Ossiculoplasty: Definition, Aim, and Surgical Reconstruction
Ossiculoplasty is the surgical reconstruction of the ossicular chain by using various autologous grafts and prostheses. The ossicles (malleus, incus, and stapes) are essential for transmitting sound from the tympanic membrane to the labyrinth. Discontinuity or fixation of the ossicular chain, whether congenital or acquired, leads to conductive hearing loss. Therefore, the primary goal of ossiculoplasty is to surgically re-establish this vital mechanical link and improve hearing.
Prerequisites for Ossicular Reconstruction
At the time of ossicular reconstruction, it is essential to ensure:
- The middle ear is healthy and free of active mucosal disease, infection and cholesteatoma.
- The Eustachian tube function is good. An atelectatic ear indicates poor function and predicts graft failure.
Timing of Ossicular Reconstruction
- Immediate (Primary) Reconstruction: This is performed during the initial surgery for conditions like traumatic ossicular disruption, isolated ossicular fixation, or during mastoidectomy surgery, if the surgeon is sure about the complete removal of the disease.
- Delayed (2nd Staged) Reconstruction: Traditionally, if the surgery is for cholesteatoma or active mucosal disease with the canal wall-up technique, ossiculoplasty will be delayed by 6 months. This staging allows confirmation of a disease-free middle ear at a second-look procedure, although single-stage reconstruction is increasingly common with advanced techniques and certainty of disease removal.
Materials for Reconstruction: Grafts and Prosthesis
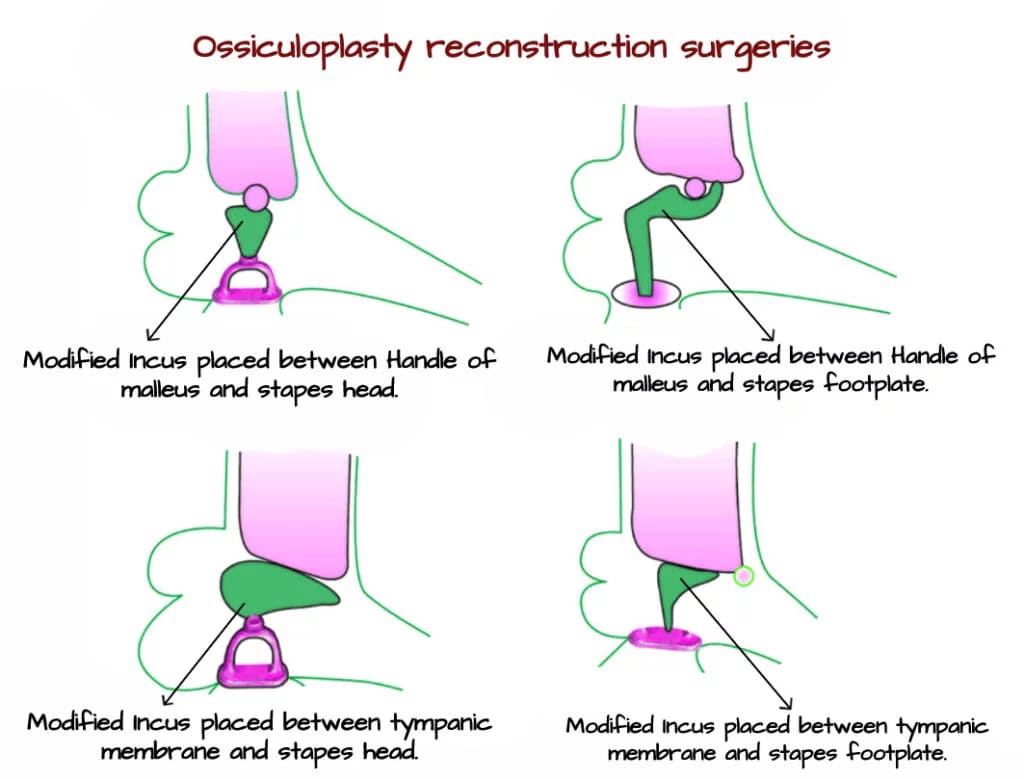
1. Autografts. Autografts are often the first choice due to excellent biocompatibility and no cost. Autograft ossicles can be sculpted to bridge the gap. Grafts commonly used for reconstruction are autologous incus, cortical bone and tragal cartilage. Autologous incus is commonly used as an autograft to reconstruct the ossicular chain. The most common defect of the ossicular chain is necrosis of the lenticular process; therefore incus is refashioned to be used as an autograft.
- Malleus-Stapes Assembly (MSA): The reshaped incus connects the malleus handle to the stapes head.
- Malleus-Footplate Assembly (MFA): It connects the malleus handle directly to the stapes footplate.
- Other Autografts: Cortical bone and tragal cartilage are also frequently used, especially for interposition or to shield a prosthesis.
Homograft-preserved ossicles with or without the tympanic membrane have been used, but they are difficult to procure and carry the risk of disease transmission.
2. Prostheses. Modern prostheses are designed to be durable, biocompatible, and easy to handle. Common materials include titanium (lightweight, excellent sound conduction), hydroxyapatite (biocompatible, integrates well), and gold/plastipore. A low-tension, short prosthesis provides better sound transmission and lower extrusion risk compared to a high-tension, long one.
- Partial ossicular replacement prosthesis (PORP): Used when the stapes superstructure is present and mobile, but the incus and/or malleus are defective. The PORP is placed between the tympanic membrane (or malleus) and the head of the stapes bone.
- Total ossicular replacement prosthesis (TORP): Used when the stapes superstructure is absent, leaving only a mobile footplate. The PORP is placed between the tympanic membrane (or malleus) and the footplate of the stapes bone.
Austin– Kartush Classification of Ossicular Defects
Austin– Kartush is the most accepted classification, which applies to situations without an intact incus. It helps to define pre-operative ossicular status to facilitate meaningful analysis of surgical outcomes. Austin proposed it in 1971 with four categories, and later it was modified by Kartush in 1994 with the addition of three further categories.

| TABLE: Modifications by Kartush | |
| Group | Ossicular status |
| O | Intact ossicular chain |
| E | Ossicular head fixation |
| F | Stapes fixation |
Kartush devised a Middle Ear Risk Index (MERI) which helps in the stratification of risk factors by giving a score of 0–16. It gives an idea preoperatively about successful outcome following surgery.
| TABLE: Middle Ear Risk Index 2001 | |
| Otologic factor | Maximum score |
| Otorrhoea | 3 |
| Perforation | 1 |
| Cholesteatoma | 2 |
| Ossicular status | 4 |
| Middle ear granulation | 2 |
| Previous surgery | 2 |
| Smoking | 2 |

TABLE: Surgical options to correct specific defects.
———— End of the chapter ————
High-Yield Points for Rapid Revision
- Most Common Ossicular Defect: Necrosis of the lenticular process of the incus.
- Gold Standard Autograft: Autologous incus, sculpted and repositioned.
- PORP vs. TORP: PORP = Stapes head present; TORP = Only footplate present.
- Key to Success: Aerated, disease-free middle ear with good Eustachian tube function.
- Best Prosthesis Characteristic: Low tension and short length.
- Staging: Ossiculoplasty is often staged (6 months later) in canal wall-up surgery for cholesteatoma.
- Primary Reconstruction Indications: Trauma, fixation, and dry canal wall-down cavities.
- Common Prosthesis Materials: Titanium and Hydroxyapatite.
- Critical Prerequisite: Absence of active infection/cholesteatoma.
- Major Complication: Prosthesis extrusion or displacement.
NEET PG & University Exam Style MCQs
- A 35-year-old male with chronic otitis media undergoes tympanomastoidectomy. Intraoperatively, the incus is necrosed but the malleus and stapes superstructure are intact. Which of the following is the most appropriate reconstruction? A. TORP B. PORP C. Malleus to footplate assembly D. Stapedotomy
- The Middle Ear Risk Index (MERI) includes all of the following factors EXCEPT: A. Presence of otorrhea B. Size of tympanic membrane perforation C. History of previous surgery D. Smoking status
- Which of the following is the MOST critical prerequisite for performing a successful ossiculoplasty? A. Profound sensorineural hearing loss B. A well-aerated and disease-free middle ear C. Absence of the malleus handle D. Prior myringoplasty
- A sculpted autologous incus is placed between the handle of the malleus and the head of the stapes. This is best described as: A. Stapedectomy B. Malleus to Footplate Assembly (MFA) C. Incus Interposition D. Malleus to Stapes Assembly (MSA)
- According to the Austin-Kartush classification, which group represents “Malleus absent, Stapes present”? A. Group A B. Group B C. Group C D. Group D
- Which material for ossicular prosthesis is known for its excellent biocompatibility and ability to integrate with bone? A. Plastic B. Titanium C. Stainless Steel D. Hydroxyapatite
- In a canal wall-up mastoidectomy for extensive cholesteatoma, the preferred timing for ossiculoplasty is usually: A. Simultaneous during the first surgery B. After 6 months in a second stage C. After 2 years D. Never attempted
- The most common site of defect in the ossicular chain in chronic otitis media is: A. Head of malleus B. Neck of stapes C. Lenticular process of incus D. Manubrium of malleus
- A prosthesis that connects the tympanic membrane directly to the stapes footplate is called a: A. PORP B. MSA C. TORP D. MFA
- Kartush’s addition to the Austin classification included all of the following EXCEPT: A. Ossicular chain intact (O) B. Malleus present (M) C. Ossicular head fixation (E) D. Stapes fixation (F)
Answers
- Answer: B. PORP.The presence of a mobile stapes superstructure indicates the need for a Partial Ossicular Replacement Prosthesis (PORP).
- Answer: B. Size of tympanic membrane perforation.MERI scores the presenceof a perforation (1 point), not its size.
- Answer: B. A well-aerated and disease-free middle ear.This is the foundational requirement for graft/prosthesis survival and function.
- Answer: D. Malleus to Stapes Assembly (MSA).This is the classic description of an incus interposition in the MSA configuration.
- Answer: C. Group C.
- Answer: D. Hydroxyapatite.It is a ceramic that is osteoconductive and integrates well with native bone.
- Answer: B. After 6 months in a second stage.This allows confirmation of a disease-free field before reconstruction.
- Answer: C. Lenticular process of incus.
- Answer: C. TORP.Total Ossicular Replacement Prosthesis is used when the stapes superstructure is missing.
- Answer: B. Malleus present (M).Kartush added groups O (intact), E (ossicular fixation), and F (stapes fixation).
Clinical Scenario-Based Viva Questions
Scenario 1: A 28-year-old patient presents with a history of right ear trauma following a slap. Otoscopy shows a healthy tympanic membrane. Audiometry reveals a 40 dB conductive hearing loss. Tympanometry is normal.
- Q1. What is the likely diagnosis?
- A1. Traumatic ossicular discontinuity (likely incudostapedial joint separation).
- Q2. What is the management?
- A2. Exploratory tympanotomy with ossiculoplasty. The ear is dry and healthy, so primary reconstruction can be performed. An autologous incus interposition or a PORP would be considered based on intraoperative findings.
Scenario 2: A 45-year-old diabetic, smoker with long-standing bilateral CSOM presents for hearing improvement. The left ear has been dry for 1 year with a large central perforation and a 50 dB conductive loss. CT shows sclerotic mastoid with no cholesteatoma.
- Q1. What factors in his MERI would you calculate?
- A1. Perforation (1), Previous surgery (0? needs clarification), Smoking (2). Otorrhea=0 (dry), Cholesteatoma=0, Ossicular status (unknown, assume worst-case C/D=4), Granulation=0. Score could range from 3 to 7+.
- Q2. What is your surgical plan?
- A2. First, perform myringoplasty to close the perforation and achieve a dry, stable ear. Ossiculoplasty may be staged due to the higher MERI score (smoking, possible ossicular defect) to ensure graft stability after tympanic membrane healing.
Scenario 3: During a surgery for inactive mucosal disease, you find the incus body eroded, the stapes superstructure absent, but a mobile footplate. The malleus handle is present.
- Q1. What Austin-Kartush class is this?
- A1. Class D (Malleus absent? Wait, handle is present. Review: Class B is “Malleus present, Stapes absent”. This is Class B).
- Q2. What prosthesis will you use?
- A2. Total Ossicular Replacement Prosthesis (TORP) placed between the malleus handle/tympanic membrane and the mobile footplate.
Frequently Asked Questions (FAQs) in Viva
- What is the main aim of ossiculoplasty? The main aim of ossiculoplasty is to surgically reconstruct the disrupted ossicular chain in the middle ear to restore the mechanical conduction of sound, thereby improving conductive hearing loss.
- What is the difference between PORP and TORP? A PORP (Partial Ossicular Replacement Prosthesis) is used when the stapes superstructure is present. A TORP (Total Ossicular Replacement Prosthesis) is used when the stapes superstructure is absent, and the prosthesis must reach the footplate.
- When is ossiculoplasty performed as a second-stage surgery? Ossiculoplasty is typically staged (done later) after a canal wall-up mastoidectomy for cholesteatoma or active infection, usually after 6 months, to ensure the middle ear is disease-free before reconstruction.
- What is the most common autograft used in ossiculoplasty? The most common and preferred autograft is the patient’s own incus bone, which is reshaped and repositioned to bridge the ossicular defect.
- What does a high Middle Ear Risk Index (MERI) score indicate? A high MERI score (above 5-6) indicates multiple unfavorable preoperative risk factors, which statistically predicts a lower chance of successful hearing improvement after ossiculoplasty.
- Can ossiculoplasty be done in a wet ear? No, ossiculoplasty should not be performed in an actively infected or draining (“wet”) ear. The ear must be dry and free of active disease to ensure graft/prosthesis survival and prevent complications.
- What is the most important factor for success in ossiculoplasty? The single most important factor is having a well-aerated, stable, and disease-free middle ear space with good Eustachian tube function.
———— End ————
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Master Ossiculoplasty for CBME, NEET PG & university exams, Definition, grafts, prosthesis, Austin-Kartush classification, MERI, Ossiculoplasty definition, Ossiculoplasty aim, Ossiculoplasty grafts, Ossiculoplasty prosthesis, PORP vs TORP, Austin Kartush classification, Middle Ear Risk Index MERI, Ossicular chain reconstruction, Conductive hearing loss surgery, Ossiculoplasty MCQs, Ossiculoplasty high yield notes, Ossiculoplasty CBME notes, ENT PG exam preparation, NEET PG ENT questions, Ossiculoplasty mnemonics, Ossiculoplasty viva questions, Ossiculoplasty clinical cases, Autologous incus graft, Titanium prosthesis ossiculoplasty, Staged ossiculoplasty, Cholesteatoma and ossiculoplasty, Prerequisites for ossiculoplasty, Complications of ossiculoplasty, Hearing after ossiculoplasty, High-yield points, MCQs, clinical cases, FAQs, and mnemonics

