Anatomy of External Ear
The human ear is an important sense organ responsible for hearing and balance. It comprises three main parts: the outer ear, the middle ear, and the inner ear. Each part plays a vital role in collecting sound from the environment and transmitting it to the brain, where the speech and auditory centres process the information.
Functions of the Ear
- Hearing: The primary function of the ear is to collect sound waves, amplify them, and convert them into electrical signals that the brain can interpret. This process allows us to perceive and understand sounds from our surroundings.
- Balance (Equilibrium): The ear also plays a critical role in maintaining balance. The vestibular system in the inner ear detects changes in head position and movement, coordinating with the eyes and muscles to help maintain stability and avoid falls.
Additional Roles of the Ear
- Warning System: The ear helps detect potentially threatening sounds from the environment, acting as a warning system to alert us to danger.
- Communication: It is a major component of our communication system, enabling us to hear and interpret speech, music, and other sounds.
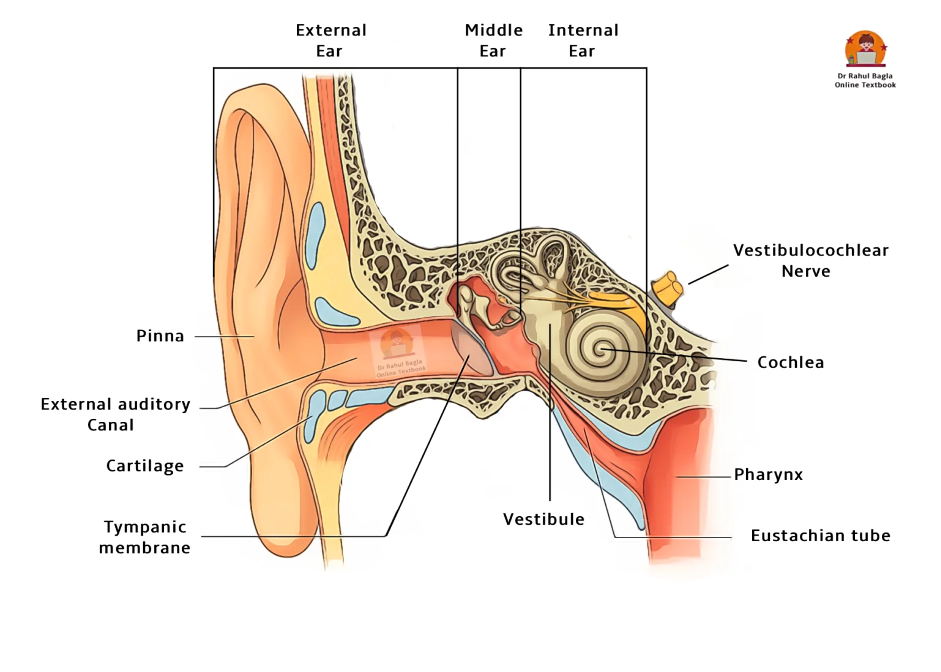
Anatomically, the ear is divided into three parts: the external ear, the middle ear, and the internal ear.
External Ear. The external ear consists of three main components:
- Auricle (Pinna): This is the visible outer portion of the ear that is attached to the lateral aspect of the head. It captures sound waves and directs them into the external auditory canal.
- External Auditory Canal: This canal extends from the auricle to the tympanic membrane (eardrum), which closes off the canal. It serves as a passageway for sound waves to reach the eardrum.
- Tympanic membrane (Ear Drum).
Middle Ear. The middle ear is an air-filled, mucous membrane-lined cavity located in the petrous part of the temporal bone. Middle ear lies between the tympanic membrane on the lateral side and the lateral wall of the internal ear on the medial side. The middle ear is connected to the nasopharynx by a narrow tube called the eustachian tube, which helps equalize air pressure in the middle ear. The middle ear contains a chain of three tiny bones called ossicles:
- Malleus (Hammer): Attached to the tympanic membrane, it transmits vibrations from the eardrum to the incus.
- Incus (Anvil): The middle ossicle that connects the malleus to the stapes.
- Stapes (Stirrup): The smallest bone in the body, which transmits sound vibrations from the incus to the inner ear through the oval window.
Internal Ear (Labyrinth). The internal ear, also known as the labyrinth, is responsible for converting mechanical signals from the external and middle ear into electrical signals that are transmitted to the brain. It consists of two main labyrinths: the bony labyrinth and the membranous labyrinth.
- Bony Labyrinth: This structure is divided into two main parts:
- Vestibular Apparatus: Consisting of the vestibule and semi-circular canals, it contains sensory organs responsible for postural equilibrium and balance.
- Cochlea: Shaped like a snail shell, it contains the sensory organ of hearing.
- Membranous Labyrinth: This structure is located within the bony labyrinth and includes the utricle, saccule, semi-circular ducts, and cochlear duct. It contains a clear fluid called endolymph. The space between the membranous and bony labyrinths is filled with perilymph.

The External Ear
The external ear comprises three main parts: (i) the auricle or pinna, (ii) the external acoustic canal, and (iii) the tympanic membrane.
Auricle or Pinna
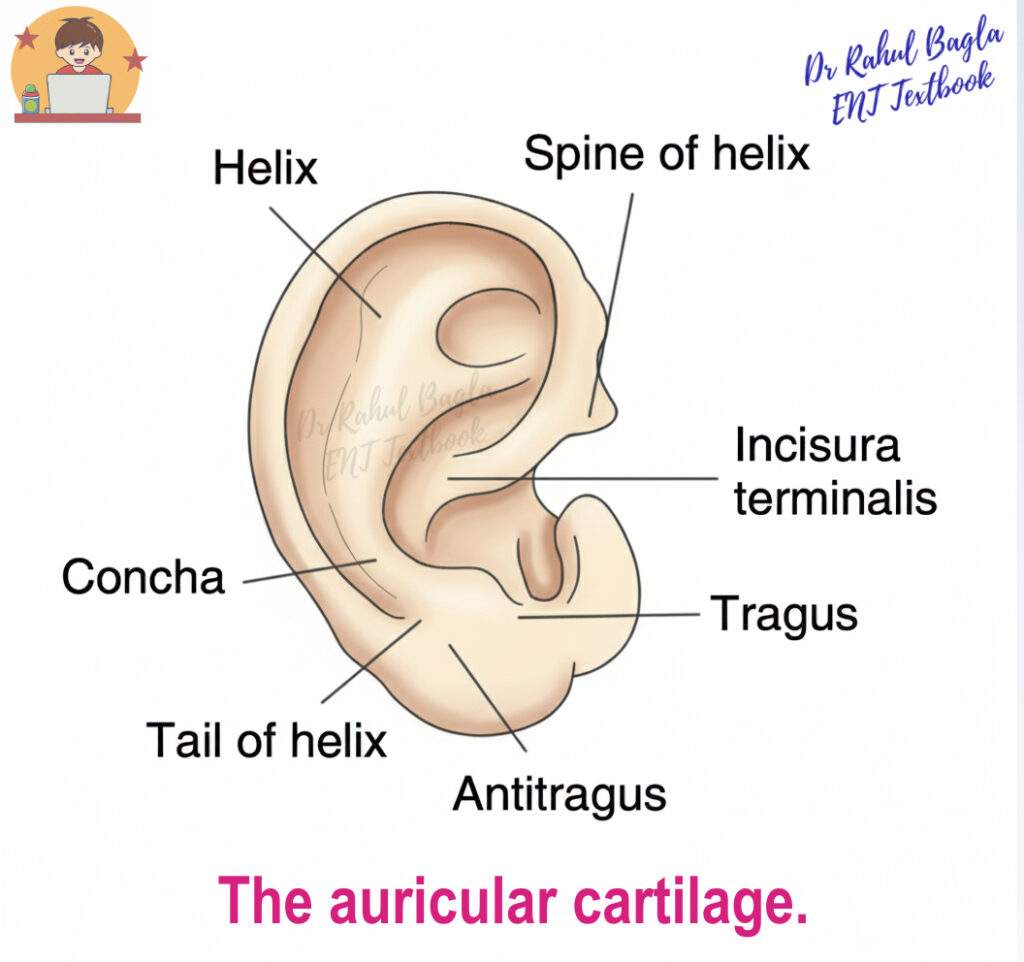
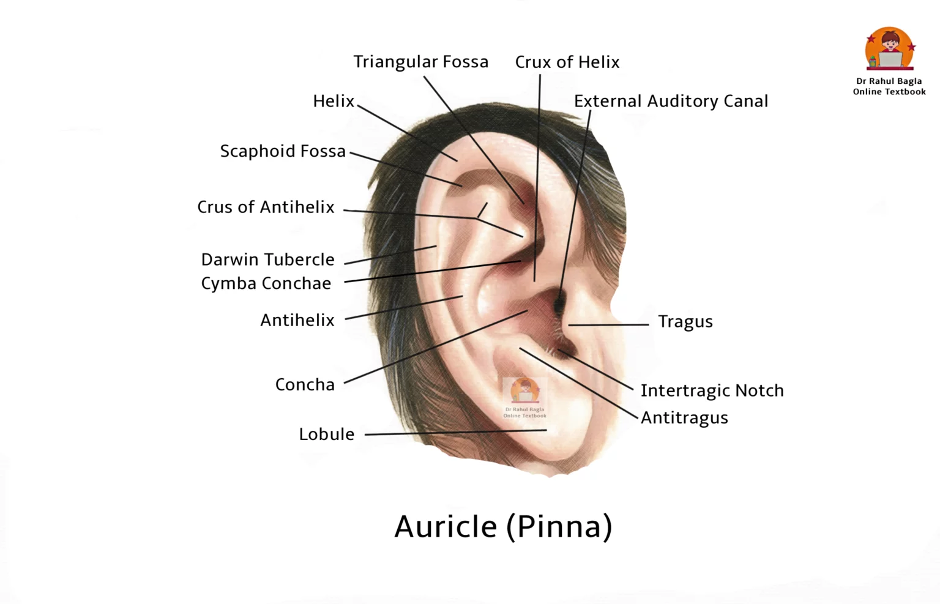
The auricle, or pinna, plays an important role in focusing and localising sound waves from the environment. Apart from its lobule, the pinna consists of a single piece of yellow elastic cartilage covered with skin. The lobule contains adipose tissue, while the contour of the pinna is shaped by the configuration of its elastic cartilage. This cartilage also forms the outer one-third of the external acoustic canal.
Clinical Relevance of the Pinna. In reconstructive surgery, cartilage from the tragus, perichondrium from the tragus or concha, and fat from the lobule are often used as grafts. Conchal cartilage is used to correct a depressed nasal bridge, and composite grafts of skin and cartilage are employed for repairing defects of the nasal ala.
Surfaces of the Auricle. There are two surfaces of the auricle: the medial (inner) and the lateral (outer). The skin on the lateral surface is tightly bound to the perichondrium, while it is loosely attached on the medial surface. The medial surface attaches to the skull and is less significant. The lateral aspect is concave, with various prominences and depressions.
Prominences and depressions of the pinna:
- The outside rim is called the helix, and it ends inferiorly at the lobule.
- A smaller curved rim, parallel and anterior to the helix, is the antihelix.
- The large hollow centre area is called the concha.
- The external acoustic meatus starts from the bottom of the concha.
- Just anterior to the opening of the external acoustic meatus and in front of the concha is an elevation (the tragus).
- Opposite the tragus is another elevation called antitragus.

Muscles of the Pinna
- Extrinsic Muscles (three in number): These include the anterior, superior, and posterior auricular muscles. They pass from the scalp or skull to the auricle and play a role in positioning the auricle.
- Intrinsic Muscles (six in number): These muscles pass between the cartilaginous parts of the auricle and can change the shape of the auricle. However, they are small, inconsistent, and generally have no useful function.
Innervation. The facial nerve innervates both groups of muscles.

Blood Supply of the Pinna
- Posterior Auricular Artery: A branch of the external carotid artery, it is the main artery supplying the medial surface (except the lobule), concha, middle and lower portions of the helix, and the lower part of the antihelix.
- Anterior Auricular Artery: A branch of the superficial temporal artery, it supplies the upper portions of the helix, antihelix, triangular fossa, tragus, and lobule.
- Small Auricular Branch from the Occipital Artery: This may assist the posterior auricular artery.

Venous drainage of the pinna is through vessels following the arteries.
Lymphatic Drainage of the Pinna
- Lymph from the medial surface drains to the lymph nodes at the mastoid tip.
- Lymph from the tragus and upper part of the lateral surface drains to the preauricular nodes.
- Lymph from the remaining auricle drains to the upper deep cervical nodes.
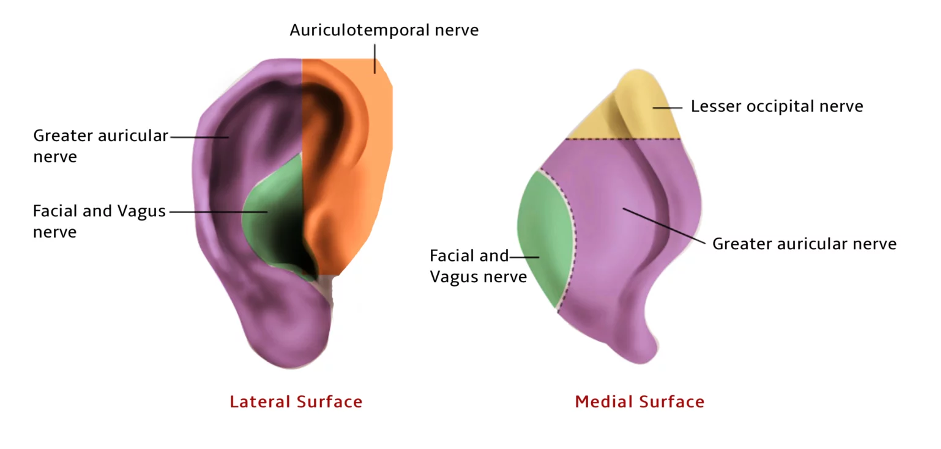
Nerve Supply of the Pinna
- Auriculotemporal Nerve (branch of the mandibular division of the trigeminal nerve, V3): Supplies the anterosuperior part of the lateral surface of the pinna, including the tragus and crus of the helix.
- Greater Auricular Nerve (C2, C3): A nerve of the cervical plexus that supplies most of the outer part of the medial surface, the posterior part of the lateral surface, and the postauricular region.
- CN VII (Facial Nerve): Innervates the skin of the concha on both sides, antihelix and retroauricular groove.
- CN X (Vagus Nerve): Its auricular branch (Arnold’s nerve) supplies the concha on both sides and postauricular skin.
- Lesser Occipital Nerve (C2): A nerve of the cervical plexus, it supplies the upper part of the medial surface of the auricle and the postauricular region.
The External Auditory Canal
The external auditory canal (EAC) extends from the bottom of the concha to the tympanic membrane, measuring approximately 24 mm along its posterior wall, with the anterior wall being 6 mm longer. The canal is wider laterally and narrows medially.
The EAC has a characteristic S-shape:
- The cartilaginous part is directed upwards, backwards, and medially.
- The bony part is directed downwards, forwards, and medially.
Practical Tip for Otoscopy: To properly examine the canal and tympanic membrane, the pinna must be pulled upwards, backwards, and laterally in adults to straighten the S-shape of the ear canal. In neonates, however, due to the underdeveloped bony part, the pinna is pulled downwards, backwards, and laterally. This is a common question on ENT practical exams.
Structure of the EAC
The EAC is structurally divided into two main parts:
- Cartilaginous Outer (Lateral) One-Third Part: Measuring about 8 mm, it is formed by the same yellow elastic cartilage as the pinna.
- Bony Inner (Medial) Two-Third Part: Measuring about 16 mm, it is primarily formed by the tympanic part of the temporal bone, with the roof formed by the squamous part of the temporal bone.

Cartilaginous Part
The cartilaginous outer one-third is attached to the bony part of the external auditory canal by fibrous bands. The skin over this section is thick and contains hairs and modified apocrine sweat glands (ceruminous and pilosebaceous glands) which produce earwax. The presence of hairs helps prevent foreign bodies from entering into the ear. Therefore, furuncles (staphylococcal infection of hair follicles) are seen only in this part. There are two horizontal deficiencies – the “fissures of Santorini” in this part increase flexibility but allow infections (e.g. malignant otitis externa) and neoplasms to spread to and from the parotid and temporomandibular regions.
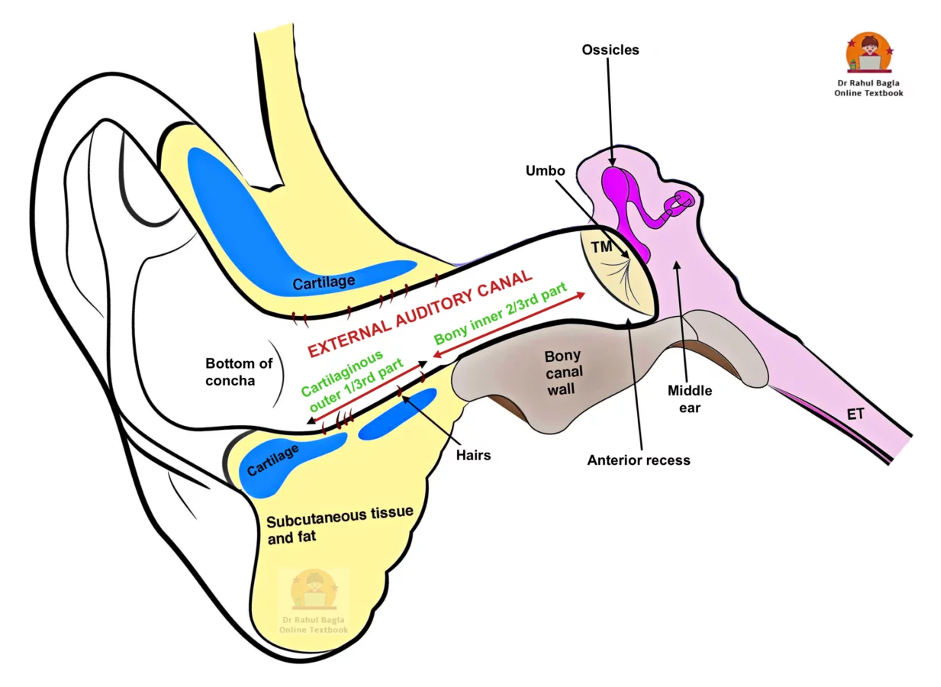
Bony Part
The bony inner two-thirds is narrow, with its medial end marked by the tympanic sulcus, a groove that is absent superiorly. The skin here is thin and continuous with the tympanic membrane. The “isthmus,” about 5-6 mm lateral to the tympanic membrane, narrows the bony canal’s diameter, making it difficult to remove foreign bodies lodged medially. Beyond the isthmus, the anteroinferior part of the deep meatus dips forwards, forming a wedge-shaped “anterior recess”. This recess acts as a gutter for ear discharge and debris, and becomes a tough spot to access either in the clinic or at surgery. Wax is usually not seen in this part, and if present over the pars flaccida or attic region is rarely true wax. It is almost always associated with an underlying cholesteatoma. Sagging in the posterosuperior part can indicate acute mastoiditis due to its relation with the mastoid antrum. The foramen of Huschke, found in the anteroinferior part, can persist into adulthood and, like the fissures of Santorini, allows infections and neoplasms to spread.
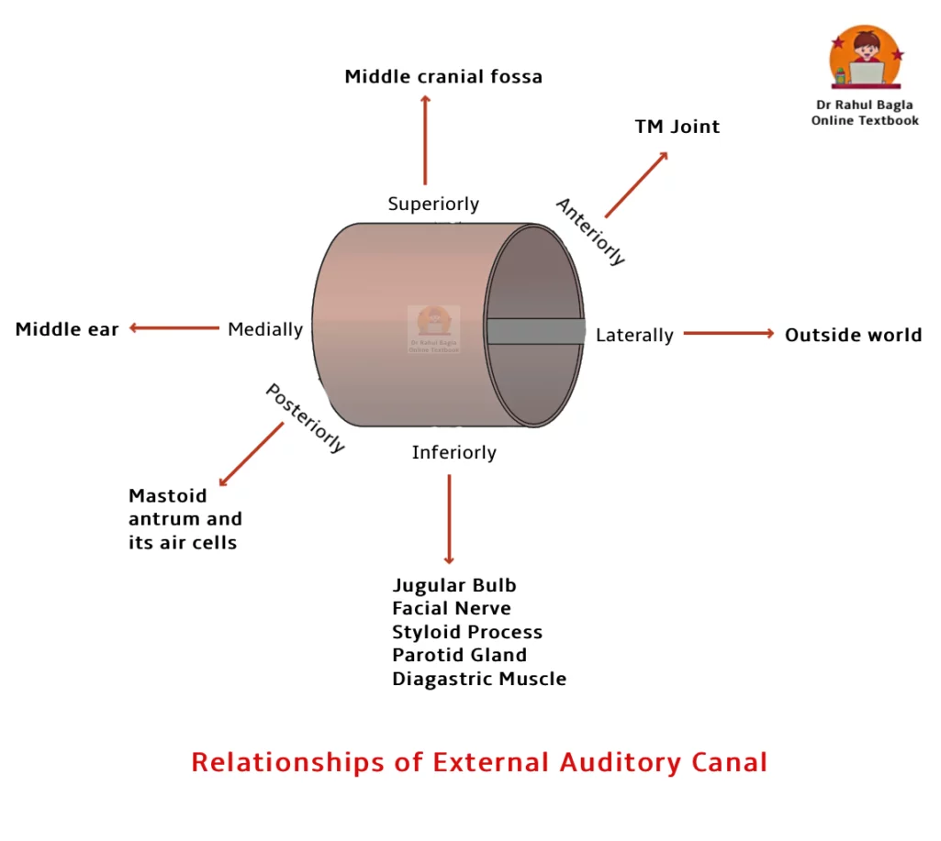
Relationships of EAC
The surrounding structures of the EAC are crucial for understanding the spread of infection and surgical approaches:
- Superior: Middle cranial fossa (risk of intracranial complications)
- Inferior: Parotid gland (risk of parotitis, facial nerve involvement)
- Posterior: Mastoid antrum and air cells, and the facial nerve (risk of mastoiditis, facial nerve palsy)
- Anterior: Temporomandibular joint (TMJ) (TMJ pain can be referred to the ear, and vice versa)
- Medial: Tympanic membrane and middle ear
- Lateral: Outside world
Nerve Supply of the EAC
- Auriculotemporal Nerve (CN V3): Supplies the anterior and superior walls.
- Auricular Branch of CN X (Vagus Nerve – Arnold’s Nerve): Supplies the posterior and inferior walls.
- CN VII (Facial Nerve): Innervates the skin of the mastoid and posterior EAC.
Important Clinical Points
- Hitzelberger’s Sign: The hypoesthesia (decreased sensation) of the posterior meatal wall occurs due to the pressure on the facial nerve (sensory fibers are affected early) in patients with acoustic neuroma. This is a classical neurological sign.
- Vasovagal Reflex: During EAC cleaning, stimulation of Arnold’s branch of the vagus nerve can cause coughing, bradycardia, syncope, and even cardiac arrest.
- Ramsay Hunt Syndrome (Herpes Zoster Oticus): The presence of herpetic vesicles on the mastoid and posterior meatal wall indicates involvement of the geniculate ganglion of the facial nerve, often associated with facial nerve palsy.
Tympanic Membrane or the Drumhead.
The tympanic membrane forms a partition between the external acoustic canal and the middle ear. It is located at the medial end of the external auditory meatus and forms the majority of the lateral wall of the middle ear cavity.
Key Dimensions and Orientation:
- The TM is set obliquely, meaning the posterosuperior part is more lateral than the anteroinferior part. This oblique orientation is clinically significant for drainage and examination.
- Measures approximately 9–10 mm in height and 8–9 mm in width.
- It is remarkably thin, about 0.1 mm thick.
- Slightly oval in shape, broader at the top than the bottom.
- Forms an angle of approximately 55° with the floor of the external auditory canal.

Divisions of the Tympanic Membrane: The tympanic membrane is divided into two parts:
- Pars Tensa. It is the lower part of the tympanic membrane and forms the majority of the tympanic membrane. The periphery of the tympanic membrane is thickened to form a fibrocartilaginous ring known as the annulus tympanicus, which fits into the bony tympanic sulcus. The bony tympanic sulcus makes an incomplete ring and does not extend into the notch of Rivinus at the roof of the canal. From the superior limits of the sulcus, the annulus becomes a fibrous band that runs centrally as the anterior and posterior malleolar folds toward the lateral process of the malleus. The remaining part of the bony ring is formed by the squamous part of the temporal bone. The central part is tented inwards at the level of the malleus, called the umbo, and a bright cone of light can be observed radiating from the malleus to the periphery in the anteroinferior quadrant of the tympanic membrane.
- Pars Flaccida (Shrapnell’s Membrane). It is the upper part of the tympanic membrane and forms a small part of the tympanic membrane. It is situated above the lateral process of the malleus, between the notch of Rivinus and the anterior and posterior malleolar folds. The pars flaccida is less taut and often appears slightly pinkish.
Clinical Significance: Due to its flaccid nature and lack of a robust middle fibrous layer, the pars flaccida is more prone to retraction pockets and cholesteatoma formation, making it a critical area for examination.

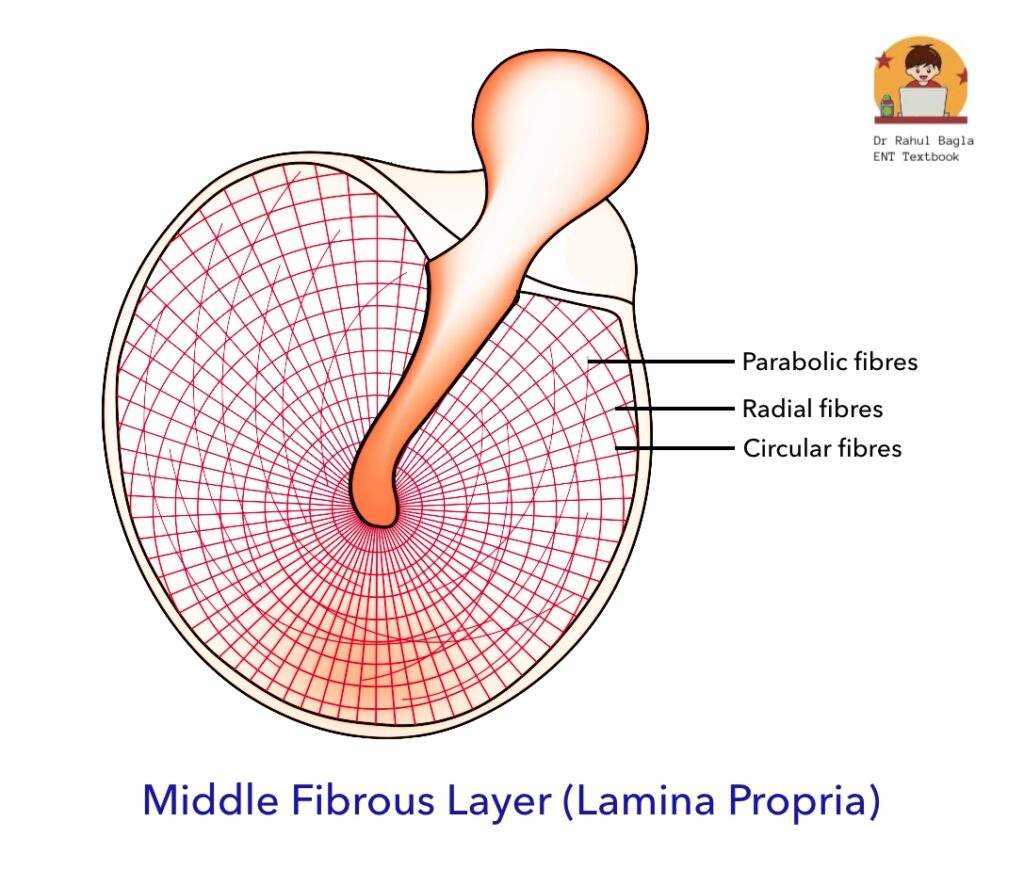
Layers of the Tympanic Membrane. The tympanic membrane consists of three distinct layers:
- Outer Epithelial Layer: Continuous with the skin lining the external auditory canal.
- Inner Mucosal Layer: Continuous with the mucosa of the middle ear.
- Middle Fibrous Layer (Lamina Propria): This is the crucial layer responsible for the TM’s strength and vibratory properties. It is present between the outer epithelial layer and inner mucosal layer and encloses the handle of the malleus. It consists of three types of fibers:
- Radial fibers: Extend from the handle of the malleus outwards to the annulus.
- Circular fibers: Concentrically arranged, especially towards the periphery.
- Parabolic fibers: Less prominent but contribute to the complex pattern of TM displacement during sound transmission.
- Note: In the pars flaccida, the middle fibrous layer (lamina propria) is significantly less prominent, and the orientation of its collagen fibers is more random. This structural difference accounts for its flaccidity and propensity for pathology.
Blood Supply of the Tympanic Membrane. The arterial supply originates from branches supplying both the external auditory meatus and the middle ear.
- Lateral Surface of TM: Supplied by the auricular branch of the maxillary artery.
- Medial Surface of TM: Supplied by the anterior tympanic branches of the maxillary artery, the stylomastoid branch of the posterior auricular artery, and potentially from the middle meningeal artery.
Nerve Supply of the Tympanic Membrane
- Lateral Surface of TM:
- Anterior half: Innervated by the auriculotemporal nerve (CN V3).
- Posterior half: Supplied by the auricular branch of the vagus nerve (CN X), also known as Arnold’s nerve.
- Medial Surface of TM: Receives innervation from the tympanic branch of the glossopharyngeal nerve (CN IX), also known as Jacobson’s nerve.
Otoscopy: Clinical Examination of the External Ear
Otoscopy is the fundamental clinical procedure used to examine the external ear canal and tympanic membrane.
Normal Findings:
- A normal tympanic membrane is typically shiny and pearly-grey in appearance.
- The transparency of the tympanic membrane can vary among individuals.
- Shadows of middle ear structures, such as the incudostapedial joint and round window, can often be seen through the membrane, especially in children or very thin TMs.
- Key landmarks such as the umbo, handle of malleus, lateral process of malleus, anterior and posterior malleolar folds, and the cone of light should be clearly visible.
Mobility (Seigalization/Pneumatic Otoscopy):
- A healthy tympanic membrane is mobile.
- Its mobility can be tested using a pneumatic otoscope or Siegel’s speculum, which allows for changes in air pressure within the external auditory canal. Observing TM movement is crucial for diagnosing middle ear effusions or adhesive otitis media.
———— End of the chapter ————
High-Yield Points for NEET PG and University Exams
- Pinna Cartilage: Yellow elastic cartilage (except lobule – adipose). Used for grafts (tragal, conchal, lobule fat).
- Furuncles: Only in cartilaginous EAC due to hair follicles.
- Fissures of Santorini & Foramen of Huschke: Deficiency in EAC cartilage/bone, allowing spread of infection to/from parotid/TMJ.
- Isthmus of EAC: Narrowest part of the bony canal, common site for foreign body impaction.
- Anterior Recess: Anteroinferior dip in bony EAC, difficult to clean discharge/debris.
- Wax in Bony EAC: Rare; if present near pars flaccida, suspect cholesteatoma.
- Sagging Posterosuperior EAC: Sign of acute mastoiditis due to proximity to mastoid antrum.
- Arnold’s Nerve (Auricular branch of Vagus CN X): Supplies posterior EAC wall and concha. Stimulation causes vasovagal reflex (coughing, bradycardia, syncope).
- Hitzelberger’s Sign: Hypoesthesia of posterior meatal wall due to acoustic neuroma (facial nerve sensory fiber compression).
- Pars Flaccida: Small, upper part of TM, lacks robust fibrous layer, prone to retraction and cholesteatoma.
- Cone of Light: Anteroinferior quadrant of normal TM, indicates healthy, mobile TM.
- Jacobson’s Nerve (Tympanic branch of Glossopharyngeal CN IX): Supplies medial surface of TM and middle ear mucosa.
- Otoscopy Adult vs. Child: Pull pinna UP, BACK, LATERAL in adults; DOWN, BACK, LATERAL in neonates.
MCQs – For NEET PG & University Exams
- A 32-year-old man presents with an itchy, painful swelling in the outer ear canal. Otoscopic exam reveals a furuncle in the lateral third of the canal. What is the likely site of infection?
A. Bony part of EAC
B. Cartilaginous part of EAC
C. Tympanic membrane
D. Mastoid process - The auricle receives its main blood supply from which artery?
A. Superficial temporal artery
B. Maxillary artery
C. Anterior tympanic artery
D. Posterior auricular artery - Arnold’s nerve, a branch of which cranial nerve, may trigger cough during ear cleaning?
A. CN V
B. CN VII
C. CN IX
D. CN X - A 45-year-old patient with acoustic neuroma reports reduced sensation over the posterior wall of EAC. Which sign describes this finding?
A. Tullio’s phenomenon
B. Hitzelberger’s sign
C. Schwartze’s sign
D. Battle’s sign - During ear examination, a pinkish, flaccid area above the lateral process of malleus is seen. This corresponds to:
A. Pars tensa
B. Annulus tympanicus
C. Umbo
D. Pars flaccida - A child presents with postauricular swelling, pain, and drooping of the posterior EAC wall. What is the most likely diagnosis?
A. Otitis media with effusion
B. Acute mastoiditis
C. Cholesteatoma
D. Eustachian tube blockage - Which nerve provides sensation to the tragus and anterior wall of the external auditory canal?
A. Greater auricular nerve
B. Lesser occipital nerve
C. Auriculotemporal nerve
D. Facial nerve - Which part of the external ear is derived from the first and second pharyngeal arches?
A. Cochlea
B. Auricle
C. Tympanic membrane
D. Eustachian tube - In tympanic membrane anatomy, which part is most vulnerable to retraction pocket formation?
A. Umbo
B. Pars tensa
C. Pars flaccida
D. Cone of light - A patient has loss of conical light reflex and an immobile tympanic membrane on pneumatic otoscopy. What does this indicate?
A. Normal finding
B. Serous otitis media
C. Tympanic membrane perforation
D. EAC atresia - Which muscle group helps in positioning of the auricle and is innervated by the facial nerve?
A. Intrinsic muscles
B. Extrinsic muscles
C. Stapedius
D. Tensor tympani - The tympanic sulcus provides attachment to:
A. Pars flaccida
B. Malleus
C. Annulus tympanicus
D. Cone of light - In otoscopy, the cone of light is typically seen in:
A. Anterosuperior quadrant
B. Posteroinferior quadrant
C. Anteroinferior quadrant
D. Posterosuperior quadrant - A patient with vesicular lesions in the EAC and postauricular area, facial palsy, and hearing loss is diagnosed with:
A. Otitis externa
B. Ramsay Hunt syndrome
C. Acute otitis media
D. Bell’s palsy - Which of the following statements about the external auditory canal is correct?
A. Entire canal is lined by thin skin with ceruminous glands
B. Isthmus is a dilation near tympanic membrane
C. Anterior wall is longer than the posterior wall
D. Furuncles occur in the bony part only
✅ Answer Key with Detailed Explanations
- B. Cartilaginous part of EAC. The lateral one-third of the external auditory canal is cartilaginous and contains hair follicles, sebaceous glands, and ceruminous glands. Furunculosis (boil) commonly arises here due to infection of hair follicles, usually by Staphylococcus aureus.
- D. Posterior auricular artery. The auricle is supplied mainly by branches of the external carotid artery: the posterior auricular artery (medial and posterior auricle) and the superficial temporal artery (anterior auricle). The posterior auricular artery is particularly significant in otologic surgeries.
- D. CN X (Vagus nerve). Arnold’s nerve is the auricular branch of the vagus nerve. It supplies the posterior and inferior walls of the EAC and can cause a reflex cough or even syncope during ear manipulation.
- B. Hitzelberger’s sign. Seen in vestibular schwannoma (acoustic neuroma), this is the loss of sensation over the posterior superior wall of EAC, supplied by the auricular branch of the facial nerve, indicating facial nerve involvement.
- D. Pars flaccida. Pars flaccida (Shrapnell’s membrane) lies above the lateral process of malleus. It is thin and lacks a fibrous layer, making it a common site for retraction pockets and primary acquired cholesteatoma.
- B. Acute mastoiditis. A classic sign of mastoiditis is postauricular swelling and sagging of the posterior EAC wall due to pus tracking into the mastoid air cells from the middle ear.
- C. Auriculotemporal nerve. A branch of the mandibular nerve (V3), it supplies the tragus, anterior EAC wall, and anterior auricle. Knowledge of this is crucial in regional nerve blocks for ear surgery.
- B. Auricle. The auricle develops from 6 auricular hillocks, 3 from each of the first and second pharyngeal arches. Disruption can lead to congenital anomalies like microtia.
- C. Pars flaccida. Due to its weak structure and lack of the fibrous layer, this part of the tympanic membrane is susceptible to negative pressure retraction, forming a cholesteatoma.
- B. Serous otitis media. Pneumatic otoscopy in SOM shows immobility of the TM due to fluid in the middle ear. Loss of cone of light is another typical sign.
- B. Extrinsic muscles. These muscles (auricularis anterior, superior, and posterior) are controlled by the facial nerve (CN VII). They allow movement of the auricle, although function is minimal in humans.
- C. Annulus tympanicus. The annulus fibrosus or annulus tympanicus fits into the tympanic sulcus, anchoring the pars tensa portion of the tympanic membrane to the temporal bone.
- C. Anteroinferior quadrant. The cone of light is a normal light reflex seen in a healthy tympanic membrane and is visible in the anteroinferior quadrant during otoscopy.
- B. Ramsay Hunt syndrome. This is herpes zoster oticus with involvement of facial nerve (CN VII). Patients present with vesicles in the EAC, facial paralysis, and sometimes hearing loss or vertigo.
- C. Anterior wall is longer than the posterior wall. The EAC is “S”-shaped and has an anterior wall longer than the posterior. The isthmus is a narrowing, not a dilation. Ceruminous glands are present only in the cartilaginous part, not the bony.
Clinical-Based Questions
- A 45-year-old male presents with severe pain and swelling in the outer part of his left external auditory canal, associated with a small boil. On examination, the pinna appears normal, but there is a tender, fluctuant swelling in the cartilaginous part of the EAC. The tympanic membrane is not visualised due to the swelling.
-
- a. What is the most likely diagnosis?
- b. Why is this condition typically confined to the outer part of the EAC?
- c. What is the initial management for this condition?
- A 30-year-old female experiences sudden, severe coughing spells and a sensation of fainting whenever her ear canal is cleaned by her general practitioner. This reflex is consistent each time she has her ears syringed.
-
- a. Which nerve is most likely being stimulated to cause these symptoms?
- b. Explain the anatomical basis for this phenomenon.
- c. What precautions should be taken during her ear cleaning?
- A 6-month-old infant is brought to the clinic with a history of fever and ear discharge. During otoscopic examination, the clinician pulls the pinna upwards, backwards, and laterally but struggles to visualize the tympanic membrane clearly.
-
- a. What anatomical difference in infants might be contributing to the difficulty in visualization?
- b. How should the pinna be manipulated to properly examine an infant’s ear?
- c. Which part of the EAC is underdeveloped in infants?
Answers to Clinical-Based Questions:
- Most likely diagnosis is Furuncle of the External Auditory Canal. b. Furuncles are staphylococcal infections of hair follicles. Hair follicles (and sebaceous/ceruminous glands) are exclusively found in the cartilaginous outer one-third of the EAC, hence the localization. c. Initial management includes local heat application, analgesics, and topical antibiotic ear drops. If fluctuant, incision and drainage may be required. Systemic antibiotics may be given if cellulitis is extensive or the patient is immunocompromised.
- The auricular branch of the vagus nerve (Arnold’s nerve) is most likely being stimulated. b. Arnold’s nerve (a branch of CN X) supplies the posterior and inferior walls of the external auditory canal. Stimulation of this nerve can trigger the vasovagal reflex, leading to parasympathetic overactivity, causing bradycardia, peripheral vasodilation, and subsequent symptoms like coughing, dizziness, and syncope. c. Precautions include gentle instrumentation, using warm (body temperature) water for syringing, and observing the patient closely for any signs of vasovagal response. Stopping the procedure immediately if symptoms occur.
- The bony part of the external auditory canal is underdeveloped in infants. This means the S-shape is less pronounced, and the EAC is relatively straighter and angled differently. b. To properly examine an infant’s ear, the pinna should be pulled downwards, backwards, and laterally. c. The bony inner two-thirds of the EAC, particularly the tympanic part of the temporal bone, is underdeveloped and grows significantly during the first year of life.
FAQ’s in Viva
- What are the three main parts of the external ear? The three main parts of the external ear are the auricle (pinna), the external auditory canal (EAC), and the tympanic membrane (eardrum).
- Why is the pars flaccida clinically important? The pars flaccida is clinically important because it is a weaker part of the tympanic membrane, lacking a strong fibrous layer, making it more prone to retraction pockets and the development of cholesteatoma.
- Which nerve is responsible for the vasovagal reflex during ear cleaning? The auricular branch of the vagus nerve (Arnold’s nerve), which supplies the posterior and inferior walls of the external auditory canal, is responsible for triggering the vasovagal reflex.
- What is the significance of the fissures of Santorini in the EAC? The fissures of Santorini are horizontal deficiencies in the cartilaginous EAC that, while providing flexibility, also act as potential pathways for the spread of infections and neoplasms between the ear canal and adjacent structures like the parotid gland or temporomandibular joint.
- How do you differentiate between the pars tensa and pars flaccida on otoscopy? The pars tensa is the larger, taut, pearly-grey lower portion of the tympanic membrane with a visible cone of light and malleus handle, while the pars flaccida is the smaller, less taut, often pinkish upper portion located above the lateral process of the malleus.
- What is the “cone of light” and where is it seen? The “cone of light” is a bright, triangular reflection seen on the anteroinferior quadrant of a normal, healthy tympanic membrane during otoscopy, radiating from the umbo. Its presence indicates a healthy, mobile TM.
Practical Tips for Viva and Clinical Exams
- Presenting an Otoscopy Finding: Start by describing the external ear (pinna, any lesions), then state how you held the pinna (adult/child technique). Describe the EAC (clear, presence of wax/discharge/foreign body). Finally, describe the TM: color, translucency, cone of light, malleus handle, lateral process, pars tensa/flaccida, any perforations or retractions.
- Common Examiner Questions:
- “What is the significance of the fissures of Santorini?”
- “Why are furuncles only seen in the outer EAC?”
- “How do you distinguish between pars tensa and pars flaccida?”
- “What is the nerve supply of the TM, and what are its clinical implications?”
- “Demonstrate how you would examine a child’s ear.”
- “What causes a vasovagal reflex during ear cleaning?”
- “What are the relations of the EAC?”
- Clinical Scenario Walkthrough: Always think anatomically. If a patient has mastoid pain and EAC sagging, relate it to the posterior relation of the EAC. If they have TMJ pain, consider its anterior relation to the EAC.
———— End ————
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: PPT Free Download, External ear nerve supply, Pinna nerve supply, Ear lobe, Ear lobe, Auricle or pinna, Anatomy of Ear, Muscles & Blood supply of pinna, Fissures of Santorini, Huschke.

Excellent
Thanks
Nice book sir thank you
Thank you Dr. Rahul
Very good for quick revision…very helpfull for exam.
Thanks
Thanks
Thank u
Hello Dr. Tun Tun Myint! 🙏
Thank you so much for your kind message — it truly means a lot! I’m really glad to hear that you found the chapter helpful. It’s always a pleasure to know that the work is reaching and supporting fellow medical professionals, especially from beautiful Myanmar.
Please don’t hesitate to reach out if you ever have questions. Wishing you continued success and joy in your medical journey!
Warm regards,
Dr. Rahul Bagla
Thank you sir
Good book
Thanks
Good job doctor
Well done. Informative and up to date.
Amazing book …easy to understand
Thank you so much professor
Excellent
Thanks