|
The following CBME core competencies are covered in this chapter.
|
Eustachian Tube Anatomy
The eustachian tube is named after Bartolomeo Eustachius (1520-74 AD). The eustachian tube (pharyngotympanic tube) is a dynamic, trumpet-shaped, mucosa-lined channel that connects the middle ear cavity to the nasopharynx.

Functions of Eustachian tube
Eustachian tube usually remains closed. It opens during swallowing, yawning and sneezing. It plays a key role in middle ear function. It provides ventilation, protection and drainage of the middle ear.
- Ventilation. It acts as a ventilatory channel, regulates equilibrium between middle ear pressure and atmospheric pressure.
- Protection. It protects middle ear against reflux of nasopharyngeal secretions, sound pressure and organisms from the pharynx.
- Drainage. It drains (clearance of) middle ear secretions toward the nasopharynx by the mucociliary system.
Basic Dimensions & Orientation
- Length: 36 mm in an adult (range: 31-38 mm) and 13–18 mm at birth. This adult length is attained by age 7. While in infants and young children, the tube is shorter, wider, more horizontal and less efficient. Hence eustachian tube dysfunction is commonly seen in infants and young children.
- Course: It runs downwards, forwards, and medially from the middle ear to the nasopharynx.
- Angle: Forms a 45° angle with the horizontal plane in adults. And 10° angle in infants.
Parts of the Eustachian Tube
The tube has two parts (bony and cartilaginous), and it is reverse of what is present in the external auditory canal.
- The lateral, Bony part, which is upper, posterolateral one-third (12 mm) and begins from the anterior wall of the tympanic cavity (protymanum). The bony tympanic end is an oval-shaped opening, measures 5 × 2 mm and it is located in the anterior wall of the middle ear, a little above the level of the floor. It is lined with a thin layer of cuboidal respiratory epithelium.
- The medial, Cartilaginous part, which is lower, anteromedial two-thirds (24 mm) and opens at the lateral wall of the nasopharynx. The fibrocartilaginous part of the tube is made of a single piece of cartilage folded upon itself in such a way that it forms the whole of the medial lamina, roof and a part of the lateral lamina; the rest of its lateral lamina is made of the fibrous membrane.
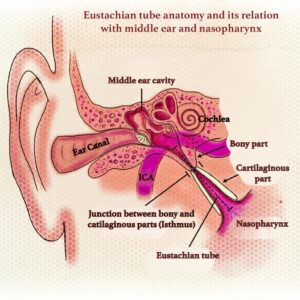
Key Anatomical Landmarks
- Isthmus: Both bony and fibrocartilaginous parts meet at the isthmus, which is the narrowest part (diameter is 0.5mm or less) of the tube. It is lined by respiratory epithelium similar to epithelium present in the nasopharynx.
- Torus Tubarius: The cartilage at the pharyngeal end raises an inverted ‘J’ shaped elevation called torus tubarius which is located 1–1.25cm behind and a little below the posterior end of the inferior turbinate.
- Fossa of Rosenmüller: Behind the torus tubarius is a recess called the fossa of Rosenmüller, which is the common site for nasopharyngeal malignancy.
- Tubal Tonsil (of Gerlach): Above the torus tubaris is the lymphoid tissue, known as the tubal tonsil (of Geralch). During childhood, tubal tonsils are present around the tubal elevation, hypertrophy of which causes eustachian tube obstruction.

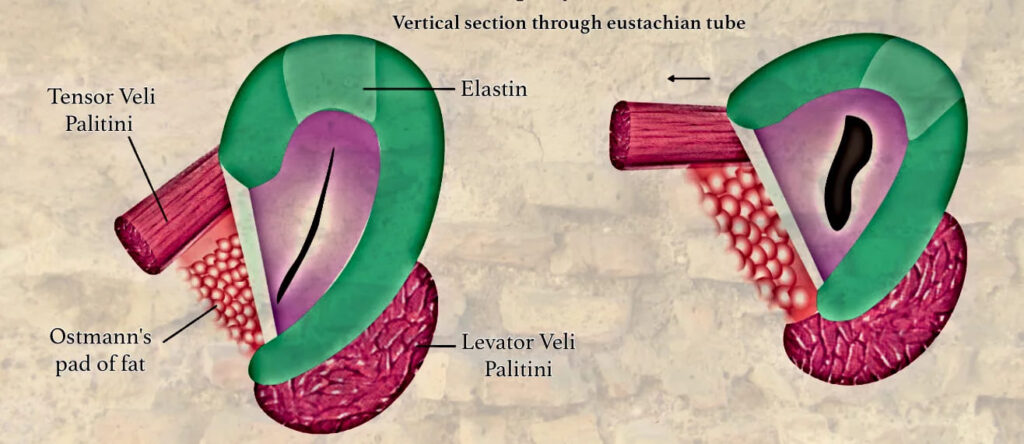
Eustachian Tube Dynamic “Valve” Mechanism
The cartilaginous tube is normally closed at rest. It opens transiently during swallowing, yawning, or sneezing. The closure is maintained by:
- Intrinsic Elastic Recoil: The “Elastin Hinge” – It is a zone, rich in elastin fibres and is situated in the roof at the junction of the medial and lateral lamina. By its recoil, it keeps the tube closed when the dilator muscle of ET (tensor veli palatini) is not in action.
- Extrinsic Tissue Pressure: Ostmann’s Pad of Fat – It is a mass of fatty tissue located in the inferolateral aspect of the eustachian tube that most likely aids in closing the tube. Therefore, it protects the middle ear from the retrograde flow of nasopharyngeal secretions. Ostmann’s fat pad decreases in volume with an increase in age, leading to a patulous eustachian tube.
Muscles of the Eustachian Tube System
These muscles are the “motors” that actively open the tube.
|
Muscle |
Primary Action |
Origin |
Insertion |
Nerve Supply |
Role in ET Function |
|
Tensor Veli Palatini (TVP) |
Primary dilator of ET |
Scaphoid fossa of medial pterygoid plate, cartilage of ET, spine of sphenoid. |
Forms palatine aponeurosis (soft palate). |
Mandibular Nerve (V3) via medial pterygoid branch. |
Contraction pulls the lateral lamina (fibrous membrane) downwards and laterally, opening the lumen like a pulley. Most important for active opening. |
|
Levator Veli Palatini (LVP) |
Elevates soft palate |
Petrous apex, inferior surface of ET cartilage. |
Soft palate (blends with contralateral muscle). |
Pharyngeal Plexus (Cranial Nerves IX, X, XI). |
Elevates the medial cartilaginous lamina and rotates the torus tubarius medially, aiding in opening. Its action is more palatal than tubal. |
|
Salpingopharyngeus |
Elevates pharynx |
Inferior part of cartilaginous ET. |
Blends with palatopharyngeus in pharyngeal wall. |
Pharyngeal Plexus (IX, X). |
Minor role. May help stabilize/ open the pharyngeal end. |
|
Tensor Tympani |
Dampens loud sounds (acoustic reflex) |
Bony canal above ET, cartilaginous ET. |
Neck of Malleus. |
Mandibular Nerve (V3). |
Not a direct dilator. Its connection suggests a role in middle ear pressure regulation during ET opening. |
During activities like swallowing or yawning, the simultaneous contraction of the Tensor veli palatini and Levator veli palatini allows air to pass through the ET, equalizing middle ear pressure with atmospheric pressure. The tube closes passively due to the elastic recoil of the elastin hinge cartilage and deformation of Ostmann’s fat pad. Dysfunction of these muscles, as seen in conditions like cleft palate or neuromuscular disorders, can lead to Eustachian tube dysfunction (ETD), causing symptoms such as ear fullness, hearing loss, and recurrent otitis media. Proper functioning of these muscles is essential for maintaining middle ear pressure, particularly during altitude changes or upper respiratory infections.
Vascular Supply
- Arterial Supply: Ascending pharyngeal artery (main), middle meningeal artery, artery of pterygoid canal.
- Venous Drainage: Pterygoid venous plexus.
- Lymphatic Drainage: Retropharyngeal and deep cervical nodes.
Differences between the Infant and Adult Eustachian Tube
In infants, the size of ET is about half as compared to the size normally seen in an adult; it averages about 18 mm and reaches adult size by 7 years of age. In infants direction of the tube is also different; it is 10 degrees to the horizontal as compared to 45 degrees in adults. As the eustachian tube of infants is wider, shorter and more horizontal, all the protective functions of ET system are less efficient. Even the milk goes into the middle ear if the infants are not fed in a head-up position. Nasopharyngeal secretions can enter more readily into the middle ear and result in middle-ear infection.
| Infant | Adult | |
| Length | 13–18 mm at birth (about half as long as in adult) | 36 mm (31–38 mm) |
| Direction | More horizontal. Forms an angle of 10° with the horizontal. | Forms an angle of 45° with the horizontal |
| Angulation at isthmus | No angulation | Angulation present |
| Bony versus cartilaginous part | Bony part is slightly longer than one-third of the total length of the tube and is relatively wider | Bony part one-third; cartilaginous part two-thirds |
| Tubal cartilage | Flaccid. Retrograde reflux of nasopharyngeal secretions can occur | Comparatively rigid. Remains closed and protects the middle ear from the reflux |
| Density of elastin at the hinge | Less dense; tube does not efficiently close by recoil | Density of elastin more and helps to keep the tube closed by recoil of cartilage |
| Ostmann’s pad of fat | Less in volume | Large and helps to keep the tube closed |
———— End of the chapter ————
Download full PDF Link:
Eustachian Tube Anatomy Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Eustachian tube anatomy, Pharyngotympanic tube structure, Eustachian tube function, Eustachian tube parts, Eustachian tube location, Eustachian tube histology, Eustachian tube embryology, Eustachian tube dysfunction, Understanding the Anatomy and Function of the Eustachian Tube, A Comprehensive Guide to the Structure of the Pharyngotympanic Tube, Exploring the Components and Location of the Eustachian Tube, The Role of the Eustachian Tube in Middle Ear Health, Anatomical Insights into Eustachian Tube Dysfunction, Bony and cartilaginous parts, Ostman pad of fat, Isthmus, Difference between young and adult eustachian tube, Eustachian Tube Anatomy
