Carcinoma Larynx (Throat Cancer)
Table of Contents
- Overview
- Laryngeal Anatomy
- Risk Factors
- TNM Classification and Staging
- Histological Types
- Spread Patterns
- Clinical Symptoms
- Diagnosis
- Treatment Options
- Post-Laryngectomy Rehabilitation
Overview. Laryngeal cancer (throat cancer) contributes to about 25% of all head and neck cancers and roughly 1% of all global cancers. It typically affects people in their 60s and 70s, and rarely appears before the age of 40. Men are four times more likely to develop it than women (4:1). Both the disease and its treatment often affect the voice, swallowing, and overall quality of the life.
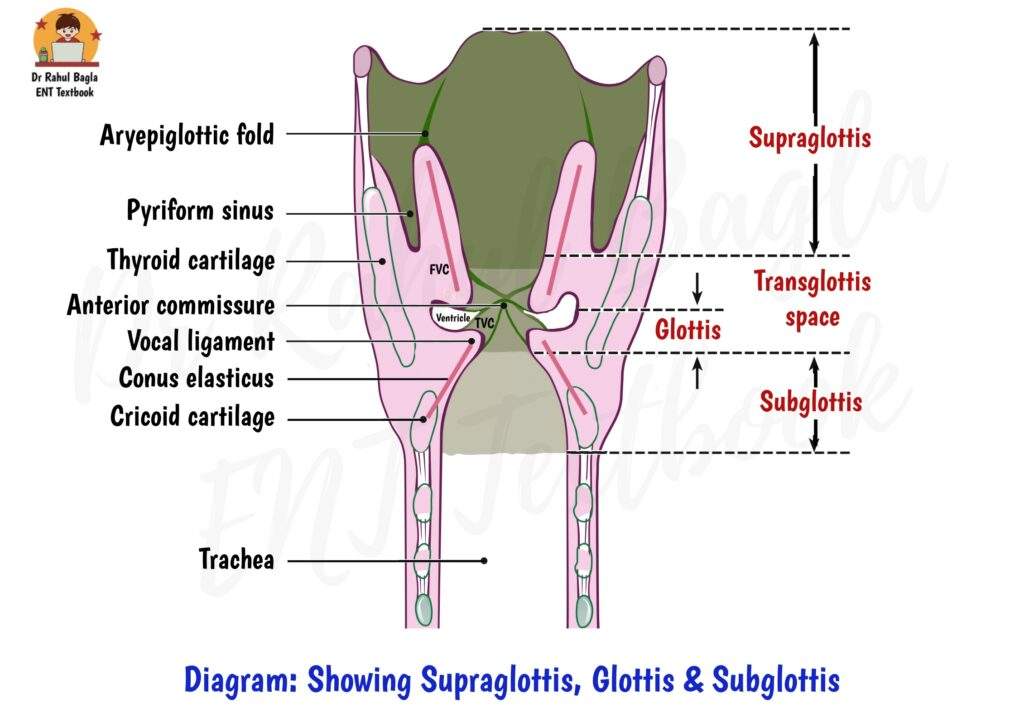
Anatomical Subsites of the Larynx. The larynx is divided into three main sites, each with specific subsites, as per the AJCC 8th Edition. Understanding these is crucial for accurate TNM staging, treatment, and prognosis:
| Site | Location | Extent | Subsites |
|---|---|---|---|
| Supraglottis | Above the vocal cords | From the epiglottis tip to a horizontal line through the ventricle's apex | Suprahyoid & infrahyoid epiglottis, aryepiglottic folds, arytenoids, false vocal cords |
| Glottis | At the level of vocal cords | From the ventricle to 1 cm below the medial free margin of the true vocal cord | True vocal cords, anterior & posterior commissure |
| Subglottis | Below the vocal cords | From 1 cm below the vocal cords to the lower border of the cricoid cartilage | Subglottis to lower border of cricoid cartilage |
Common Risk Factors. Multiple risk factors increase the likelihood of developing laryngeal cancer:
- Smoking introduces carcinogens like nitrosamines, polycyclic aromatic hydrocarbons, nitrosodiethanolamine, nitrosoproline, polonium, carbon monoxide, thiocyanate, hydrogen cyanide, nicotine and metabolites of these constituents. These chemicals damage DNA and RNA, triggering the laryngeal cancer.
- Alcohol enhances the carcinogenic effects of tobacco significantly (approximately 15 times).
- HPV strains (especially HPV-16 and HPV-18) integrate into host DNA and cause its mutations.
- GERD leads to chronic acid irritation of the laryngeal mucosa, raising the risk of laryngeal cancer.
- Occupational exposure. Inhaling substances like asbestos, chromium, or lead at work increases the risk of laryngeal cancer.
- Previous radiation exposure to the head or neck also contributes significantly.
TNM Staging. The TNM system is a globally accepted method to classify and stage cancers, including laryngeal cancer. Developed by the American Joint Committee on Cancer (AJCC), it helps standardise diagnosis, treatment planning, and prognosis. For laryngeal cancer, the 8th AJCC guidelines divide the larynx into three regions, with TNM assessing:
- T: Primary Tumour size and extent (e.g., T1, T2).
- N: Regional lymph Node involvement (e.g., N0, N1).
- M: Presence or absence of distant Metastasis (M0 or M1).
These components combine to assign a stage (I–IV), guiding treatment and predicting outcomes.
TNM classification for cancer larynx (American Joint Committee on Cancer, 8th Edition). The TNM system categorizes laryngeal cancer based on tumour characteristics, lymph node involvement, and metastasis. Here’s a breakdown:
T: Primary Tumour
T-staging Supraglottis Glottis Subglottis
Tx Primary tumour cannot be assessed Primary tumour cannot be assessed Primary tumour cannot be assessed
T0 No evidence of primary tumour No evidence of primary tumour No evidence of primary tumour
Tis Carcinoma in situ Carcinoma in situ Carcinoma in situ
T1 Tumour limited to one subsite of supraglottis with normal vocal cord mobility. Tumour limited to vocal cord(s) (may involve anterior or posterior commissures) with normal mobility.
• 1A Tumour limited to one vocal cord.
• 1B Tumour involves both vocal cords.Tumour limited to the subglottis.
T2 Tumour invades mucosa of more than one adjacent subsites of supraglottis or glottis or region outside the supraglottis
(e.g., mucosa of base of tongue, vallecula, medial wall of pyriform sinus) without fixation of the larynx.Tumour extends to supraglottis and/or subglottis, and/or with impaired vocal cord mobility. Tumour extends to vocal cord(s) with normal or impaired mobility.
T3 Tumour limited to larynx with vocal cord fixation and/or invades any of the following: postcricoid area, pre-epiglottic tissues,paraglottic space and/or minor thyroid cartilage invasion. Tumour limited to the larynx with vocal cord fixation and/or invades paraglottic space and/or minor thyroid cartilage erosion. Tumour limited to larynx with vocal cord fixation.
T4a Tumour invades through the thyroid cartilage and/or invades tissues beyond the larynx (e.g., trachea, soft tissues of neck, including deep extrinsic muscle of tongue, strap muscles, thyroid or oesophagus). Same as T4a supraglottis Same as T4a supraglottis
T4b Tumour invades prevertebral space, encases carotid artery or invades mediastinal structures. Same as T4b supraglottis Same as T4b supraglottis
N: Regional Lymph Nodes
| N Staging (Regional lymph nodes) | Criteria |
|---|---|
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Metastasis in a single ipsilateral lymph node, 3 cm or less in greatest dimension without extranodal extension |
| N2a | Metastasis in a single ipsilateral lymph node more than 3 cm but not more than 6 cm in greatest dimension, without extranodal extension |
| N2b | Metastasis in multiple ipsilateral lymph nodes, none more than 6 cm in greatest dimension, without extranodal extension |
| N2c | Metastasis in bilateral or contralateral lymph nodes, none more than 6 cm in greatest dimension, without extranodal extension |
| N3a | Metastasis in a lymph node more than 6 cm in greatest dimension, without extranodal extension |
| N3b | Metastasis in single or multiple lymph nodes with extranodal extension |
M: Distant Metastasis
| M Staging (Distant Metastasis) | Criteria |
|---|---|
| MX | Distant metastasis cannot be assessed. |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
Laryngeal Cancer Staging. Once TNM is determined, the tumour is grouped into stages (0–IV), reflecting disease severity and guiding treatment. The AJCC 8th Edition staging for laryngeal cancer is:
| Stage | TNM Combination |
|---|---|
| Stage 0 | Tis, N0, M0 |
| Stage I | T1, N0, M0 |
| Stage II | T2, N0, M0 |
| Stage III | T3, N0, M0 or T1–T3, N1, M0 |
| Stage IV | IVA: T4a, N0–N2, M0 or T1–T4a, N2, M0 IVB: T4b, any N, M0 or any T, N3, M0 IVC: Any T, any N, M1 |
Importance of TNM Staging. The TNM system is a cornerstone in laryngeal cancer management. Here’s why it matters:
- Guides Treatment: Early stages (I–II) may use radiotherapy or surgery; advanced stages (III–IV) often require chemoradiotherapy or laryngectomy.
- Predicts Prognosis: Lower stages (I–II) have better outcomes than advanced stages (IV).
- Standardises Diagnosis: Allows global comparison of cases.
- Facilitates Research: Enables consistent evaluation of treatment outcomes across studies.
Histological Types. Identifying the histological type helps guide treatment and prognosis:
- Squamous Cell Carcinoma (SCC): Makes up 85–95% of cases. It grows either outward (exophytic) or inward (endophytic). Histology shows epithelial nests (prickle cells) surrounded by inflammatory stroma and keratin pearls. Cytokeratin (primary marker) confirms the diagnosis.
- Verrucous Carcinoma: A well-differentiated SCC variant with limited nodal spread and favourable outcome.
- Rare Types: Fibrosarcoma, chondrosarcoma, adenocarcinoma, oat cell carcinoma, spindle cell carcinoma, and salivary gland carcinoma.
Spread Patterns of Laryngeal Cancer
Understanding the anatomical site and subsites, and the spread pattern of laryngeal cancer improves diagnosis, treatment planning, and prognosis. Using early warning signs like hoarseness and recognising risk factors can lead to early detection and better outcomes.
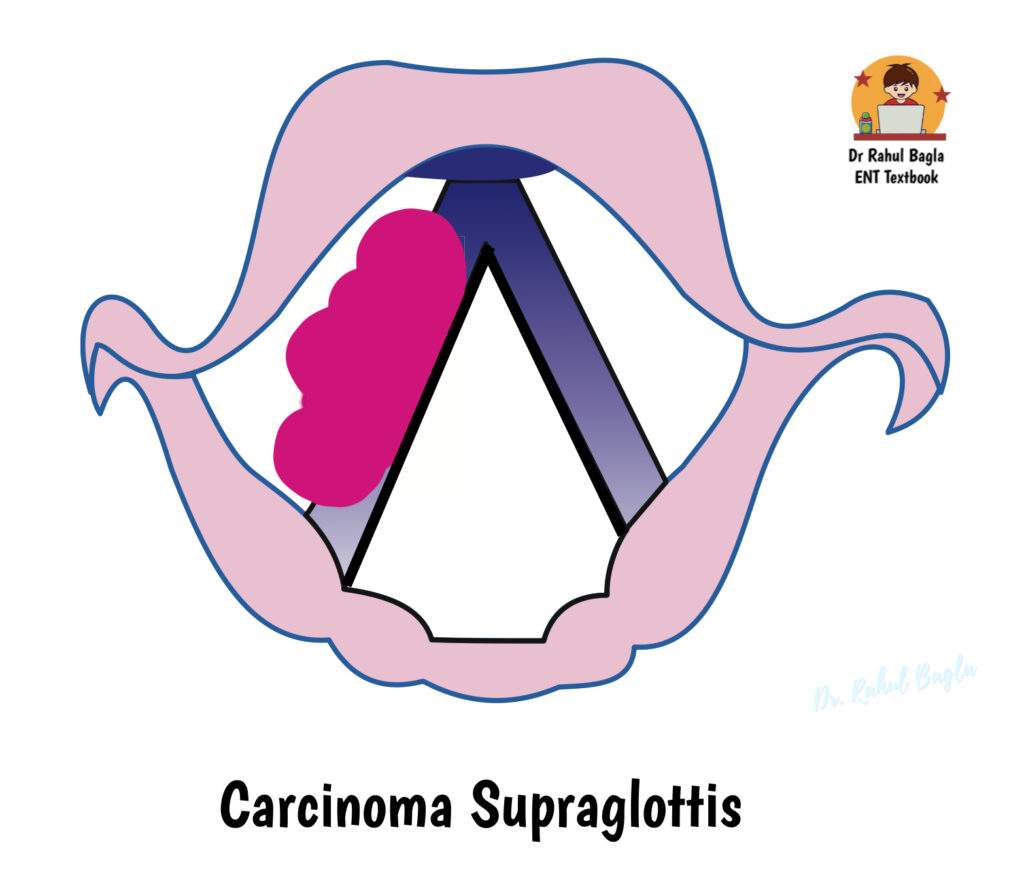
1. Supraglottic Tumours
- These tumours spread aggressively as compared to glottic tumours.
- They invade the pre-epiglottic space via small foramina in epiglottic cartilage.
- From there, they enter the paraglottic space, deep tongue muscles, pyriform sinus, glossoepiglottic fold, and hypopharynx.
- Lymph node metastasis occurs early, affecting upper and middle jugular nodes, often bilaterally (especially epiglottic cancers).
- The hyoid bone rarely gets involved, so surgeons often preserve it during surgery.
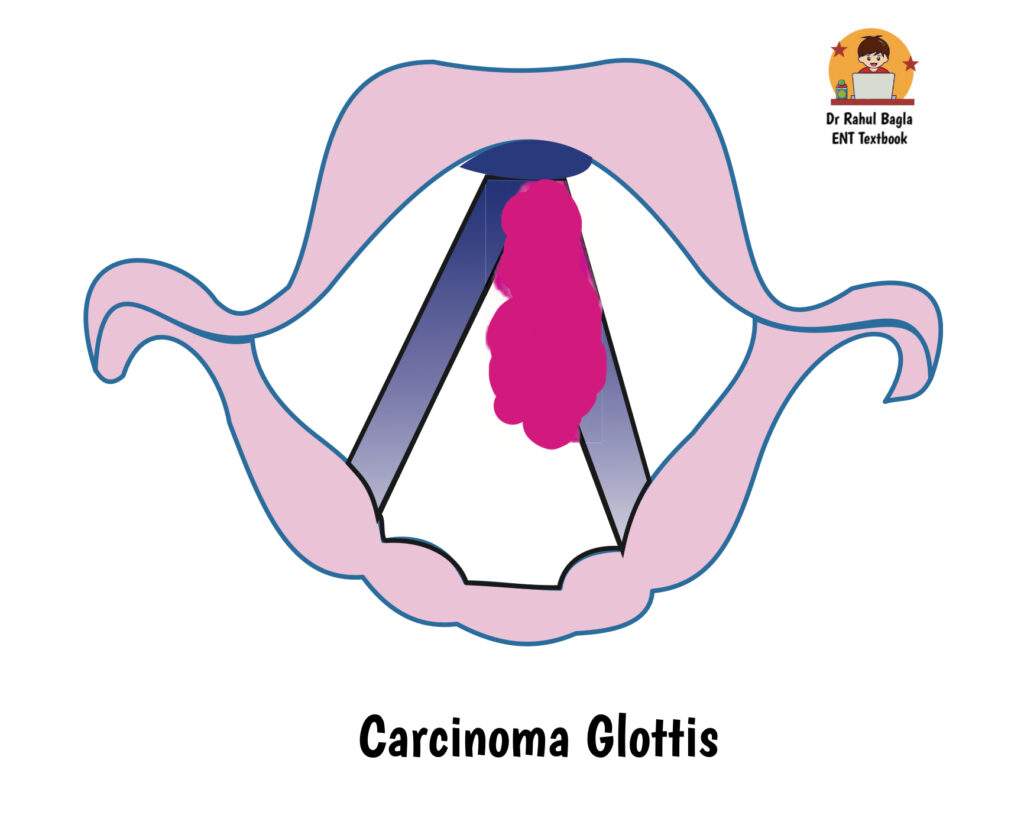
2. Glottic Tumours
- These tumours spread slowly due to a lack of submucosal lymphatics; hence, lymph node metastasis is rare.
- Early spread moves anteriorly to the anterior commissure and the opposite cord.
- Later spread involves posterior movement to the arytenoids, superiorly into the ventricle and false cords, and inferiorly to the subglottis via the cricothyroid membrane.
- Reinke’s space and Broyle’s ligament act as barriers unless tumours cross the vocal ligament and muscle to reach the paraglottic space.
3. Subglottic Tumours
- These tumours are rare and usually result from the inferior extension of glottic cancers.
- They encircle the subglottic region and may invade the thyroid gland, trachea, or oesophagus.
- Lymphatics commonly spread to precricoid (Delphian), paratracheal, and mediastinal nodes.
- Patients often present with stridor due to airway obstruction.
- Hoarseness appears late, as these tumours involve the vocal cords only in advanced stages.

4. Transglottic Tumours
- Transglottic tumours are tumours that extend across the ventricle and involve both true and false vocal cords.
- They spread into the paraglottic space, affecting all laryngeal subsites.
- Their extensive reach often requires aggressive treatment approaches.
Table: Spread of Laryngeal Cancer – Site Wise
| Site | Pattern of Spread | Lymph Node Involvement | Important Points |
|---|---|---|---|
| Supraglottis | - Aggressive spread - Invades pre-epiglottic space via cartilage foramina - Reaches paraglottic space, tongue muscles, pyriform sinus, hypopharynx | - Early nodal spread - Involves upper & middle jugular nodes - Often bilateral (esp. epiglottic tumors) | - Hyoid rarely involved (can be preserved) - Higher rate of lymphatic spread |
| Glottis | - Slow spread due to few submucosal lymphatics - Anterior: anterior commissure & opposite cord - Posterior: arytenoid & ventricle - Downward: subglottis | - Late nodal spread - If involved, affects levels II–VI | - Early hoarseness = early detection - Reinke’s space & Broyle’s ligament limit spread |
| Subglottis | - Often extension of glottic tumors - Circumferential spread - Invades thyroid gland, trachea, or esophagus | - Spreads to Delphian (precricoid), paratracheal & mediastinal nodes | - Rare primary site - Stridor is early clue - Hoarseness appears late |
| Transglottis | - Crosses ventricle - Involves true & false cords - Spreads into paraglottic space and multiple laryngeal subsites | - High nodal risk due to wide spread | - Extensive involvement - Often requires total laryngectomy |
Clinical Presentation of Laryngeal Cancer
Laryngeal cancer usually presents with local symptoms, although it can spread to lymph nodes or distant sites. Systemic signs like weight loss or anaemia appear rarely unless the disease has advanced. Fortunately, distinct early symptoms allow ENT surgeons to identify the red flags.
Key Red Flag Symptoms
- Hoarseness > 3 weeks in a high risk patient
- Persistent throat discomfort or lump sensation
- Unexplained neck swelling
- Voice changes with airway obstruction symptoms
1. Supraglottic Cancer – Often Silent Until Advanced
- Patients may report a globus sensation or a foreign body feeling in the throat in the early stages.
- Small lesions, especially if exophytic, may cause haemoptysis.
- As the tumour grows, voice quality changes to a ‘hot potato’ voice due to impaired articulation.
- Hoarseness occurs when the lesion reaches the vocal cords.
- Referred otalgia, odynophagia, and true dysphagia appear when the tumour invades laterally into the pyriform sinus or pharyngeal walls.
- Many patients remain asymptomatic until the tumour grows large, often presenting first with a neck mass due to cervical lymph node metastasis.
2. Glottic Cancer – Early Voice Change Helps Early Detection
- Hoarseness is the most common symptom and appears early because even minor lesions disturb the vibratory function of the vocal cords. This happens because voice quality depends on the normal structure of the vocal cord epithelium and its superficial lamina propria. However, vocal cord fixation suggests deeper spread (to the thyroarytenoid muscle) and poor prognosis.
- As the tumour grows, patients develop breathiness, reduced phonation time, and possible aspiration, especially if cord fixation occurs.
- Advanced cases cause progressive breathing difficulty, stridor, and airway obstruction.
- Haemoptysis usually indicates a larger or more vascular tumour.
- Referred ear pain (otalgia) through the vagus nerve signals deeper invasion—a warning sign.
- Dysphagia and odynophagia rarely occur unless the tumour extends into adjacent structures like the supraglottis.
- Nodal metastasis is rare unless the disease reaches advanced stages, usually spreading to levels II–VI.
3. Subglottic Cancer – Rare but Easily Missed
- Initial symptoms are vague and often mimic globus pharyngeus or a foreign body sensation.
- As the lesion spreads circumferentially, it causes progressive dyspnoea and stridor due to airway narrowing.
- Always consider subglottic cancer in unexplained vocal cord paralysis, especially in high-risk individuals.
- If the tumour involves the glottis or compresses the recurrent laryngeal nerve, hoarseness and sometimes diplophonia (double voice) may develop.
- Reduced phonation time and vocal fatigue worsen with tumour growth.
- Sometimes, the tumour may invade the thyroid gland, mimicking a thyroid isthmus lesion.
Table: Clinical Presentation of Laryngeal Cancer – Subsite Wise
| Subsite | Early Symptoms | Progressive Symptoms | Late/Advanced Symptoms | Important Clues |
|---|---|---|---|---|
| Supraglottis | - Often silent in early stage - Globus sensation or foreign body feeling - Mild haemoptysis (exophytic lesion) | - ‘Hot potato’ voice due to poor articulation - Hoarseness (when lesion reaches cords) | - Otalgia (referred) - Odynophagia - Dysphagia (if spread to pyriform sinus/pharynx) - Neck mass (nodes) | - Presents late - Lymphatic spread common - Cervical lymph node metastasis may be first sign |
| Glottis | - Early hoarseness (even small lesion affects vibration) - Breathiness - Short phonation | - Aspiration if vocal cord fixation - Strained or breathy voice | - Dyspnoea, stridor (airway narrowing) - Haemoptysis - Referred ear pain (deep invasion) - Rare nodal spread | - Hoarseness = earliest clue - Most common laryngeal cancer - Early detection possible |
| Subglottis | - Vague discomfort - Globus or foreign body feeling | - Hoarseness if glottis or RLN affected - Vocal fatigue - Diplophonia | - Stridor, progressive dyspnoea - Thyroid gland involvement (mimics isthmus lesion) - Unexplained cord paralysis | - Rare site - Missed easily - Think of it in unexplained vocal cord palsy in high-risk individuals |
Diagnosis of Laryngeal Cancer
Early and accurate diagnosis of laryngeal cancer remains crucial for effective treatment. The diagnostic process follows a structured approach involving clinical history, laryngoscopy, imaging, and histopathological confirmation.
- Clinical History
- Head & Neck Local Examination
- Indirect Laryngoscopy
- Laryngoscopy (Flexible or Rigid)
- Imaging (CT/MRI/X-ray)
- Direct Laryngoscopy with Biopsy
- Recurrence Check (PET-CT)
- Ultra-Precise Microlaryngoscopy
- Modern Tools (NBI, Contact Endoscopy)
- Pulmonary Function Tests
1. Clinical History. Start by asking about symptoms. They vary by location:
- Supraglottic lesions may cause difficulty swallowing or a throat lump.
- Glottic lesions often present with persistent hoarseness.
- Subglottic lesions typically lead to progressive dyspnoea and stridor.
Red Flag: If hoarseness lasts >3 weeks in high-risk patients (especially smokers), investigate for cancer.
2. Local Examination. Palpation and inspection of the neck. Look for:
- Laryngeal tenderness or widening. These suggest an extralaryngeal tumour spread through the thyroid cartilage.
- Laryngeal Crepitus. It is a normal grating sensation, felt when moving the larynx side to side. It is because of the cricoid cartilage rubbing against the vertebrae. Loss of crepitus indicates growth in post-cricoid growth, retropharyngeal abscess or mass in the hypopharynx.
- Neck lymph nodes (Levels II–IV, VI): Look for location, number, size, consistency (metastatic nodes are hard; lymphoma nodes are firm and rubbery; hyperplastic nodes are soft), tenderness, fixity to overlying skin or deeper structures and mobility of the lymph nodes.
- Midline swelling. It may suggest spread from the anterior commissure or subglottic region through the cricothyroid membrane.
3. Indirect Laryngoscopy. This basic OPD procedure helps inspect the laryngeal structures using a mirror. Examine the lesion’s appearance, vocal cord mobility, and disease extent.
- Appearance of the Lesion.
- Suprahyoid lesions appear exophytic (outward-growing).
- Infrahyoid lesions usually appear ulcerative.
- Vocal cord lesions may show nodules, thickening, or ulcers.
- Anterior commissure lesions often look like granulation tissue.
- Subglottic lesions typically form raised submucosal nodules, especially in the anterior half.
- Vocal Cord Mobility. If vocal cords show impaired movement or fixation, suspect deeper invasion. Tumours may infiltrate the thyroarytenoid muscle, cricoarytenoid joint or involve the recurrent laryngeal nerve
- Extent of Disease. Always assess if the disease has spread to surrounding structures like the vallecula, base of tongue and the pyriform sinus
4. Flexible/Rigid Laryngoscopy. Compared to mirror laryngoscopy, this method is superior in both comfort and diagnostic accuracy. Use either 70° or 90° rigid telescopes, or a flexible nasolaryngoscope for a detailed view:
- Flexible nasolaryngoscopy, especially in the outpatient clinic, provides a panoramic, high-resolution assessment.
- It helps evaluate vocal cord mobility, mucosal lesions, and tumour extent in real time.
5. Radiological Evaluation. Imaging helps determine tumour size, spread, and involvement of adjacent structures.
- CT Scan (Contrast-Enhanced). It is the investigation of choice for evaluating the extent of tumour subsites, pre-epiglottic space, paraglottic space, cartilage erosion and lymph node metastases. It should be done before the biopsy.
- MRI of the Neck. MRI detects soft-tissue involvement more accurately than CT. Reserve it for cases with suspected recurrence, as it’s more time-consuming and expensive.
- Chest X-Ray or Thoracic CT. Use these to evaluate pulmonary metastases, second primaries, pre-existing tuberculosis, aspiration-related changes and mediastinal lymphadenopathy.
6. PET-CT – Detect Recurrence & Distant Spread. Positron Emission Tomography (PET-CT) plays a selective but crucial role:
- Helps differentiate tumour recurrence from post-radiotherapy oedema.
- Useful in detecting distant metastasis and post-treatment surveillance.
7. Direct Laryngoscopy with Biopsy Under General Anaesthesia. This is the gold standard for diagnosis:
- Offers a complete view of hidden regions like the base of the tongue, anterior commissure, infrahyoid epiglottis, subglottis, and ventricle.
- Essential for assessing tumour extent, cricoarytenoid joint mobility, and obtaining a biopsy.
8. Microlaryngoscopy – High Precision for Small Lesions. Best for early-stage glottic tumours:
- Allows a magnified view under a microscope
- Minimally invasive biopsy
- Helps preserve the voice
9. Newer Diagnostic Tools. Contact endoscopy and narrow-band imaging (NBI) can distinguish carcinoma in situ from invasive cancers. These modalities improve visualisation and margin assessment.
10. Pulmonary Function Tests (PFT). Before planning conservation laryngeal surgery, always assess the respiratory status:
- To ensure that the patient can tolerate surgery and anaesthesia.
- To determine if partial laryngectomy is a feasible option.
Laryngeal Cancer Treatment: Options and Recovery
Laryngeal cancer demands tailored treatments to restore health and function. Options are radiotherapy, surgery, or chemoradiotherapy based on cancer stage. Early-stage treatments prioritise voice preservation, while advanced cases may require total laryngectomy. However, rehabilitation helps patients regain their voice, swallowing, and sense of smell after surgery.
1. Premalignant and Carcinoma in situ (CIS):
- Treatment: CO2 laser stripping.
- Follow-up: Close monitoring to prevent progression.
2. T1 Lesions:
- T1a Glottic:
- Transoral Laser Microsurgery (TLM): Quick recovery, daycare. Minimally impacts swallowing/daily activities.
- Radiotherapy (RT): Weeks of daily sessions, but preserves voice effectively.
- Outcome: Comparable survival rates. Choice based on patient needs/facility. TLM for active individuals, RT if voice is primary concern or anterior commissure involved.
- T1b Lesions (e.g., anterior commissure):
- RT generally yields better voice outcomes than TLM.
3. T2 Lesions
- Survival: Similar rates with RT vs. surgery.
- RT: 25-30% local recurrence. If it recurs, total laryngectomy is often needed (organ preservation is difficult).
- Surgery (TLM/TORS): 7-15% recurrence rates. Quicker recovery than RT.
- Recurrence after surgery: May undergo Open partial laryngectomy (OPL) or repeat TLM/ Transoral robotic surgery (TORS) to preserve the larynx.
- Combining surgery with RT in recurrent cases enhances control.
4. T3 Lesions
- Preferred: Chemoradiotherapy (preserves larynx, effective cancer control).
- Alternative (if Chemoradiotherapy is not available/ patients who decline Chemoradiotherapy): OPL, TLM, or TORS (surgical options).
5. T4a Lesions
- Treatment: Total Laryngectomy (due to cartilage invasion, dysfunctional larynx).
- Voice prosthesis is inserted post-surgery for speech.
- Postoperative RT: Enhances control, especially with nodal disease.
- Indications for Total Laryngectomy (T4a and others):
- T4a tumours with bone or cartilage invasion.
- Involved nodes > 3 cm, multiple positive nodes, extranodal spread.
- Extension into the neck soft tissue.
- Subglottic extension of the primary tumour.
- Key: Pre-op counselling is vital; laryngectomy impacts voice/breathing. Postoperative RT addresses residual disease. Neck dissections manage nodal involvement.
Treatment Options by Cancer Stage.
| Stage | Treatment Options | Key Features |
|---|---|---|
| Premalignant/CIS | CO2 Laser Stripping | Outpatient procedure, close follow-up |
| T1a Glottic | Transoral laser microsurgery (TLM), Radiotherapy (RT) | TLM: Day-care, quick recovery; RT: Weeks of treatment, good voice |
| T1b Glottic | RT, TLM | RT preferred for better voice outcomes |
| T2 | RT, TLM, Transoral robotic surgery (TORS) | RT: 25–30% recurrence; Surgery: 7–15% recurrence |
| T3 | Chemoradiotherapy, Open partial laryngectomy (OPL), TLM, TORS | Chemoradiotherapy preserves larynx; surgery for select cases |
| T4a | Total Laryngectomy, RT | Addresses cartilage invasion; voice prosthesis used |
Nodal Disease Management
- Modified neck dissections for nodal disease.
- For T3 and T4a supraglottic cancers: Bilateral elective neck dissections (clear levels II–IV) to control metastatic spread.
Radiotherapy Complications. Radiotherapy treats early lesions but causes complications.
- Mucositis
- Xerostomia
- Radionecrosis
- Hypothyroidism
- Odynophagia
- Laryngeal oedema
- Stricture and fibrosis.
Patients require supportive care to manage side effects. Supportive therapies like hydration and pain management ease symptoms. However, long-term effects like fibrosis need ongoing care.
Challenges After Laryngectomy – Rehabilitation
Total laryngectomy causes major changes (loss of voice, smell, taste, swallowing/ breathing issues). Consequently, rehabilitation becomes essential for recovery. Moreover, preoperative counselling prepares patients for these changes. Clinicians address these issues through tailored rehabilitation. However, patients need support to adapt to tracheostoma care. Therefore, meeting laryngectomized individuals offers practical insights. Additionally, therapy improves swallowing and communication. These efforts restore function and confidence.
1. Pulmonary Rehabilitation: Heat and moisture exchangers (HMEs) restore airway humidification post-laryngectomy. They act as artificial noses, warming and filtering air to reduce dryness. Clinicians attach HMEs to the stoma using adhesive tape. Consequently, patients experience less coughing and discomfort. Moreover, HMEs improve breathing comfort. Therefore, they are vital for pulmonary rehabilitation. HMEs use calcium chloride-impregnated filters for moisture retention. However, patients need guidance on proper use. Therefore, clinicians provide training for stoma care. Additionally, regular HME replacement ensures effectiveness. These steps enhance respiratory health.
2. Swallowing Rehabilitation: Laryngectomy disrupts normal swallowing. Clinicians preserve pharyngeal mucosa during surgery to create a wide neopharynx. This reduces dysphagia by easing bolus passage. Consequently, patients swallow more comfortably. Moreover, therapy strengthens swallowing muscles. Therefore, preserving the mucosa is critical for effortless swallowing. A constricted neopharynx increases swallowing effort. However, therapy and surgical planning minimise this issue. Therefore, clinicians assess swallowing function post-surgery. Additionally, dietary adjustments support recovery.
3. Smell Rehabilitation: Laryngectomy bypasses the nose, limiting active smelling. Clinicians teach the nasal airflow-inducing manoeuvre (NAIM), or polite yawning, to restore smell. Patients lower their jaw with their lips closed to draw air into the nasal cavity. Consequently, this stimulates the olfactory mucosa. Moreover, about 30% of patients regain passive smelling. Therefore, NAIM improves sensory function. NAIM is simple but requires practice. However, it significantly enhances the quality of life. Therefore, clinicians provide training sessions. Additionally, patients benefit from sensory therapy. These efforts restore sensory experiences.
4. Voice Rehabilitation Options: Three main methods: oesophageal speech, electrolarynx, tracheoesophageal puncture (TEP). Patients choose based on their needs.
-
Oesophageal Speech. Clinicians teach oesophageal speech to produce a natural voice without devices. Patients swallow air and release it to vibrate the neopharynx. This method offers pitch control and hands-free speech. Consequently, it’s cost-effective and safe. However, only 5–25% of patients succeed due to training demands. Intensive therapy supports oesophageal speech development. However, a limited air reservoir shortens sentences. Therefore, clinicians provide ongoing support. Additionally, patients practice articulation for clarity. These efforts yield natural communication.
-
Electrolarynx devices vibrate neck tissues to produce speech. Clinicians recommend them for immediate communication. They’re easy to use, benefiting patients struggling with other methods. Consequently, an electrolarynx suits older patients. However, the robotic voice and high costs are drawbacks. Therefore, clinicians assess patient dexterity before prescribing. Patients hold the device against their neck for speech. However, battery replacement adds ongoing costs. Therefore, training ensures effective use. Moreover, telephonic speech remains challenging. These factors influence patient satisfaction.
-
Tracheoesophageal Puncture (TEP). Clinicians perform TEP to create a fistula between the trachea and oesophagus. A silicone prosthesis, like Blom-Singer or Provox, shunts lung air to vibrate the neopharynx. This produces natural, long-lasting speech. Primary TEP occurs during laryngectomy, while secondary TEP follows later. Consequently, TEP offers hands-free communication. However, complications like leakage arise. Cricopharyngeal myotomy prevents muscle spasms during TEP speech. However, Candida overgrowth or prosthesis replacement needs monitoring. Therefore, clinicians provide maintenance training. Moreover, TEP’s natural voice enhances patient confidence. These benefits make TEP popular.
———— End of the chapter ————
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Cummings, Otolaryngology-Head and Neck Surgery.
- Stell and Maran’s, Textbook of Head and Neck Surgery and Oncology.
- Ballenger’s, Otorhinolaryngology Head And Neck Surgery
- Susan Standring, Gray’s Anatomy.
- Frank H. Netter, Atlas of Human Anatomy.
- B.D. Chaurasiya, Human Anatomy.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery.
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Ganong’s Review of Medical Physiology.
- Guyton & Hall Textbook of Medical Physiology.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page:https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Juvenile Angiofibroma. https://www.entlecture.com/juvenile-angiofibroma/
- Please read. Tumours of Hypopharynx . https://www.entlecture.com/tumours-of-the-hypopharynx/
- Please read. Anatomy of Oesophagus. https://www.entlecture.com/anatomy-of-oesophagus/
Frequently asked questions
- What are the early signs of laryngeal cancer?
- How is throat cancer diagnosed in the early stages?
- How does smoking cause laryngeal cancer?
- What is transoral laser microsurgery for throat cancer?
- Symptoms of supraglottic laryngeal cancer
- How to regain speech after laryngectomy?
- Tracheoesophageal puncture for voice restoration
- Nasal airflow-inducing manoeuvre for smell rehabilitation
- What are the symptoms of laryngeal cancer?
- What causes throat cancer?
- How is laryngeal cancer diagnosed?
- What are the treatment options for throat cancer?
- Can laryngeal cancer be cured?
- What is the survival rate for laryngeal cancer?
- How does smoking affect laryngeal cancer risk?
- What is a laryngectomy, and how does it affect speech?
- How to recover speech after throat cancer surgery?
- What are the side effects of radiotherapy for throat cancer?
- \What is the role of HPV in laryngeal cancer?
- How to manage swallowing problems after laryngectomy?
- What is the difference between glottic and supraglottic cancer?
- How does laryngeal cancer spread to lymph nodes?
- What is the best treatment for early-stage throat cancer?
Keywords:Discover the causes, symptoms, histological types, and spread of larynx (throat) cancer. Learn how early signs help improve survival and treatment options. Laryngeal cancer, Vocal cord cancer, Throat cancer symptoms, Glottic carcinoma, Subglottic tumour, Supraglottic tumour, Early signs of throat cancer, Risk factors for laryngeal cancer, Vocal cord tumour symptoms, Laryngeal cancer, Throat cancer, Larynx cancer, Head and neck cancer, Laryngeal cancer symptoms, Throat cancer treatment, Laryngeal cancer causes, Laryngeal cancer diagnosis, Voice rehabilitation, Neck dissection, Radiotherapy complications, What are the early signs of laryngeal cancer? How is throat cancer diagnosed in the early stages? Laryngeal cancer treatment options for T1 lesions, Post-laryngectomy rehabilitation techniques, How does smoking cause laryngeal cancer? What is transoral laser microsurgery for throat cancer? Symptoms of supraglottic laryngeal cancer How to regain speech after laryngectomy? Tracheoesophageal puncture for voice restoration Nasal airflow-inducing maneuver for smell rehabilitationWhat are the symptoms of laryngeal cancer?What causes throat cancer?How is laryngeal cancer diagnosed?What are the treatment options for throat cancer?Can laryngeal cancer be cured?What is the survival rate for laryngeal cancer?How does smoking affect laryngeal cancer risk?What is a laryngectomy and how does it affect speech?How to recover speech after throat cancer surgery?What are the side effects of radiotherapy for throat cancer?What is the role of HPV in laryngeal cancer?How to manage swallowing problems after laryngectomy?What is the difference between glottic and supraglottic cancer?How does laryngeal cancer spread to lymph nodes?What is the best treatment for early-stage throat cancer?
