Adenoidectomy
Adenoidectomy, the surgical removal of the adenoids, is one of the most frequently performed pediatric surgeries. This procedure can be performed alone, in combination with tonsillectomy (adenotonsillectomy), or with myringotomy and grommet insertion to treat otitis media with effusion. When combined with tonsillectomy, the adenoids are removed first, and the nasopharynx is packed before the tonsillectomy begins. Despite its disadvantages, such as unpredictable bleeding, poor access to choanal adenoids causing recurrence, and potential injury to the eustachian tube opening, the blind curettage method remains the most commonly used adenoidectomy method. While the traditional blind curettage method remains common, newer endoscopic techniques are gaining popularity due to improved visualisation and precision.
Preoperative Assessment:
- Investigations for surgical fitness: Hemogram, urine analysis (routine and microscopic), blood sugar (fasting), blood urea/creatinine, chest X-ray, ECG.
- Coagulation Profile: Prothrombin time, partial thromboplastin time, bleeding time, clotting time and platelet count.
- X-ray of the Nasopharynx (Lateral View with Open Mouth): To assess the size of the adenoids and the extent of nasopharyngeal air space compromise.
- Nasal Endoscopy: Useful for assessing adenoid size in cooperative children and is considered the gold standard for diagnosis.
- Children with Down Syndrome: Assess for potential atlantoaxial instability (subluxation of the first and second cervical vertebrae) and cardiac abnormalities.
Indications for Adenoidectomy:
- Adenoid Hypertrophy: Causing snoring, mouth breathing, obstructive sleep apnea syndrome, craniofacial growth abnormalities (adenoid facies), or speech abnormalities (e.g., rhinolalia clausa).
- Chronic Otitis Media with Effusion: Due to anatomical obstruction of the eustachian tube.
- Recurrent Acute Otitis Media: Associated with adenoiditis or adenoid hyperplasia.
- Dental Malocclusion: Adenoidectomy does not correct dental abnormalities but prevents recurrence after orthodontic treatment.
- Recurrent Rhinosinusitis
Contraindications for Adenoidectomy:
- Cleft Palate or Submucous Palate: Removal of adenoids causes velopharyngeal insufficiency, causing a hypernasal voice (rhinolalia aperta) and regurgitation of food.
- Acute Infection of the Upper Respiratory Tract: Surgery during an active infection can increase the risk of bleeding, anaesthetic complications, and post-operative infections.
- Haemorrhagic Diathesis.
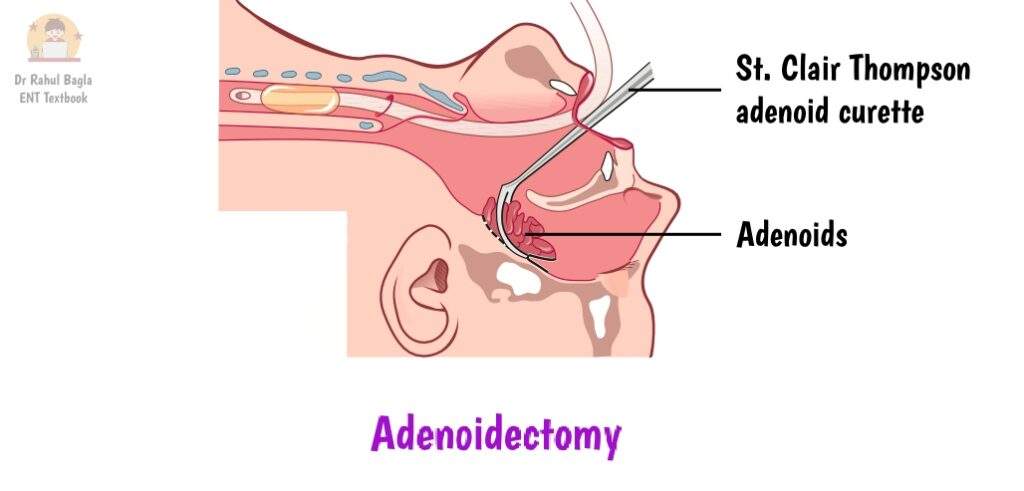
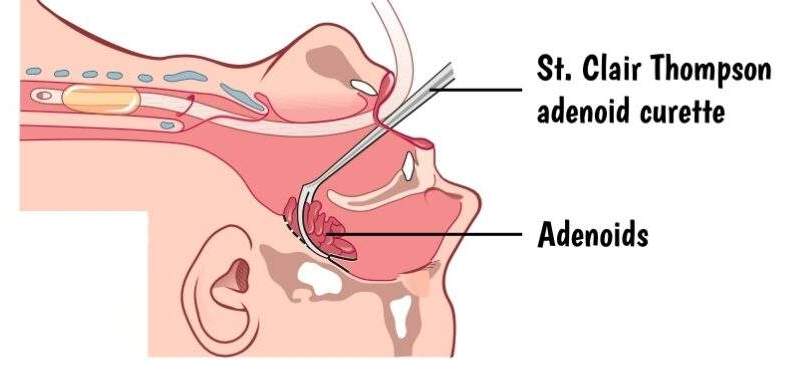
Surgical Steps: Traditional Adenoidectomy (Blind Curettage)
1. Anaesthesia: Usually performed under general anaesthesia with endotracheal intubation, providing a secure airway.
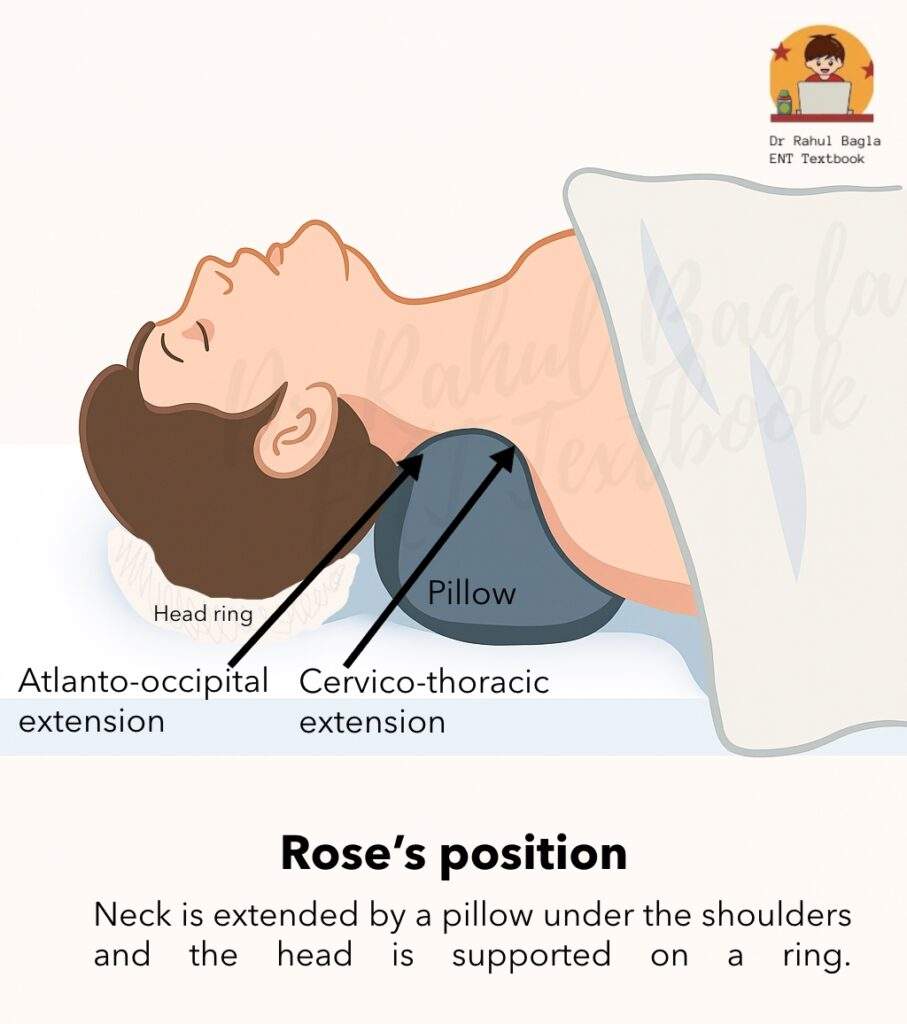
2. Position:
- The patient is typically placed in Rose’s position (also known as the Tonsillectomy position).
- The patient lies supine with a pillow or shoulder bag placed under the shoulders. This manoeuvre leads to extension at the atlanto-occipital and cervicothoracic joints (Important for viva).
- A rubber ring is placed under the head to stabilise it.
- Rationale for Rose’s position: This position allows for optimal visualisation of the oral cavity and oropharynx. Critically, it creates a dependent position for the nasopharynx, which helps to prevent the aspiration of blood and secretions into the trachea during surgery.
- The surgeon sits behind the patient’s head, using a headlight for illumination.
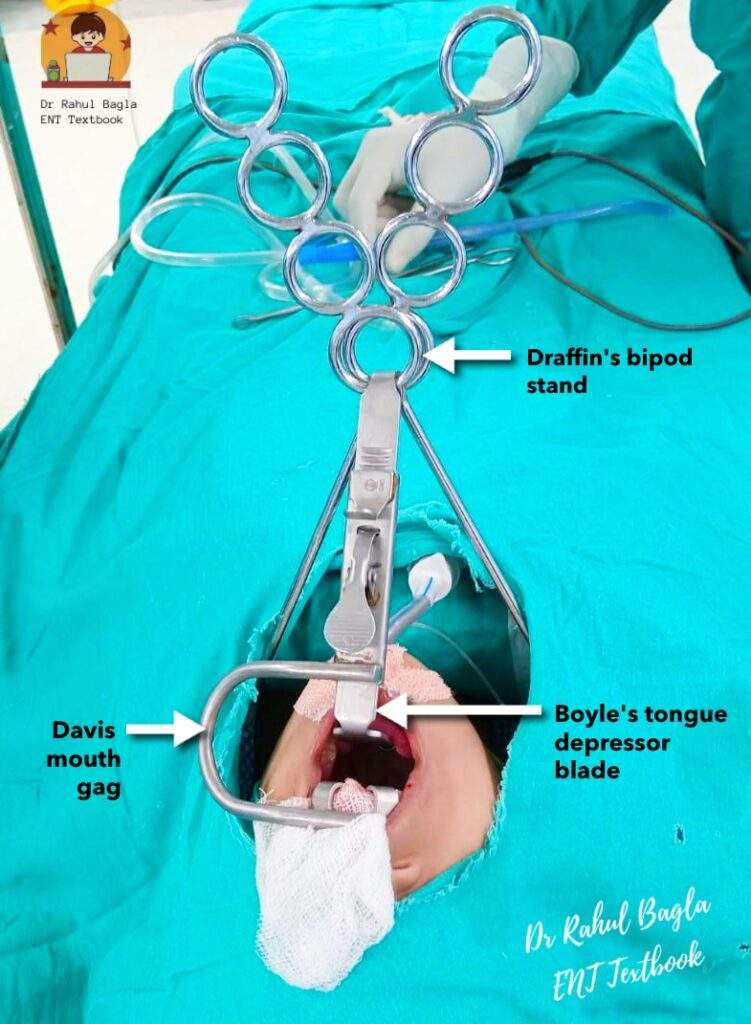
3. Mouth Opening and Gag Insertion: We use a Boyle-Davis mouth gag to keep the mouth open. Draffin’s bipods suspend the gag, stabilising both the gag and the patient’s head. The surgeon uses a curved tongue depressor to elevate the soft palate.
4. Throat Pack Insertion: A throat pack is inserted into the oropharynx. This serves a vital purpose:
- It prevents blood and secretions from entering the oesophagus.
- It prevents the aspiration of laryngeal clots.
- It minimises air and anaesthetic agent leakage.
5. Pre-Curettage Assessment: We use a finger to palpate the adenoid mass, pushing it medially and check for any abnormal vascular structures, such as a pulsating aberrant carotid artery, which is a rare but critical finding.
6. Adenoid Curette Insertion: We use an appropriately sized St. Clair Thomson’s adenoid curette with a guard. The curette is held in the right hand in a dagger-style grip. We introduce the curette into the nasopharynx, apply it over the posterior border of the nasal septum and then move downwards to engage the adenoid tissue.
7. Adenoid Removal: With a single, gentle, sweeping movement, we shave off the bulk of the adenoid tissue. We then use smaller curettes (luc’s forceps) for any lateral masses and punch forceps to remove residual lymphoid tissue. However, it is a blind procedure, and it is better to use a nasal endoscope to visualise the adenoid removal, avoiding injury to surrounding structures. Care is taken to avoid injury to the pharyngeal ends of the eustachian tubes.
8. Hemostasis: We achieve hemostasis by packing the area with a gauze swab for several minutes. If bleeding persists, we can electrocoagulate persistent bleeders under direct vision (if using an endoscope) or by carefully packing. If all else fails, a postnasal pack can be left for 24 hours.
9. Combined Procedures: If an adenotonsillectomy is planned, we perform the adenoidectomy first and place a pack in the nasopharynx for hemostasis. The tonsillectomy can then be performed with the pack in place.
Other Techniques for Adenoidectomy include:
- Microdebrider Adenoidectomy: This technique uses a rotating blade within a sheath to cut the adenoid tissue while simultaneously aspirating blood and tissue. It provides excellent hemostasis and allows for precise tissue removal under endoscopic guidance.
- Endoscopic Adenoidectomy: This is a major advance. Using a nasal endoscope, the surgeon can directly visualise the adenoid pad, the Eustachian tube orifices, and the choanae. This allows for complete removal of the adenoids and minimises the risk of injuring surrounding structures.
- Monopolar Cautery/Suction Diathermy Adenoidectomy: This method uses heat to both cut and coagulate tissue, which significantly minimises blood loss and post-operative bleeding.
- Transoral Coblation Adenoidectomy: This technique uses radiofrequency energy to ablate tissue at low temperatures. It results in minimal thermal damage to surrounding tissues and is associated with reduced pain and faster recovery.
- KTP Laser Adenoidectomy: While effective, this method is less common due to its high cost and the risk of collateral thermal damage, which can lead to postoperative nasopharyngeal stenosis.
Postoperative Care:
- Monitoring: We closely monitor the patient for any signs of bleeding from the nose or mouth. We also check vital signs (pulse, respiration, blood pressure) regularly. We keep the patient in a coma position (recovery position) until they are fully conscious to prevent aspiration.
- Diet: Once the patient is fully recovered from anesthesia, we allow cold liquids like ice cream or cold milk. Sucking on ice cubes can help relieve pain and discomfort. We then gradually advance the diet from soft foods to solids, encouraging plenty of fluids to maintain hydration.
- Hygiene: We advise patients to use gargles, such as betadine or saltwater, three to four times a day. Rinsing the mouth with plain water after every meal helps keep it clean.
- Medications: We manage postoperative pain with analgesics like paracetamol. A suitable oral antibiotic can be prescribed for about a week to prevent infection.
- Discharge: Patients are typically discharged within 24 hours if there are no complications. Normal activities can usually be resumed within two weeks.
Complications:
|
Complications |
Description and Management |
|
Hemorrhage |
|
|
Injury to the Eustachian Tube |
|
|
Injury to Pharyngeal Musculature and Vertebrae |
|
|
Grisel Syndrome |
|
|
Velopharyngeal Insufficiency (VPI) |
|
|
Nasopharyngeal Stenosis |
A rare complication caused by scarring and fibrosis, especially with excessive diathermy use or laser surgery. |
|
Recurrence |
Occurs due to the regrowth of adenoid tissue that was not completely removed. This is more common after blind curettage. |
|
Dental Injury |
It can accidentally occur from the mouth gag or if the gag slips. |
|
Nasopharyngeal Blood Clot |
|
———— End of the chapter ————
High-Yield Points for Exams
- Most Common Method: Blind curettage with St. Clair Thomson’s curette is still the most widely used.
- Gold Standard for Diagnosis: Nasal endoscopy.
- Position: Rose’s position, which provides a dependent nasopharynx to prevent aspiration.
- Throat Pack Rationale: Prevents aspiration and seals the airway.
- Strict Contraindication: Submucous cleft palate (risk of VPI).
- Special Concern in Down Syndrome: Atlantoaxial instability.
- Post-op Haemorrhage Signs: Rising pulse rate, vomiting of dark blood.
- Referred Pain: From adenoids to the ear is via CN IX and CN X.
- Post-op Pain Management: Paracetamol is the preferred analgesic. Aspirin and NSAIDs are avoided due to the risk of bleeding.
- Grisel Syndrome: Atlantoaxial dislocation, presenting as torticollis.
NEET PG-Style MCQs
- A 6-year-old child presents with chronic nasal obstruction and mouth breathing. During the preoperative assessment for adenoidectomy, the patient is found to have a submucous cleft palate. Which of the following is the most appropriate course of action? A) Proceed with the adenoidectomy as planned. B) Perform the adenoidectomy with a coblator to minimise tissue damage. C) Postpone the surgery and manage the symptoms medically. D) Adenoidectomy is strictly contraindicated due to the risk of velopharyngeal insufficiency.
- During an adenoidectomy, a patient is placed in Rose’s position. The primary rationale for this position is: A) To facilitate the introduction of St. Clair Thomson’s curettes. B) To prevent injury to the Eustachian tube orifice. C) To make the nasopharynx dependent and prevent blood aspiration. D) To provide better exposure for a tonsillectomy performed simultaneously.
- The most sensitive indicator of an occult post-adenoidectomy haemorrhage that the patient might be swallowing is: A) Dropping blood pressure. B) Increasing respiratory rate. C) Falling platelet count. D) Rising pulse rate.
- Which of the following is considered the most common and traditional method of performing an adenoidectomy? A) Endoscopic adenoidectomy B) Coblation adenoidectomy C) St. Clair Thomson’s blind curettage D) Microdebrider adenoidectomy
- Grisel syndrome, a rare complication of adenoidectomy, is characterised by: A) Postoperative haemorrhage. B) Nasopharyngeal stenosis. C) Atlantoaxial dislocation leading to torticollis. D) Velopharyngeal insufficiency.
- An ENT resident is asked to list the strict contraindications for an adenoidectomy. Which of the following should be included in their list? A) Chronic sinusitis B) Mild snoring C) Recurrent rhinitis D) Hemorrhagic diathesis
- A 5-year-old boy is scheduled for adenoidectomy and myringotomy with grommet insertion. The indication for the myringotomy and grommet insertion is most likely: A) Recurrent acute otitis media (RAOM). B) Otitis media with effusion (OME). C) Chronic suppurative otitis media (CSOM). D) Cholesteatoma.
- Which of the following modern adenoidectomy techniques is associated with a high risk of postoperative nasopharyngeal stenosis due to thermal damage? A) Microdebrider adenoidectomy B) Coblation adenoidectomy C) KTP Laser adenoidectomy D) Suction diathermy adenoidectomy
- The main purpose of inserting a throat pack during an adenoidectomy procedure is to: A) Provide a better surgical field for the surgeon. B) Prevent injury to the pharyngeal wall. C) Prevent the aspiration of blood and secretions into the trachea. D) Reduce postoperative pain and swelling.
- A child with Down syndrome is undergoing a preoperative assessment for adenoidectomy. The most critical special consideration to address before positioning the child for surgery is: A) The need for prophylactic antibiotics. B) The presence of potential cardiac abnormalities. C) The risk of atlantoaxial instability. D) The likelihood of a difficult intubation.
MCQ Answers and Explanations
- D) Adenoidectomy is strictly contraindicated due to the risk of velopharyngeal insufficiency. Removing the adenoids, which help close the nasopharynx during speech, can lead to hypernasality and nasal regurgitation in patients with a submucous cleft palate.
- C) To make the nasopharynx dependent and prevent blood aspiration. Rose’s position provides a dependent nasopharynx, which allows blood to flow away from the airway and into the oropharynx, from where it can be suctioned.
- D) Rising pulse rate. A rising pulse rate (tachycardia) is often the first and most reliable sign of reactionary haemorrhage, especially in children, who may be swallowing blood.
- C) St. Clair Thomson’s blind curettage. Despite the availability of modern techniques, blind curettage is still the most commonly used and taught traditional method.
- C) Atlantoaxial dislocation leading to torticollis. Grisel syndrome is a rare but distinct complication involving subluxation of the C1-C2 joint, resulting in a painful, wry neck.
- D) Haemorrhagic diathesis. Uncontrolled bleeding disorders are an absolute contraindication to adenoidectomy due to the high risk of severe and life-threatening haemorrhage.
- B) Otitis media with effusion (OME). Myringotomy with grommet insertion is the standard surgical treatment for persistent otitis media with effusion, which is a common sequela of adenoid hypertrophy.
- C) KTP Laser adenoidectomy. The high thermal energy from lasers can cause collateral damage and subsequent scarring, leading to nasopharyngeal stenosis.
- C) Prevent the aspiration of blood and secretions into the trachea. The throat pack acts as a physical barrier, sealing off the airway from blood and secretions during the procedure.
- C) The risk of atlantoaxial instability. Children with Down syndrome have a higher risk of C1-C2 instability. Hyperextending the neck in Rose’s position could cause a catastrophic spinal cord injury.
Clinical-Based Questions (Practical & Viva Scenarios)
- Case Scenario: A 7-year-old girl is scheduled for adenoidectomy due to chronic mouth breathing and snoring. Her mother reports that she was born with a “shortened uvula.” On clinical examination, you notice a bifid uvula.
- a) What is the most likely diagnosis?
- Answer: The bifid uvula, along with the history, is a strong indicator of a submucous cleft palate.
- b) Would you proceed with the adenoidectomy? Why or why not?
- Answer: No, I would not. A submucous cleft palate is a strict contraindication to adenoidectomy. The adenoids play a crucial role in compensating for the palatal insufficiency by helping to close off the nasopharynx during speech and swallowing. Removing the adenoids would lead to severe velopharyngeal insufficiency (VPI), resulting in a hypernasal voice and nasal regurgitation of food.
- c) What would be your management plan?
- Answer: I would cancel the adenoidectomy and refer the patient to a craniofacial team or a plastic surgeon for a palatoplasty to correct the cleft. I would also manage the child’s nasal symptoms conservatively with nasal corticosteroids and saline rinses, while also counselling the parents about the risks of surgery.
- a) What is the most likely diagnosis?
FAQ Section in Viva
- What is an adenoidectomy?
- Adenoidectomy is a surgical procedure to remove the adenoids, which are lymphoid tissues located at the back of the nose.
- What are the main reasons for an adenoidectomy?
- The main reasons include chronic nasal obstruction, snoring, Obstructive Sleep Apnea (OSA), and recurrent ear infections (otitis media with effusion).
- Is an adenoidectomy a major surgery?
- While it is a common procedure, it is considered a major surgery requiring general anaesthesia and careful postoperative monitoring for complications like bleeding.
- What is the typical recovery time after an adenoidectomy?
- Most children recover quickly, with normal activities resuming within one to two weeks, though some discomfort and a change in voice may be noted temporarily.
- Are there any serious risks associated with adenoidectomy?
- The most serious risks include haemorrhage, airway obstruction, and rare complications like Grisel syndrome or velopharyngeal insufficiency in patients with an undiagnosed cleft palate.
- What should a child eat after an adenoidectomy?
- A child should start with cold, soft liquids like ice cream and milk, gradually advancing to soft foods over the next few days. Avoid hot, spicy, or sharp foods.
- Does an adenoidectomy affect the immune system?
- No, removing the adenoids does not have a significant long-term impact on a child’s immune system, as other lymphoid tissues of Waldeyer’s ring and the systemic immune system compensate.
———— End ————
Download full PDF Link:
Adenoidectomy Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Cummings, Otolaryngology-Head and Neck Surgery.
- Stell and Maran’s, Textbook of Head and Neck Surgery and Oncology.
- Ballenger’s, Otorhinolaryngology Head And Neck Surgery
- Susan Standring, Gray’s Anatomy.
- Frank H. Netter, Atlas of Human Anatomy.
- B.D. Chaurasiya, Human Anatomy.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery.
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Ganong’s Review of Medical Physiology.
- Guyton & Hall Textbook of Medical Physiology.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Juvenile Angiofibroma. https://www.entlecture.com/juvenile-angiofibroma/
- Please read. Tumours of Hypopharynx . https://www.entlecture.com/tumours-of-the-hypopharynx/
- Please read. Anatomy of Oesophagus. https://www.entlecture.com/anatomy-of-oesophagus/
Keywords: What are adenoids and their function, Symptoms of swollen adenoids in children, Adenoidectomy recovery tips for parents, Natural remedies for enlarged adenoids, Adenoids and breathing problems in kids, Adenoid-related ear infections treatment, Adenoids vs tonsils: key differences, When do adenoids need to be removed, Adenoid issues and sleep apnea connection, How to diagnose adenoid problems at home, Adenoids explained: symptoms, treatments, and when to seek help, Swollen adenoids in children: causes and effective remedies, Everything you need to know about adenoidectomy recovery, The role of adenoids in your child’s health: what to watch for, Natural remedies for enlarged adenoids: a parent’s guide, Adenoids and sleep apnea: how they’re connected, Adenoids vs. Tonsils: understanding the differences and care tips, When should adenoids be removed? Signs and expert advice, Common myths about adenoids debunked: what parents should know, How to diagnose and manage adenoid issues at home, The nasopharyngeal tonsil, commonly referred to as the “adenoids,” is located where the roof and posterior wall of the nasopharynx meet, adenoidectomy recovery tips, natural remedies for swollen adenoids, adenoid hypertrophy in adults, adenoids and sleep apnea connection, endoscopic adenoid removal procedure, adenoid-related ear infections in children, diet after adenoid surgery, adenoid regrowth symptoms, adenoid biopsy procedure details, adenoid cystic carcinoma prognosis
