Septoplasty
Septoplasty is a foundational procedure in Otorhinolaryngology, routinely performed to restore normal nasal breathing. Mastering its surgical principles, anatomy, and indications is essential for all ENT students preparing for the CBME curriculum, university theory exams, and competitive NEET PG MCQs.
Anatomy of the Nasal Septum
The nasal septum divides the nasal cavity into two halves and plays a vital role in airflow dynamics and structural support of the external nose. Consequently, any significant deviation can severely impair breathing efficiency.

Parts of the Nasal Septum.
The septum has three main anatomical divisions:
- Columellar Septum: This is the most caudal part, formed by the medial crura of the alar cartilages united by fibrous tissue and covered by skin. It is freely movable.
- Membranous Septum: Located between the columella and the caudal edge of the septal cartilage, this segment is composed of double skin layers and lacks bony or cartilaginous support. It is also freely movable.
- Septum Proper (Osteocartilaginous Framework): This is the rigid, main part of the septum, covered by the nasal mucosa (mucoperichondrium and mucoperiosteum).
The rigid framework is composed of:
- Cartilage: Septal (Quadrilateral) Cartilage (largest anterior component).
- Bones: Perpendicular Plate of Ethmoid (PPE) (postero-superior), Vomer (postero-inferior), and minor contributions from the Maxillary and Palatine crests.
Why Nasal Septum Deviation Occur?
A septal deviation can occur for two main reasons.
- The septal cartilage itself may have a natural bend.
- The cartilage may look bent because the bony part of the septum is tilted.
If the cartilage is straight but the bone is tilted, correcting the bony attachment usually fixes the deviation. If the cartilage itself is bent, surgeons use special techniques to straighten it. When a deviated septum also causes an external nasal deformity, the patient may need an additional procedure to correct the outside shape of the nose. This combined surgery is called rhinoplasty.
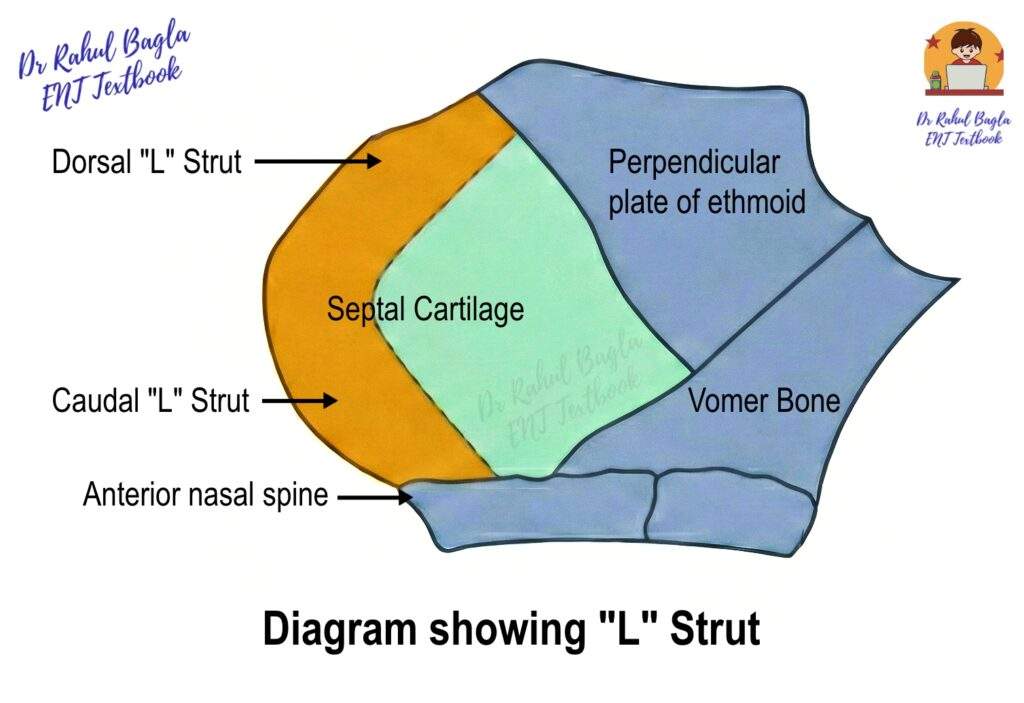
The Essential L-Strut (Caudal and Dorsal Strut)
For structural integrity and support, a critical L-shaped strut of cartilage and bone must be preserved during septal surgery; therefore, this strut is vital for supporting the external nasal skeleton.
- What is L-strut? : The L-strut comprises the dorsal (superior) margin and the caudal (anterior/inferior) margin of the septal cartilage, thus providing the nose’s shape and tip support.
- Safety Margin: At least preserve at least 1 cm of the L-strut’s width during surgery.
- Clinical Significance: Damage to the L-strut can lead to severe cosmetic and functional defects: Saddle Nose Deformity (dorsal collapse) or supratip depression (caudal collapse).
Nasal Obstruction: Differential Diagnosis
Nasal obstruction is a common patient complaint, and while a deviated nasal septum (DNS) is a major cause, clinicians must consider other factors (nasal valve and mucosal elements) in order to have patient satisfaction following septal surgery. Consequently, a systematic approach is necessary for accurate diagnosis.
- Anatomical – It is mainly caused by anatomical obstruction g., DNS, polyp, choanal atresia. Nasal obstruction is usually constant with minimal or no improvement in response to decongestants.
- Mucosal Obstruction – It is mainly caused by Mucosal Blockage (e.g., Allergic/Vasomotor Rhinitis, Infection, Sinusitis). Nasal obstruction is usually intermittent with significant improvement in response to decongestants.
- The Nasal Valve – The Nasal Valve is the narrowest part of the nasal airway, providing up to 50% of total airway resistance; therefore, its collapse significantly contributes to obstruction.
Diagnosis and Examination
- Anterior Rhinoscopy: Map the deviation relative to the L-strut.
- Nasendoscopy (Diagnostic Endoscopy): Essential for visualizing posterior deviations, adenoids, and choanae not visible on rhinoscopy.
- Palpation: Use a Jobson-Horne probe to check consistency (bone vs. cartilage) and identify spurs.
- Cottle’s Test: Pull the cheek laterally. Improvement in breathing suggests nasal valve collapse.
Viva Tip: An examiner will likely ask you to perform Cottle’s test and distinguish between mucosal and anatomical obstruction. Always mention the role of nasendoscopy in modern assessment.
Surgical Management: Septoplasty vs. SMR
The goal of septal surgery is to straighten the septum and re-establish the nasal airway while preserving the crucial L-strut.
Submucosal Resection (SMR)
- Principle: Excision of the deviated bone/cartilage.
- Indication: Only for deviations NOT involving the dorsal or caudal L-strut (e.g., posterior bony spurs, high septal deviation).
- Incision: Killian incision is placed 1 cm cephalad (behind) from the caudal margin of the septum. It provide excellent exposure of the septum proper and perichondrium is less adherent to the underlying cartilage and the flap can be raised more easily. If the deviation is situated further cephalad, the incision for access can be made close to the offending segment (Modified Killian’s Incision). Next the perichondrium of the underlying cartilage is elevated. The deviated part of the septum is freed from its peripheral cartilaginous and bony attachments on both sides and removed.
Indications: The present days indication of SMR are:
- Transnasal hypophysectomy
- Septal cartilage graft.
Complications of SMR
- Columellar retraction
- Supratip depression
- Flappy septum
- Septal hematoma.
Limitation: It cannot address L-strut deviations, and excessive excision risks septal perforation and collapse.
Septoplasty
- Principle: Reconstruction and repositioning of the septum, prioritizing preservation of the L-strut. It is a more conservative procedure than SMR where only deviated portion of the nasal septum is removed.
- Indication: Most cases of septal deviation, particularly those involving the L-strut (caudal and dorsal deviations).
- Incision: Hemitransfixion (or Freer’s) incision along the caudal edge of the septal cartilage, usually unilateral. It provides excellent exposure of caudal L-strut and septum proper. Hemitransfixion can be partial, complete or extended, depending upon exposure required. If access is required to the whole of caudal arm of the L-strut then a full hemitransfixion is used. However, if access is not required for the most posterior parts of the septum, then a partial hemitransfixion would suffice. If access is required to the floor of the nasal cavity then an extended hemitransfixion incision is used.
- Approach: Provides access to the whole septum, including the L-strut, which is typically avoided in SMR. Therefore, septoplasty is the procedure of choice for most modern septal corrections.
Indications of Septoplasty
- Nasal Obstruction: A deviated septum narrows the airway and causes unilateral or bilateral nasal blockage.
- Septorhinoplasty Component: Surgeons perform septoplasty as part of septorhinoplasty to improve both function and cosmetic nasal shape.
- Recurrent Epistaxis: Septal spurs repeatedly traumatize the mucosa and trigger anterior nosebleeds.
- Recurrent or Chronic Sinusitis: A deviated septum impairs ventilation and drainage of sinuses, contributing to persistent sinus infections.
- Contact Point Headache: A deviated septum touches the lateral nasal wall, especially the middle turbinate, and triggers rhinogenic headaches.
- Endoscopic Sinus Surgery (ESS) Access: Surgeons correct the septum when its deviation limits visualization or access to the middle meatus or frontal recess.
- Endoscopic Dacryocystorhinostomy (DCR): Correction is needed when septal deviation obstructs the surgical corridor to the lacrimal sac.
- Trans-septal Transsphenoidal Approach: Surgeons straighten the septum to gain access to the sphenoid sinus and the pituitary fossa.
- Sleep-Disordered Breathing: Deviated septum contributes to snoring, obstructive sleep apnoea (OSA), or hypopnoea syndrome, warranting correction.
Contraindications of Septoplasty
- Acute Nasal or Sinus Infection: Infection increases bleeding, crusting, and postoperative complications.
- Uncontrolled or Untreated Diabetes Mellitus: Poor glycaemic control impairs wound healing and raises infection risk.
- Uncontrolled Hypertension: High blood pressure increases intraoperative and postoperative bleeding.
- Bleeding Diathesis: Coagulopathies increase operative bleeding risk; correction or optimization is essential before surgery.
Septoplasty – Steps of Surgery:
- Patient Position: Place the patient in the Reverse Trendelenburg position (head elevate at 15 degrees). This is done to reduce bleeding by promoting venous drainage and consequently improving the surgeon’s visibility.
- Anaesthesia and Haemostasis: Achieve local anaesthesia and vasoconstriction by injecting 2% Lignocaine with Adrenaline (1:50,000). Inject the solution in the subperichondrial plane to induce hydrodissection, which helps the flap lift more easily and separates the perichondrium from the cartilage.
- Incision is made: A Hemitransfixion incision is made along the caudal edge of the septal cartilage.
- Raising Mucoperichondrial/periosteal Flaps: Caudally, the perichondrium is more adherent to the septal cartilage at the caudal side as compared to the cephalic side. Hence, it is comparatively easy to elevate the flap on the cephalic side as compared to the caudal side. Therefore, always raise the flap in the subperichondrial/ subperiosteal plane (just deep to the perichondrium/periosteum) to minimise bleeding and maintain flap viability.
- Unilateral Flap Elevation: Generally, the flap is raised on the concave side first. It provides more space for instrumentation. It also allows easy access for excision of deviated septal cartilage or bone. It also preserves the opposing side’s mucosa, significantly reducing the risk of septal perforation.
- Bilateral Flap Elevation: It is usually done when there is a S-shaped deviation or when you need to apply a mattress suture or harvest large posterior bony grafts (e.g., perpendicular plate of ethmoid), where access to both sides of the septum is required.
- Disarticulation of bony-cartilaginous junction: The bony-cartilaginous junction is disarticulated to reach the other side of the bony septum. Care is taken not to tear the opposite mucosa. Sometimes this separation is not enough to straighten the septum, so a thin piece of bone or cartilage is removed (preferably in one piece for graft use). The quadrilateral cartilage is also freed from the maxillary crest, and again, a small sliver may need to be removed to bring the septum back to the midline.
- Removal of deviation and realignment of septum: Septoplasty focuses on reconstruction rather than simple excision, hence only the most deviated part of the septum is removed, and the rest of the septum is brought in midline. It can be done by multiple techniques.
-
- Cutting Techniques (Scoring): Scoring involves making partial-thickness cuts on the concave side of the cartilage. This weakens the intrinsic spring of the cartilage, allowing it to straighten out. Used for cartilaginous bends (C-shaped or S-shaped).
- Swinging Door Technique: Used for caudal septal deviation/dislocation. Excise a minimal, appropriate amount of cartilage from the caudal arm of the L-strut, then reposition the remaining L-strut. Secure it to the Anterior Nasal Spine (ANS) using 4-0 PDS sutures.
- Grafting techniques: A straight, firm piece of septal cartilage or Perpendicular Plate of Ethmoid bone (called a batten graft) is placed on the concave side of a bent or weakened septum to keep it straight. This makes the correction more stable than scoring alone. The graft is shaped, thinned, and perforated. It is then sewn to the septum using fine sutures (e.g., 5-0 PDS) to support the straightened septum and prevent recurrence of deviation.
- Mattress Suture technique: Used to control septal curvature. After scoring the cartilage to make it pliable, fine, non-absorbable sutures (e.g., 5-0 Prolene) are placed and incrementally tightened until the desired shape is achieved. Requires bilateral flap elevation to cover the suture knots.
- Relocating Techniques: These techniques are used when the septum is shifted off the midline but can be corrected simply by putting it back in place. Dislocated septal cartilage can be replaced in the maxillary groove or on the anterior nasal spine by excision of the cartilage along the floor of nose and fixing it with a suture.
- Suturing: Trans-septal mattress sutures are placed to coapt mucoperichondrial flaps tightly. This is the most crucial step for preventing the formation of a septal haematoma.
- Packing: Packing is done in both nasal cavities to prevent collection of blood between the flaps and to support the straightened septum. Ribbon gauze coated with antibiotic ointment or liquid paraffin is commonly used. Other options include Merocel or silicone splints. Packing is usually kept for 24–48 hours to keep the mucoperichondrial flaps together and maintain septal alignment. A nasal dressing is applied externally.
Important Considerations in Septoplasty:
- Managing a Septal Spur (Maxillary Crest). Raising a flap over a sharp bony spur is challenging and prone to tears. Therefore, employ special techniques:
-
- Back-to-Front (Cephalad to Caudal): Raise the flap over the cartilage first, then dissect the posterior flap from cephalad (top) to caudal (bottom), dissecting toward the spur’s peak (less adherent area).
- Front-to-Back (Tunnel Technique): Create an anterior tunnel (over the quadrilateral cartilage) and a posterior tunnel (posterior to the spur). This leaves the mucosa attached only at the spur’s peak, consequently allowing for safe, sharp dissection through the highly adherent mucoperiosteum at the crest.
- Management when the floor of the nasal cavity exposure is required. If access is required to the floor of the nasal cavity, then an extended hemitransfixion is applied. This would allow raising a tunnel underneath the septal spur, which reduces the chance of mucosal tear over the spur. Raising the flap over a spetal spur can be challenging as the perichondrial fibres of the cartilaginous septum and the periosteal fibres of the maxillary crest are interwoven. To reduce the chance of mucosal tear, two techniques can be employed.
Postoperative Care
- Septal surgery is a day care surgery and the patient can go home after he fully recovers from effects of sedation with no postoperative nausea or bleeding. Patients with obstructive sleep apnoea should better be observed overnight.
- Avoid strenuous exercise as it may cause bleeding.
- Pack, if kept is removed the next day and patient be instructed not to blow the nose or sneeze hard. Secretions can be drawn backwards into the throat by snorting rather than blowing the nose.
- Saline spray or steam inhalation are encouraged after pack removal.
- Xylo- or oxymetazoline drops are used if nose becomes stuffy.
- Nasal splints, if used, are removed on fourth to eighth day and gentle suction of nose is done.
- Patient should avoid trauma to nose, wipe the nose gently and in no case push the nose from one side to another.
Complications
- Bleeding. It may require repacking if severe.
- Septal haematoma. Evacuate the haematoma and give intranasal packing on both sides of the septum for equal pressure.
- Septal abscess. This can follow infection of septal haematoma.
- Perforation. When tears occur on the opposing side of the mucous membrane.
- Depression of the bridge. Usually occurs in the supratip area due to too much removal of cartilage along the dorsal border.
- Retraction of the columella. Often seen when the caudal strip of cartilage is not preserved.
- Persistence of deviation. It usually occurs due to inadequate surgery and may require a revision operation.
- Flapping of the nasal septum. Rarely seen, when too much of the septal framework has been removed. The septum, which now consists of two mucoperichondrial flaps, moves to the right or left with respiration.
- Toxic shock syndrome. It is rare after septal surgery. It can follow staphylococcal (sometimes streptococcal) infection and is characterised by nausea, vomiting, purulent secretions, hypotension and rash. It should be diagnosed early. It is treated by removal of packing, hydrating the patient, maintaining blood pressure and administering proper antibiotics.
Special Septoplasty Considerations
There are special cases related to septoplasty that deserve to be discussed separately.
1. Endoscopic Septoplasty.
This technique uses a nasal endoscope to improve visualisation, especially for high (cephalic) septal deformities. It allows minimal-access dissection, targeting isolated deviated areas, making it useful for revision surgeries. It can be performed along with sinus surgery. It serves as an excellent teaching tool because it clearly shows the nasal anatomy to trainees.
2. Paediatric Septoplasty.
Earlier, surgeons avoided septoplasty before 17 years, but new evidence says it is safe even at 6 years. Delaying surgery can worsen nasal obstruction and affect nasal and facial growth. The principle of Paediatric Septoplasty is to minimise resection, maximise re-implantation and to avoid disrupting the endochondral ossification plates if possible. Any removed cartilage should be reshaped and put back to support normal growth.
3. External Approach Septoplasty.
This technique is usually reserved for cases where the dorsal L-strut deformity prevents endonasal access. It provides better surgical exposure for complex septal reconstructions. Often performed as external septorhinoplasty, particularly for extracorporeal septoplasty in severely deformed or fractured septa.
4. Extracorporeal Septoplasty (External Approach Septoplasty).
It is indicated in severely fractured or deformed septa (e.g., severe trauma, revision surgery) that cannot be straightened in situ. In this method, both cartilaginous and the bony segment are excised in one piece as intact as possible (removed from the body). The new septum is then reconstructed outside the nose (extracorporeally) by cutting, reshaping, or splinting the pieces together (often using a batten graft or a PDS sheet as a backing). The neo-septum is reinserted and secured to the anterior nasal spine, maxillary crest, and upper lateral cartilages. It is almost always performed via an external septorhinoplasty approach for maximal visualisation and access.
———— End of the Chapter ————
Download the full PDF Link:
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Cummings, Otolaryngology-Head and Neck Surgery.
- Stell and Maran’s, Textbook of Head and Neck Surgery and Oncology.
- Ballenger’s, Otorhinolaryngology Head And Neck Surgery
- Susan Standring, Gray’s Anatomy.
- Frank H. Netter, Atlas of Human Anatomy.
- B.D. Chaurasiya, Human Anatomy.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery.
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Ganong’s Review of Medical Physiology.
- Guyton & Hall Textbook of Medical Physiology.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page:https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Juvenile Angiofibroma. https://www.entlecture.com/juvenile-angiofibroma/
- Please read. Tumours of Hypopharynx . https://www.entlecture.com/tumours-of-the-hypopharynx/
- Please read. Anatomy of Oesophagus. https://www.entlecture.com/anatomy-of-oesophagus/
Keywords: Septoplasty, deviated nasal septum, DNS surgery, nasal septum surgery, septal deviation treatment, septoplasty indications, septoplasty steps, septoplasty complications, submucous resection, SMR vs septoplasty, endoscopic septoplasty, nasal septum anatomy, causes of deviated septum, L-strut septum, caudal septal deviation, dorsal septal deviation, septoplasty incision types, hemitransfixion incision, Killian incision, mucoperichondrial flap elevation, cartilaginous septum deviation, bony septum deviation, septoplasty postoperative care, septoplasty contraindications, septal spur management, maxillary crest spur, extracorporeal septoplasty, pediatric septoplasty, functional septorhinoplasty, nasal valve collapse, Cottle test, septoplasty vs rhinoplasty, nasal obstruction differential diagnosis, septal hematoma management, septoplasty packing types, Merocel packing, ribbon gauze packing, what is septoplasty surgery for DNS, how is septoplasty done step by step, is septoplasty necessary, difference between SMR and septoplasty, best technique for caudal septal deviation, how to identify L-strut in septoplasty, why preserve 1 cm L-strut, how to manage septal spur, which incision is best for septoplasty, how to perform a hemitransfixion incision, DNS vs turbinate hypertrophy, does septoplasty improve snoring, septoplasty recovery time, indications for endoscopic septoplasty, when to do extracorporeal septoplasty, can septoplasty be done in children, how to avoid mucosal tears, exam-oriented steps of septoplasty, caudal septal dislocation treatment, why septoplasty fails, NEET PG septoplasty questions, nasal septum anatomy NEET PG, L-strut questions ENT exam, DNS classification MBBS, Cottle test NEET PG, SMR complications NEET PG, septoplasty vs SMR MCQs, steps of septoplasty MBBS notes, management of septal spur MBBS, DNS with nasal valve collapse MCQ, mucoperichondrial flap anatomy MCQ, pediatric septoplasty indications exam, extracorporeal septoplasty MCQ, septal hematoma exam question, septoplasty complications MCQ, nasal airflow resistance, nasal valve area, mucoperichondrium, mucoperiosteum, septal cartilage scoring, batten graft septoplasty, PDS sutures septoplasty, anterior nasal spine fixation, maxillary crest deviation, septal dislocation, rhinogenic headache, septal perforation risk, saddle nose deformity, supratip depression, endonasal approach, functional nasal surgery, rhinoplasty combined procedures, septal reconstruction, anatomy of nasal septum MBBS, septoplasty for ENT trainees, simplified septoplasty notes, high-yield septoplasty notes, deviated nasal septum surgical correction, ENT practical viva septoplasty, DNS with nasal valve collapse, common errors during septoplasty, how to avoid septal perforation in surgery, nasal septum parts, quadrilateral cartilage, vomer bone, perpendicular plate of ethmoid, nasal endoscopy DNS findings, mucosal vs anatomical obstruction, nasal airway physiology, steps of mucoperichondrial flap elevation, reverse trendelenburg ENT surgery.
