examination) | 1. Spontaneous Nystagmus 2. Corneal Reflex (Blink Reflex) 3. Fistula test 4. Romberg's Test and Sharpened Romberg Test 5. Gait Test 6. Tandem Gait Test 7. Unterberger Stepping Test (Fukuda Stepping Test) 8. Past-pointing Test (Pointing Test) 9. Dix-Hallpike Maneuver (Positional Test) |
| Laboratory Tests (Instrumental Evaluation) | 1. Caloric Test 2. Electronystagmography (ENG) / Videonystagmography (VNG) 3. Optokinetic Test 4. Rotational test 5. Cupulometry 6. Galvanic Test 7. Posturography (Dynamic Posturography) 8. Vestibular Evoked Myogenic Potentials (VEMPs) |
Clinical tests of vestibular functions
1. Spontaneous Nystagmus
Nystagmus is an important tell-tale sign in the evaluation of vestibular function. Nystagmus is defined as a rhythmical, involuntary, oscillatory movement of the eyes without a cognitive, visual or vestibular stimulus. The direction of nystagmus may be horizontal, vertical or rotatory. Generally, horizontal canal lesions produce horizontal nystagmus, superior (anterior) canal lesions cause rotatory nystagmus, and posterior canal lesions lead to vertical nystagmus.
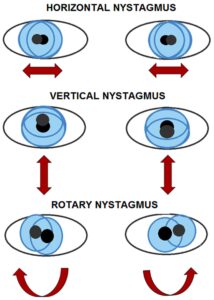
Diagram: Types of Nystagmus
Mechanism of Vestibular Nystagmus: Vestibular nystagmus comprises two distinct components or phases:
Vestibular nystagmus has a slow and a fast component. The ‘slow phase’ is due to the abnormality in the vestibular system, while the ‘fast phase’ is due to the corrective central mechanism that brings the eyes back to the primary position. However, while only the slow phase plays a part in image stabilisation, it is the fast phase that is actually detected, and hence by convention, the direction of the nystagmus is attributed to that of its fast phase.
For example, in acute right-sided vestibular failure, the slow phase is towards the right (the weak side), but the fast phase will be to the left, thus causing left-beating nystagmus. However, crucial for interpretation, the patient’s past-pointing and falling will still occur towards the slow component, indicating the side of vestibular weakness (i.e., towards the right in this example).
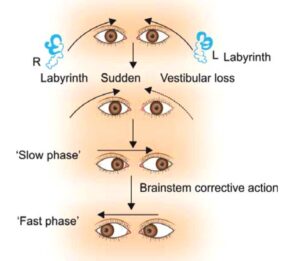
Diagram: Showing machanism of nystagmus
Degree of nystagmus. Intensity of nystagmus is indicated by its degree.
| 1stdegree | It is a weak nystagmus and is visible only when the patient looks in the direction of the fast phase |
| 2nddegree | It is stronger than 1st degree and is visible even when the patient looks straight ahead. |
| 3rddegree | It is stronger than 2nd degree and is visible even when the patient looks in the opposite direction of the fast phase |
*These degrees of nystagmus are according to Alexander’s law and may not hold true in case of nystagmus of central origin.
How to look for nystagmus.
Patient is asked to sit on the examination chair or may lie supine on the bed. The clinician keeps his finger about 30 cm centrally in front of the patient’s eyes. The clinician moves his finger in all four directions (up, down, left, right) and asks the patient to follow his finger. The finger should not move beyond 30 degrees from the initial central position, as it will induce physiological “gaze-evoked nystagmus,” which is not indicative of pathology. The presence of spontaneous nystagmus strongly suggests an organic lesion. Differentiating its origin (peripheral vs. central) is paramount for diagnosis and management.

Table: Differentiating Peripheral vs. Central Nystagmus
| Feature | Peripheral Nystagmus | Central Nystagmus |
|---|---|---|
| Lesion Site | Labyrinth or Vestibulocochlear nerve (VIIIth CN) | Central neural pathways (vestibular nuclei, brainstem, cerebellum) |
| Fatiguability | Fatiguable (decreases with repeated testing) | Non-fatiguable (persists with repeated testing) |
| Reproducibility | Reproducible (can be elicited again) | Non-reproducible (variable or inconsistent) |
| Optic Fixation | Suppressed by optic fixation (looking at a fixed point); Enhanced in darkness or with Frenzel glasses (+20 dioptre, abolish optic fixation). | Not suppressed by optic fixation. |
| Direction | Unidirectional (fast phase always beats in one direction); Typically horizontal or horizontal-rotatory. | Often multidirectional (vertical, purely torsional, or changing direction with gaze). |
| Associated Symptoms | Severe vertigo, nausea, vomiting, hearing loss, tinnitus. | Milder vertigo; often associated with other neurological signs (e.g., ataxia, diplopia, dysarthria). |
| Specific Patterns | - Irritative lesions (e.g., serous labyrinthitis) cause nystagmus towards the lesion side. - Paretic lesions (e.g., purulent labyrinthitis, VIIIth nerve section) cause nystagmus towards the healthy side. | - Torsional nystagmus (lesion of the brainstem/vestibular nuclei); - Downbeat nystagmus (craniocervical junction, cerebellar degeneration); - Upbeat nystagmus (pons/medulla junction); - Pendular nystagmus (congenital, MS); Disconjugate nystagmus. |
2. Corneal reflex (Blink reflex).
Normally there is an involuntary bilateral blinking (closure) of the eyelids elicited by touching the cornea.
The reflex is mediated by:
- Afferent pathway: via the ophthalmic branch (V1) of the trigeminal nerve (CN V) sensing the stimulus on the cornea only.
- Efferent pathway: via the facial nerve (CN VII) initiating the motor response (efferent fiber) to oculi orbicularis
- Center: (nucleus) is located in the pons of the brainstem.
Method. A small wisp of cotton wool is touched on the cornea on the lateral aspect without touching eyelashes and conjunctiva while the patient is asked to look forward and straight. Look for blinking and tearing in both the eyes.
Interpretations. The corneal reflex may be slowed or absent in disorders that affect the trigeminal nerve, facial nerve, or brain stem nuclei, such as posterior fossa and cerebellopontine angle tumours, such as acoustic neuroma.
3. Fistula test
The fistula test identifies an abnormal communication (fistula) between the middle and inner ear. Normally, pressure changes in the external ear canal do not transmit to the labyrinth.
Principle. If a fistula exists, pressure changes applied to the external auditory canal transmit to the labyrinth, stimulating it and inducing nystagmus and vertigo.
Method. The test is performed by applying intermittent pressure on the tragus or by using Siegel’s speculum, in order to produce pressure changes in the ear canal. If there is existence of an abnormal communication between the middle and inner ear, the pressure changes are transmitted to the labyrinth. Stimulation of the labyrinth results in nystagmus and vertigo. The direction of nystagmus is observed. The direction of nystagmus will be to the opposite side in positive fistula test.
Interpretations.
(i) Negative test (i.e. No fistula).
- Normally the pressure changes in the external auditory canal cannot be transmitted to the labyrinth
- When the labyrinth is dead (non-functioning), no nystagmus will be elicited even with a fistula.
(ii) Positive test (i.e. fistula present). Common causes include:
- Erosion of the horizontal (lateral) semi-circular canal (e.g., due to cholesteatoma) or a surgically created window in the horizontal semi-circular canal (e.g., following fenestration operation).
- Abnormal opening in the oval window (post-stapedectomy fistula) or the round window (rupture of round window membrane).
In another way, a Positive fistula also implies that the labyrinth is still functioning.
(iii) False negative fistula (i.e. negative fistula test but fistula is present) test is seen when fistula is there but is covered by cholesteatoma or granulation tissue and does not allow pressure changes to be transmitted to the labyrinth.
(iv) False positive fistula test (i.e. positive fistula test without the presence of a fistula) is seen in
- Congenital syphilis. Annular ligament is lax and mobile, causing the stapes footplate to be hyper-mobile.
- 25% cases of Meniere’s disease. It is due to the fibrous bands connecting the utricular macula to the stapes footplate.
This false positive phenomenon is also known as Hennebert’s sign.
Tullio’s Phenomenon: This refers to giddiness or vertigo produced by loud noise rather than pressure. It is typically associated with labyrinthine fistula and can occur after fenestration surgery.
4. Romberg’s Test and Sharpened Romberg Test
These tests assess static balance by challenging proprioceptive and vestibular inputs, especially when visual input is removed.
Method:
- The patient removes shoes and stands with feet together, arms by their side. The examiner must stand close by for safety.
- First, the patient stands quietly with eyes open. This allows visual compensation.
- Then, the patient stands with eyes closed. With visual input lost, the vestibular and proprioceptive systems are put to a greater test.
- If the patient can perform this without significant sway, proceed to the Sharpened Romberg Test: The patient stands in a heel-to-toe position (tandem stance), with one foot directly in front of the other. Arms are folded across the chest.
Interpretations:
- Peripheral Vestibular Lesions: The patient sways and tends to fall towards the side of the lesion, especially with eyes closed. Inability to perform the sharpened Romberg test strongly indicates vestibular impairment.
- Central Vestibular Disorders: Patients often exhibit swaying or instability even with their eyes open, indicating a more profound and often multi-sensory balance deficit.
- A “wooden soldier” fall (straight backward without correction) is frequently non-organic or psychogenic.
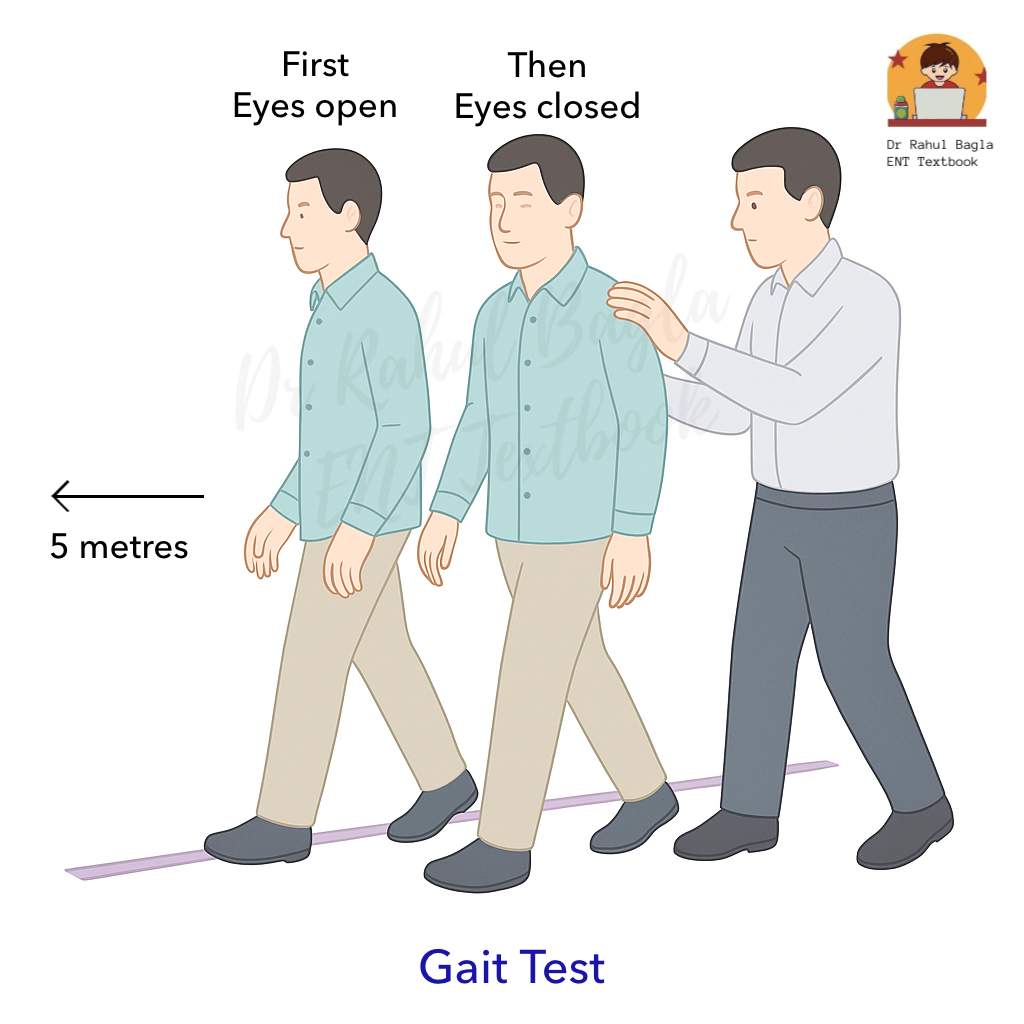
5. Gait Test
Method. The patient is asked to walk along a straight line in normal speed for 5 metres to a fixed point, first with eyes open and then closed. The examiner walks alongside to prevent the person from falling over and hurting himself.
Interpretation. In the case of recent vestibular hypofunction, with eyes closed, the patient tends to deviate to the affected side.
6. Tandem Gait Test
Method. The patient is asked to take 10 heel-to-toe steps in a straight line in normal speed with arms folded on the chest, first with eyes open and then closed. The examiner walks alongside the patient for safety reasons and looks out for deviation towards the side of the lesion.
With the eyes open, this primarily tests cerebellar function as the visual components compensate for chronic vestibular and proprioceptive deficits. However, tandem walking with closed eyes is a good test of vestibular function, assuming that the visual and proprioceptive functions are intact.
Interpretation.
- Peripheral Vertigo: Patients may exhibit some impaired balance but can usually still walk.
- Central Vertigo: Patients with central lesions often cannot walk or even stand without falling, highlighting a more severe imbalance.
7. Unterberger Stepping Test (Fukuda Stepping Test)
This test identifies the tendency of patients with vestibular imbalance to turn while walking, indicating the side of the lesion.
Method. The patient is asked to march on the spot 50 times with the arms extended and eyes closed. Repetition of the test is essential for consistency.
Interpretation.
- A positive test is indicated by rotational movement of the patient towards the side of the lesion by more than 30-45 degrees or displacing forward/backwards by more than 50cm.
- Patients having unilateral paralytic labyrinthitis will rotate to the side of the lesion.
- Patients having active irritative lesions will not be able to perform the test
8. Past-pointing Test
Past pointing means the movement of a pointing finger that goes beyond the intended mark. This is called overshooting and is a manifestation of dysmetria (inability to control the range of motion).
Method. The patient stands in front of the clinician. The clinician extends his arms and points both of his index fingers approximately 15cm (6 inches) apart. The patient is asked to lift both arms over the head and then bring the arms down to touch his index fingers to the clinician’s index fingers.
Interpretation.
- Normally, the patient can perform the test without difficulty.
- Vestibular Disease: Patients have difficulty lining up with the clinician’s fingers and will consistently “past-point” (overshoot) towards the side of the vestibular lesion.
- Clinical Correlation: Importantly, the direction of past-pointing, falling during Romberg, the slow component of nystagmus, and the turn in the Unterberger test all point towards the side of the vestibular lesion.
9. Dix-Hallipke Manoeuvre (Positional Test)
This manoeuvre is critical for diagnosing Benign Paroxysmal Positional Vertigo (BPPV) and differentiating peripheral from central positional vertigo. This test should be conducted when the patient complains of vertigo provoked by specific head–neck movements or in certain head positions. Typical symptoms are brief intense spells of rotatory vertigo which usually precipitates during an abrupt change in head position, getting out of bed, turning over in bed, bending over, looking up or when extending or flexing the neck.
Dix-Hallpike Manoeuvre test is done to elicit vertigo, and the patient should be informed and warned beforehand. Careful examination of the patient’s eyes is essential during the test. It also helps to differentiate a peripheral from a central lesion.
Method.
- The patient sits on the examination couch with legs extended.
- The examiner holds the patient’s head, turns it to approximately 45° horizontally to the right.
- During the complete procedure patient is required to keep his eyes open and should look at one point on the examiner’s face (i.e. the nose or bridge of the nose).
- Then the patient is guided into a supine position so that his head hangs over the edge of the couch, approximately 30° below the horizontal.
- Keep the patient in the head-down position for a few (20-30) seconds
- Observe the patient’s eyes for nystagmus, and ask about the onset and intensity of vertigo.
- Gently help the patient return to the sitting position. Allow them to recover before repeating the test.
- Repeat the entire procedure with the head turned to the left.
- If both sides are negative, perform the test with the head in a straight-hanging position (testing the superior semicircular canals, though BPPV commonly affects the posterior canal).

Four parameters of nystagmus are observed to differentiate peripheral (typically BPPV) from central positional nystagmus:
- Latency: The delay between assuming the provocative position and the onset of nystagmus/vertigo.
- Duration: How long does the nystagmus and vertigo last?
- Direction: The characteristic beating pattern of the nystagmus.
- Fatiguability: Whether the nystagmus and vertigo diminish with repeated testing in the same position.
Table: Differentiating Peripheral vs. Central Positional Nystagmus (Dix-Hallpike Findings).
Positional nystagmus in peripheral and central lesions of the vestibular system. Positional nystagmus is elicited by the Hallpike manoeuvre.
| Feature | Peripheral | Central |
| Latency | 2–20 s | No latency (immediate onset) |
| Duration | Less than 1 min | More than 1 min |
| Direction of nystagmus | Direction fixed, towards the under-most ear | Direction changing |
| Fatiguability | Fatiguable (decreases or disappears with repeated testing in the same position) | Non-fatiguable (persists with repeated testing) |
| Accompanying symptoms | Severe vertigo | None or slight |
| Intensity of vertigo | Severe | Mild |
| Reproducibility | Non-reproducible | Reproducible |
| Incidence | Common | Rare |
Laboratory Tests for Vestibular Functions.
These tests help to confirm the diagnosis and allow objective and quantitative evaluation of peripheral vestibular function and the vestibular-ocular reflex.
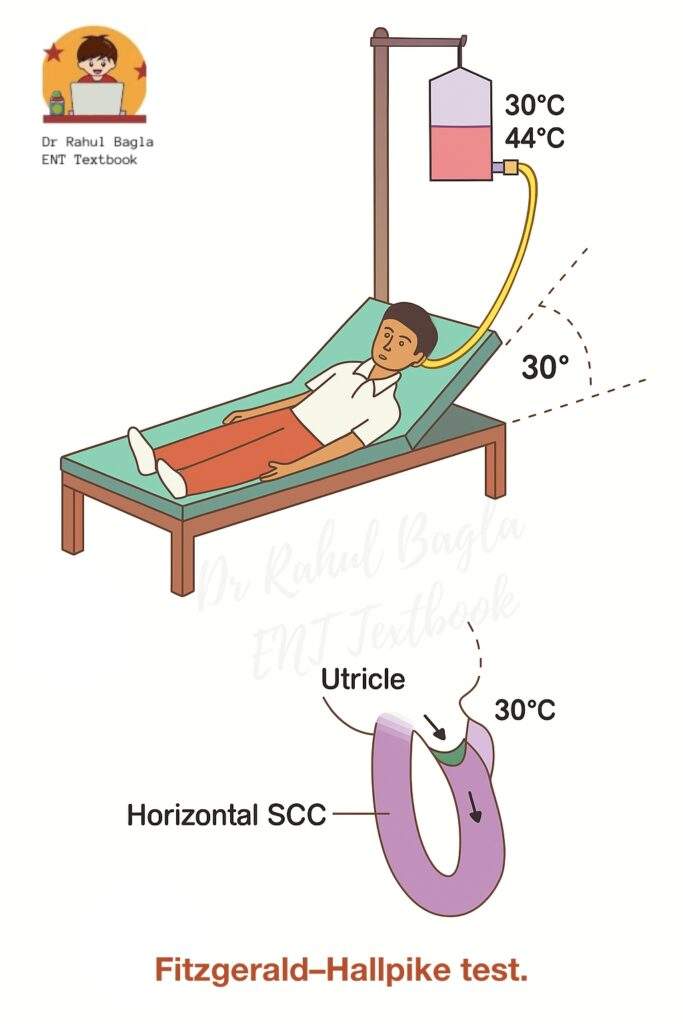
1. Caloric Test
The caloric test checks how well each ear’s balance system (labyrinth) is working by making changes in temperature in the external auditory canal through hot or cold water. The caloric test induces nystagmus (involuntary eye movements). The advantage of the test is that it evaluates each ear separately, unlike rotational tests (which test both ears together). If the induced vertigo is similar to one patient’s experience, it proves the labyrinthine origin of vertigo. However, some patients may not tolerate the induced vertigo and discomfort.
Principle: Irrigation with water at 30 or 44°C (37 ± 7°C) for 40 seconds is the standard procedure. A 5-minute interval between consecutive irrigations allows the temporal bone temperature to normalize.
- Hot Water (44°C): Heats the endolymph in the horizontal semicircular canal. The heated endolymph becomes less dense, rises, and creates a flow towards the ampulla, deflecting the cupula. This simulates a head rotation to the irrigated side (same side), producing nystagmus with the fast phase to the irrigated side.
- Cold Water (30°C): Cools the endolymph, making it denser. It sinks, creating a flow away from the ampulla. This simulates a head rotation to the opposite side, producing nystagmus with the fast phase to the opposite side.
Mnemonic: COWS (Cold Opposite, Warm Same)
- Cold water/air induces nystagmus with a fast phase to the Opposite side.
- Warm water/air induces nystagmus with a fast phase to the Same side.
Methods. The caloric test is typically performed using one of three primary methods.
- Modified Kobrak Test
- Fitzgerald-Hallpike Bi-thermal Caloric Test
- Cold-air Caloric (Dundas Grant’s) Test.
A. Modified Kobrak Test (Quick Office Procedure)
The Modified Kobrak Method is a quick in-office procedure that precisely controls temperature to stimulate the ear, typically using a small volume of water or air for a localised effect.
Method.
- The patient sits with their head tilted 60 degrees backwards. This position places the horizontal semicircular canal in a vertical orientation.
- The ear is irrigated with ice water for 60 seconds, starting with a small volume and gradually increasing it if there’s no response:
- Begin with 5 mL of ice water.
- If no response, increase to 10 mL, then 20 mL, and finally 40 mL.
Interpretation.
- Normal Response: A normal response is the presence of nystagmus (involuntary eye movements) beating toward the opposite ear when 5 mL of ice water is used.
- Hypoactive Labyrinth: If nystagmus is only observed with increased volumes of water (between 5 mL and 40 mL), it suggests the labyrinth (inner ear balance organ) is hypoactive (underactive).
- Dead Labyrinth: If there is no nystagmus even after irrigating with 40 mL of ice water, it indicates a dead labyrinth.
B. Fitzgerald-Hallpike Bi-thermal Caloric Test:
Method.
- The patient reclines on the couch at 30 degrees (so that horizontal SCC comes in a vertical position).
- Examine both ears for wax or tympanic membrane (TM) perforations. (If TM is perforated, use air instead of water).
- Alternatively, irrigate each ear with water at 30°C and 44°C for 40 seconds.
- Observe and record the nystagmus (duration, amplitude, frequency) using electronystagmography (ENG) or videonystagmography (VNG). The total time is recorded from the start of irrigation to the end of nystagmus and charted on a calorigram.
- If no nystagmus is elicited, repeat the test with 20°C water for 4 minutes before concluding a “dead labyrinth.”
Interpretations (Most Common Findings): Both canal paresis and directional preponderance must be greater than 15-20% to be clinically significant.
- Canal Paresis (CP): One ear is weaker
- Definition: The response (measured as nystagmus duration) to both cold & warm is much less on one side than on the opposite side. It reflects the weak function of the ipsilateral labyrinth, vestibular nerve, or vestibular nuclei.
- Calculation: [(RC + RW) – (LC + LW)]
% CP = _____________________________________ x 100
(RC + RW + LC + LW)
where R/L = Right/Left ear, C/W = Cold/Warm irrigation response). - Commonly seen in Meniere’s disease, vestibular schwannoma, post-labyrinthectomy, or vestibular nerve section.
- Directional Preponderance (DP): Nystagmus is stronger in one direction
- Definition: The total duration of nystagmus beating in one direction is significantly greater than the nystagmus beating in the opposite direction.
- Calculation: [(RW + LC) – (LW + RC)]
% DP = ____________________________________ x 100
(RC + RW + LC + LW)
(where R/L = Right/Left ear, C/W = Cold/Warm irrigation response for respective beating direction). - Clinical Significance: This can be seen in both central and peripheral lesions. DP towards the side of a central lesion, and away from the side of a peripheral lesion (due to an irritative lesion). Further investigations (e.g., BERA, CT/MRI) are required for differentiation and localisation. If nystagmus is 25–30% or more on one side, it indicates directional preponderance.
- Specific Patterns:
- CP + Contralateral DP: Commonly seen in Meniere’s disease.
- CP + Ipsilateral DP: Often seen in acoustic neuroma.
- No nystagmus at all: Indicates a dead labyrinth or bilateral hypofunction
C. Cold-air Caloric (Dundas Grant’s) Test. Cold air is introduced into the ear by pouring ethyl chloride in the Dundas grant tube, which is a coiled copper tube wrapped in cloth. This test is used when there is perforation in the eardrum.
2. Electronystagmography.
It detects and records spontaneous or induced nystagmus that is not seen with the naked eye. A pair of disposable surface electrodes is placed around the orbit, which records the difference in potential between the cornea and the retina (corneoretinal potentials). It is a relatively easy, non-invasive test and allows a proper, permanent, documented record of nystagmus for future reference and medicolegal cases. It cannot record torsional eye movements.
3. Optokinetic Test
This test is used to diagnose a central lesion.
Principle. In response to repetitive visual patterns, such as a series of moving stripes or a large striped curtain in front of our eyes. The eyes follow one object with a slow-phase movement. The eyes are reset in the orbit by a fast component. This sequence of slow ipsilateral and fast contralateral eye movements forms optokinetic nystagmus.
Method. Patient is instructed to look straight ahead rather than follow a series of vertical stripes on a drum or open magazine moving slowly in both directions, and the results are analysed.
Interpretation.
- Normal nystagmus. Nystagmus with a slow component in the direction of moving stripes and a fast component in the opposite direction.
- Abnormal nystagmus. It is usually seen in brainstem and cerebral or other central disorders.
4. Rotational Tests
The rotational chair is used for analysing horizontal canal vestibulo-ocular reflex (VOR).
Method. The patient is asked to sit in a motorised and computer-controlled chair (Barany’s revolving chair) without optical fixation. The revolving chair delivers the desired velocity and rotational waveforms. The patient’s head is comfortably immobilised and kept in a tilted 30° forward position. The chair is rotated in either direction and is stopped suddenly, and the resulting nystagmus is carefully monitored and recorded using either ENG or VNG. Normally, nystagmus lasts for 25–40 s. The test is useful as it can be performed in cases of congenital abnormalities where the ear canal has failed to develop, and it is not possible
Further, it can be performed in two ways.
- Sinusoidal rotation stimulation. The chair is rotated sinusoidally over a range of frequencies, e.g. from approximately 0.05Hz to 1Hz, while the peak velocity of the stimulus is kept constant
- Velocity step or ‘impulsive’ rotational test. There is an abrupt increase in chair velocity, say from a stationary position to 60 or 90 degrees per second, measuring the per- and post-rotation responses to clockwise and anti-clockwise. This complete procedure is then repeated in the opposite direction.
These tests are generally available in higher centres and provide a less provocative alternative to the caloric test. This test provides an alternative to the caloric test and is tolerated well by children. However, both labyrinths are tested simultaneously and do not give information about the site of the lesion and are relatively expensive.
Interpretation. There are three main abnormalities seen.
| Response | Disorder |
| Bilateral reduced or No Response | Seen in bilateral vestibular failure, ototoxicity, post-meningitis and idiopathic. |
| Asymmetric response or Directional preponderance. | Seen in vestibular system disorder. |
| Loss of VOR suppression | Seen in central disorder. |
5. Cupulometry
6. Galvanic test
7. Posturography
8. Vestibular Evoked Myogenic Potentials (VEMP)
Cerebellar Function Tests
- Asynergia (abnormal finger-nose test). The patient touches the tip of his nose with his forefinger and then touches the clinician’s finger, held within the reach of the outstretched arm of the patient. The test is repeated as fast as the patient can. The position of the clinician’s finger can be changed to make the test more sensitive. Patients having cerebellar dysfunction will not be able to touch the nose on the first attempt (dysmetria). The reason is that intention tremors are more pronounced as the hand approaches the face.
- Dysmetria (inability to control range of motion). i.e. movements are incorrect in range, direction and force. The movements may overshoot their intended mark (hypermetria) or fall short of it (hypometria).
- Adiadochokinesia (inability to perform rapid alternating movements). e.g. supination and pronation of the forearm or patting the palm of one hand to the palm and back of the other hand.
- Rebound phenomenon (inability to control movement of extremity when opposing forceful restraint is suddenly released). When the patient attempts to do a movement against resistance, and if the resistance is suddenly removed, the limb moves forcibly in the direction towards which the effect was made. This is called the rebound phenomenon. It is due to the absence of the breaking action of antagonistic muscles.
———— End of the chapter ————
High-Yield Points for Quick Revision
- The vestibular system is crucial for equilibrium and posture.
- Nystagmus indicates vestibular dysfunction; differentiate peripheral vs. central based on fatiguability, direction, and effect of optic fixation.
- COWS mnemonic for caloric test: Cold Opposite, Warm Same.
- Dix-Hallpike manoeuvre is the gold standard for BPPV diagnosis. Look for latency, duration, direction, and fatiguability of nystagmus.
- Canal Paresis (CP) and Directional Preponderance (DP) are key interpretations of the caloric test, with specific associations (e.g., CP + Contralateral DP in Meniere’s, CP + Ipsilateral DP in acoustic neuroma).
- Past-pointing, Romberg’s fall, slow phase of nystagmus, and Unterberger turn all indicate the side of the vestibular lesion.
- VEMPs specifically test otolith organ function (cVEMP for saccule, oVEMP for utricle).
- Fistula test detects abnormal communication between middle and inner ear; remember Hennebert’s sign (false positive).
- Romberg’s test assesses static balance, differentiating proprioceptive/vestibular issues from cerebellar issues (eyes open vs. eyes closed).
Practical Tips for Viva and Clinical Exam Scenarios
- Presenting a Case: When presenting a patient with vertigo, always start with the onset, duration, and associated symptoms (hearing loss, tinnitus, neurological deficits). This immediately points towards peripheral vs. central causes. Example Viva Question: “A patient presents with sudden onset, severe rotatory vertigo lasting minutes, associated with nausea but no hearing loss. What’s your top differential and how do you confirm it?” (Answer: BPPV, confirmed by Dix-Hallpike).
- Performing Dix-Hallpike: Always warn the patient about inducing vertigo. Maintain eye contact to observe nystagmus, and have a clear understanding of its characteristics. Practice the smooth movement.
- Differentiating Nystagmus: Examiners frequently ask about differentiating peripheral from central nystagmus. Memorize the table and be ready to explain each feature with a clinical example.
- Caloric Test Interpretation: Understand the calculation for Canal Paresis and Directional Preponderance, and their clinical significance. Be prepared to explain COWS mnemonic.
- Safety First: In balance tests like Romberg’s and Gait test, emphasize standing close to the patient to prevent falls, as patient safety is paramount.
- “Why this test?”: For each test, be ready to explain its principle, what it measures, and why it’s clinically relevant. For example, “Why use VEMP when we have caloric tests?” (Answer: VEMP assesses otoliths and neural pathways, while caloric tests assess horizontal semicircular canals).
NEET PG Style Multiple Choice Questions (MCQs)
- Which of the following characteristics is most suggestive of peripheral nystagmus? a) Non-fatiguable with repeated testing b) Direction-changing with gaze c) Suppressed by optic fixation d) Associated with mild vertigo and other neurological signs
- A 45-year-old patient undergoes a caloric test. The results show a significant reduction in nystagmus duration from the right ear compared to the left, for both warm and cold irrigations. This finding is indicative of: a) Directional preponderance b) Bilateral vestibular failure c) Right canal paresis d) Central vestibular lesion
- The Dix-Hallpike manoeuvre is positive for left-beating nystagmus that starts after a 5-second latency and lasts for 30 seconds. This pattern is characteristic of: a) Meniere’s disease b) Acoustic neuroma c) Benign Paroxysmal Positional Vertigo (BPPV) d) Cerebellar ataxia
- Which clinical test specifically identifies an abnormal communication between the middle and inner ear, and can show a false positive result in Meniere’s disease? a) Romberg’s Test b) Dix-Hallpike Manoeuvre c) Fistula Test d) Unterberger Stepping Test
- In the Unterberger Stepping Test, a patient with a unilateral paralytic labyrinthitis will typically: a) Deviate to the healthy side b) Rotate towards the side of the lesion c) Fall straight backward d) Show no deviation
- Which of the following laboratory tests primarily assesses the function of the saccule and the inferior vestibular nerve? a) Optokinetic Test b) Ocular Vestibular Evoked Myogenic Potentials (oVEMPs) c) Cervical Vestibular Evoked Myogenic Potentials (cVEMPs) d) Rotational Test
- A patient reports severe vertigo and inability to stand without falling, even with eyes open. This finding on dynamic balance testing (e.g., Tandem Gait) most strongly suggests: a) Peripheral vestibular lesion b) Proprioceptive deficit c) Central vestibular lesion d) Psychogenic disorder
- The “COWS” mnemonic is used for which vestibular function test? a) Dix-Hallpike Maneuver b) Romberg’s Test c) Caloric Test d) Past-pointing Test
- Which parameter in Dix-Hallpike maneuver differentiates peripheral from central positional nystagmus by its disappearance on repeated testing? a) Latency b) Direction c) Duration d) Fatiguability
- A patient consistently overshoots towards the right side when performing the Past-pointing Test. This indicates a lesion on the: a) Left labyrinth b) Right labyrinth c) Cerebellum d) Brainstem
MCQ Answers and Explanations:
- c) Suppressed by optic fixation. Explanation: Peripheral nystagmus is typically suppressed when the patient fixates on a visual target, whereas central nystagmus is not. Non-fatiguable, direction-changing, and association with mild vertigo and other neurological signs are features of central nystagmus.
- c) Right canal paresis. Explanation: Canal paresis refers to a reduced response from one ear (the right ear in this case) on caloric testing, indicating weakness of that labyrinth or its nerve. Directional preponderance refers to nystagmus being stronger in one direction, regardless of the ear irrigated.
- c) Benign Paroxysmal Positional Vertigo (BPPV). Explanation: BPPV is characterized by a latent period (2-20 seconds), a limited duration (<1 minute), and fatigable nystagmus upon repeated Dix-Hallpike maneuvers.
- c) Fistula Test. Explanation: The fistula test checks for abnormal communication between the middle and inner ear. Hennebert’s sign (false positive fistula test) can be seen in Meniere’s disease due to fibrous bands or congenital syphilis.
- b) Rotate towards the side of the lesion. Explanation: In unilateral paralytic labyrinthitis, the patient will drift or rotate towards the side of the weaker labyrinth during the Unterberger Stepping Test.
- c) Cervical Vestibular Evoked Myogenic Potentials (cVEMPs). Explanation: cVEMPs specifically assess the saccule and the inferior vestibular nerve pathway. oVEMPs assess the utricle and superior vestibular nerve.
- c) Central vestibular lesion. Explanation: Severe instability, especially with eyes open, indicates a more profound balance deficit often seen in central lesions, as they disrupt multisensory integration more extensively than isolated peripheral lesions. Peripheral lesions usually cause more pronounced instability with eyes closed due to reliance on visual compensation.
- c) Caloric Test. Explanation: COWS (Cold Opposite, Warm Same) is a mnemonic used to remember the direction of the fast phase of nystagmus induced during the caloric test.
- d) Fatiguability. Explanation: Peripheral positional nystagmus (e.g., in BPPV) is fatiguable, meaning its intensity and duration decrease with repeated testing in the same position, whereas central nystagmus is non-fatiguable.
- b) Right labyrinth. Explanation: In the Past-pointing Test, patients with a vestibular lesion consistently past-point (overshoot) towards the side of the lesion. Therefore, right-sided past-pointing indicates a right labyrinthine lesion.
Clinical-Based Questions
1. Scenario: A 60-year-old male presents with sudden onset, severe spinning vertigo that lasts for approximately 30 seconds each time he turns his head to the right or lies down on his right side. He reports associated nausea but no hearing changes or tinnitus. The Dix-Hallpike maneuver is performed, and with his head turned to the right and hanging, there is a burst of upward and torsional nystagmus appearing after a 5-second delay, which then fades away after 25 seconds.
Questions:
- What is the most likely diagnosis?
- Explain the key Dix-Hallpike findings that support your diagnosis.
- What is the probable mechanism causing this condition?
- Briefly outline the most common treatment for this condition.
Answers:
- Most likely diagnosis: Benign Paroxysmal Positional Vertigo (BPPV), likely involving the right posterior semicircular canal.
- Key Dix-Hallpike findings: Latency: The 5-second delay before nystagmus onset. Short Duration: The nystagmus fading after 25 seconds (less than 1 minute). Direction: Upward and torsional nystagmus (characteristic of posterior canal BPPV). Provocation by specific head position: Symptoms triggered only when turning to the right or lying on the right side.
- Probable mechanism: Canalithiasis, where otoconia (calcium carbonate crystals) from the utricle become dislodged and migrate into the posterior semicircular canal. When the head is moved into a specific provocative position, these free-floating otoconia move within the endolymph, causing abnormal fluid displacement and stimulating the cupula, leading to vertigo and nystagmus.
- Most common treatment: Epley manoeuvre (Canalith Repositioning Procedure). This series of head movements aims to guide the dislodged otoconia out of the semicircular canal and back into the utricle.
Frequently Asked Questions (FAQs)
- Q: What are the main differences between peripheral and central vertigo? A: Peripheral vertigo is typically sudden, severe, episodic, associated with nausea/vomiting, and often accompanied by auditory symptoms, while central vertigo is usually insidious, milder, constant, and associated with other neurological signs but rarely auditory symptoms.
- Q: Why is the Dix-Hallpike maneuver important in diagnosing vertigo? A: The Dix-Hallpike maneuver is crucial because it is the gold-standard test to diagnose Benign Paroxysmal Positional Vertigo (BPPV), the most common cause of recurrent vertigo, by reproducing the patient’s symptoms and eliciting characteristic nystagmus.
- Q: How does the caloric test help distinguish between unilateral and bilateral vestibular hypofunction? A: The caloric test evaluates each ear separately; a significantly reduced response from one ear indicates unilateral hypofunction (canal paresis), whereas absent responses from both ears suggest bilateral hypofunction or a “dead labyrinth.”
- Q: What is the significance of “fatiguability” in nystagmus observed during vestibular testing? A: Fatiguability means the nystagmus and vertigo decrease or disappear with repeated testing in the same provocative position, which is a key distinguishing feature of peripheral vestibular lesions, particularly BPPV.
- Q: Can vestibular function tests be performed in children? A: Yes, many vestibular function tests can be adapted for children; for instance, rotational tests are generally better tolerated by children than caloric tests, which can be uncomfortable.
- Q: What is the role of VEMPs in evaluating dizziness? A: VEMPs specifically assess the function of the otolith organs (saccule and utricle) and their neural pathways, providing valuable information for diagnosing conditions like Meniere’s disease or superior canal dehiscence syndrome, which are not directly tested by caloric or rotational tests.
- Q: Why is it important to differentiate between peripheral and central causes of dizziness? A: Differentiating between peripheral and central causes is critical because central causes often indicate more serious neurological conditions (e.g., stroke, tumor) requiring urgent and distinct management compared to more benign peripheral vestibular disorders.
Download full PDF Link:
Vestibular Function Tests Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Vestibular function test, Balance assessment tests, Vestibular testing procedures, Dix-Hallpike manoeuvre, Electronystagmography (ENG), videonystagmography (VNG), Caloric stimulation test, Rotational chair testing, Vestibular evoked myogenic potentials (VEMP), Posturography, Corneal reflex (Blink reflex), Spontaneous Nystagmus, Fistula test, Romberg’s Test, Unterberger Stepping Test, Vestibular Function Tests, Nystagmus types, Caloric test interpretation, Dix-Hallpike maneuver, BPPV, Romberg test positive, Peripheral vs central vertigo, ENT viva questions vestibular, MBBS ENT notes balance, NEET PG ENT dizziness, Vestibular schwannoma diagnosis, Electronystagmography ENG, Videonystagmography VNG, Vestibular evoked myogenic potentials VEMP, Cerebellar function tests, Balance disorder diagnosis.Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests, Vestibular Function tests,
