Mastoidectomy
Mastoidectomy involves the surgical eradication of disease from the middle ear cleft, which includes the mastoid antrum, mastoid air cells, middle ear, and Eustachian tube.
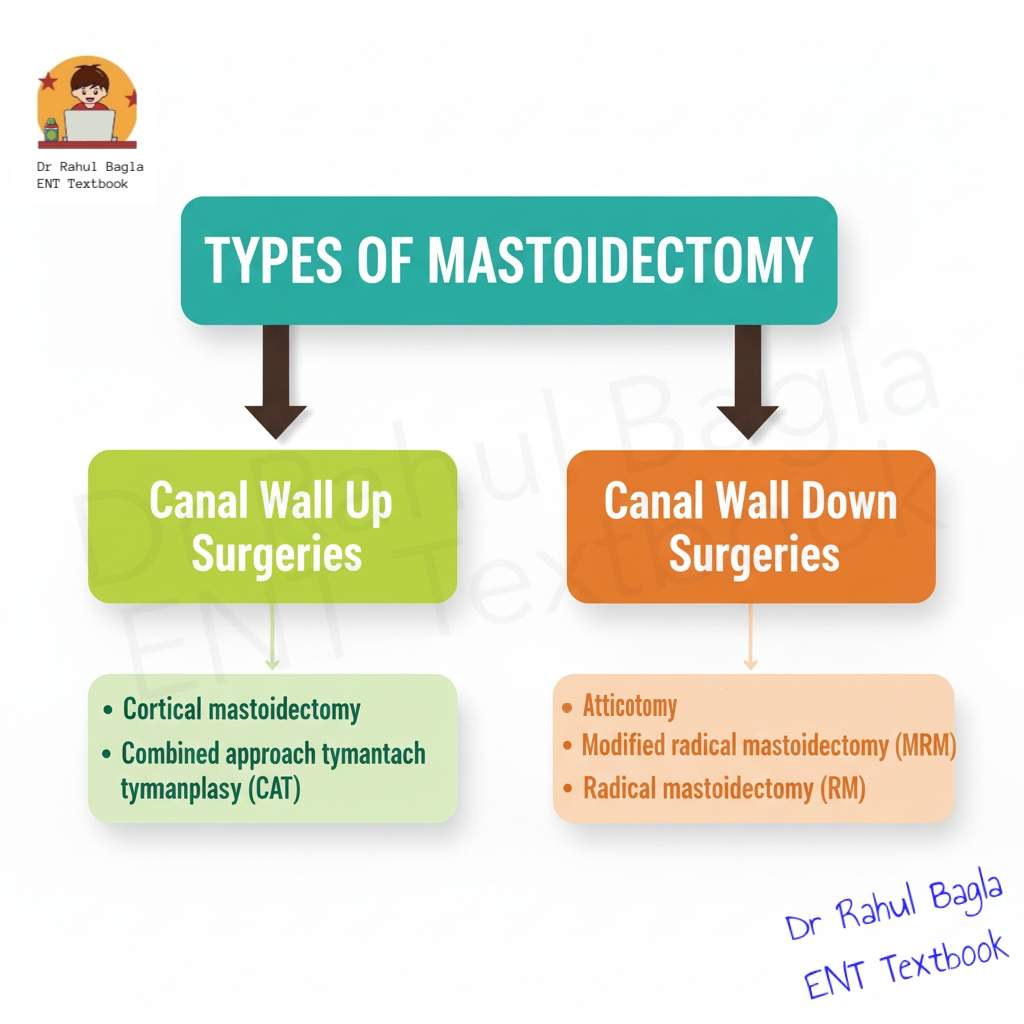
Classification of Mastoidectomy
There are two broad classifications of mastoidectomy based on the status of the posterior EAC wall, which forms the common boundary between the mastoid and the middle ear.
- Canal Wall Up (CWU) Surgery: The posterior EAC wall is preserved. It includes cortical mastoidectomy and combined approach tympanoplasty (CAT).
- Canal Wall Down (CWD) Surgery: The posterior EAC wall is removed. It includes atticotomy, modified radical mastoidectomy (MRM) and radical mastoidectomy (RM).
Canal Wall Up (CWU) Surgeries.
The posterior bony ear canal wall is preserved during the CWU surgery. It is comparatively difficult to perform. The advantage of CWU is, it avoids the creation of an open mastoid cavity, thus eliminating the associated long-term cavity problems like discharge and debris accumulation. The disadvantage of CWU is, higher risk of residual disease due to incomplete visualisation of all anatomical areas. Consequently, this often necessitates a “second-look” surgery 12–18 months later to check for and remove any remaining disease.
1. Cortical Mastoidectomy (Simple Mastoidectomy or Schwartz Procedure): 🔗Read more:
2. Combined Approach Tympanoplasty (CAT): It was started by Jansen in 1960. Surgery involves cortical mastoidectomy with tympanoplasty and a posterior tympanotomy. Posterior tympanotomy is the creation of a small window in the facial recess area to inspect and remove disease from the middle ear. This approach offers a good view of the sinus tympani and posterior mesotympanum. The facial recess is a crucial surgical landmark and a common ENT viva question. It forms a triangular area bounded by:
- Medially: The mastoid segment of the facial nerve.
- Laterally: The chorda tympani nerve.
- Superiorly: The fossa incudis (the area lodging the short process of the incus).
- Clinical Relevance: Surgeons use the facial recess approach for the insertion of cochlear implant electrodes.
Table: Differences Between Canal Wall Up (CWU) and Canal Wall Down (CWD) Surgery
| Feature | Canal Wall Up (CWU) Surgery | Canal Wall Down (CWD) Surgery |
|---|---|---|
| Posterior Canal Wall | Preserved. | Removed. |
| Surgical Access | Limited/Difficult (Visualization of hidden areas is poor). | Excellent/Wide (Ensures complete disease eradication). |
| Mastoid Cavity | No open mastoid cavity is created. | Creates an open mastoid cavity (requires meatoplasty). |
| Long-Term Problems | Eliminated (No discharge, debris accumulation). | Prone to 5 D's (Debris, Discharge, Dependence, Deafness, Dizziness). |
| Residual Disease | Higher risk, therefore often necessitates a "second-look" surgery. | Lower risk, consequently "second-look" surgery is usually not required. |
| Hearing Aim | Preserved/Improved (Better functional results). | Sacrificed (RM) or Preserved/Reconstructed (MRM). |
| Difficulty | Technically more challenging. | Easier technically due to wide exposure. |
| Examples | Cortical Mastoidectomy, Combined Approach Tympanoplasty (CAT). | Modified Radical Mastoidectomy (MRM), Radical Mastoidectomy (RM), Atticoantrotomy. |
Canal Wall Down (CWD) Surgeries.
The posterior bony ear canal wall is removed during the CWD surgery.
Table: Advantages and Disadvantages of CWD Surgery
| Feature | Advantage | Disadvantage |
|---|---|---|
| Access | Provides excellent surgical access, thereby ensuring complete disease eradication and minimizing the chance of residual disease. | Creates a mastoid cavity that can lead to lifelong problems. |
| Recurrence | Offers low recurrence rate for cholesteatoma. | Consequently, patients may face persistent ear discharge, debris, and conductive hearing loss. |
| Follow-up | Thus, it eliminates the need for a "second-look" surgery. | Requires regular, lifelong follow-up for cleaning. |
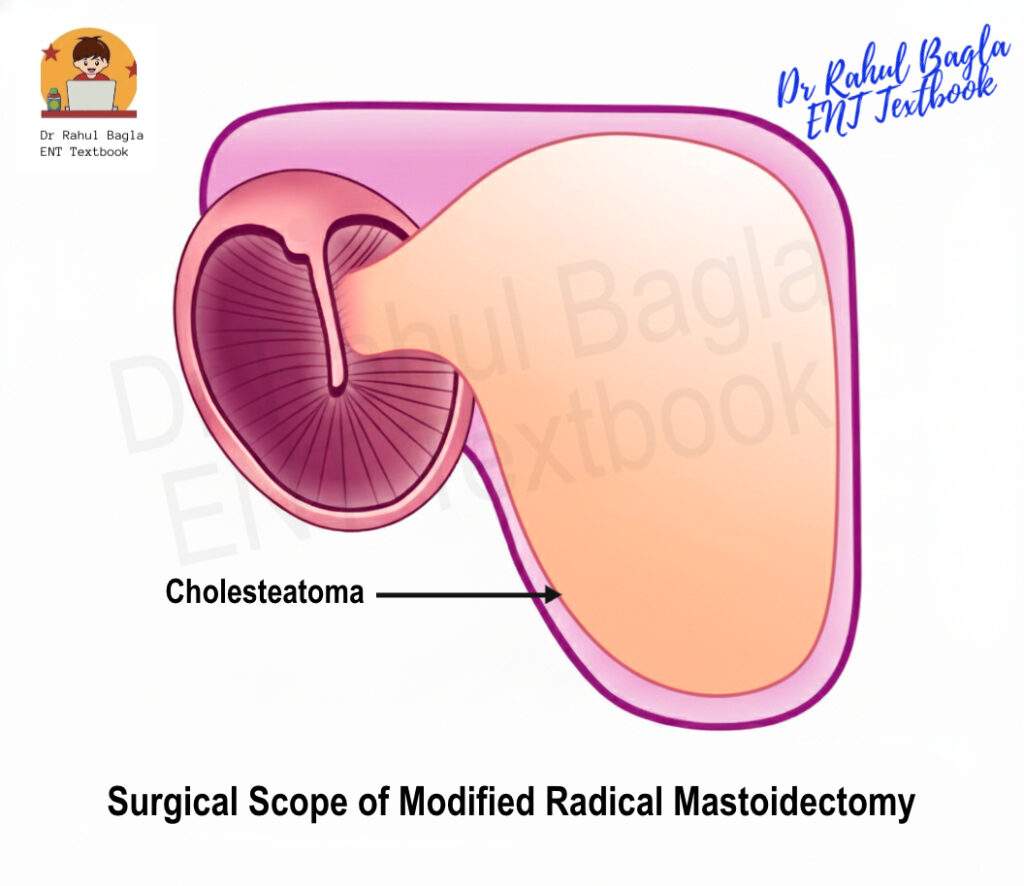
1. Modified Radical Mastoidectomy (MRM). Also known as canal wall down mastoidectomy, it is the preferred surgery for atticoantral chronic otitis media with cholesteatoma. The goal of this surgery is to completely eradicate disease from the middle ear cleft and create a single, safe, and dry self-cleansing cavity, while preserving healthy middle ear structures for future reconstruction.
Indications:
- Cholesteatoma with recurrent discharge and a good cochlear reserve for future hearing reconstruction.
- When a canal wall up procedure is difficult due to a small, sclerotic mastoid or an inexperienced surgeon.
- Extensive disease in only the hearing ear
- Damaged posterior canal wall
- Labyrinthine fistula
- Patient is not willing to come for regular follow-up.
- CSOM is associated with severe complications.
Contraindications
- Benign chronic otorrhea with a central perforation and without cholesteatoma.
- Acute otitis media with coalescent mastoiditis.
- Persistent secretory otitis media.
- Tubercular otitis media.
Surgical Steps:
1. Mastoid Exenteration: Initial steps are similar to cortical mastoidectomy, clearing the mastoid air cells.
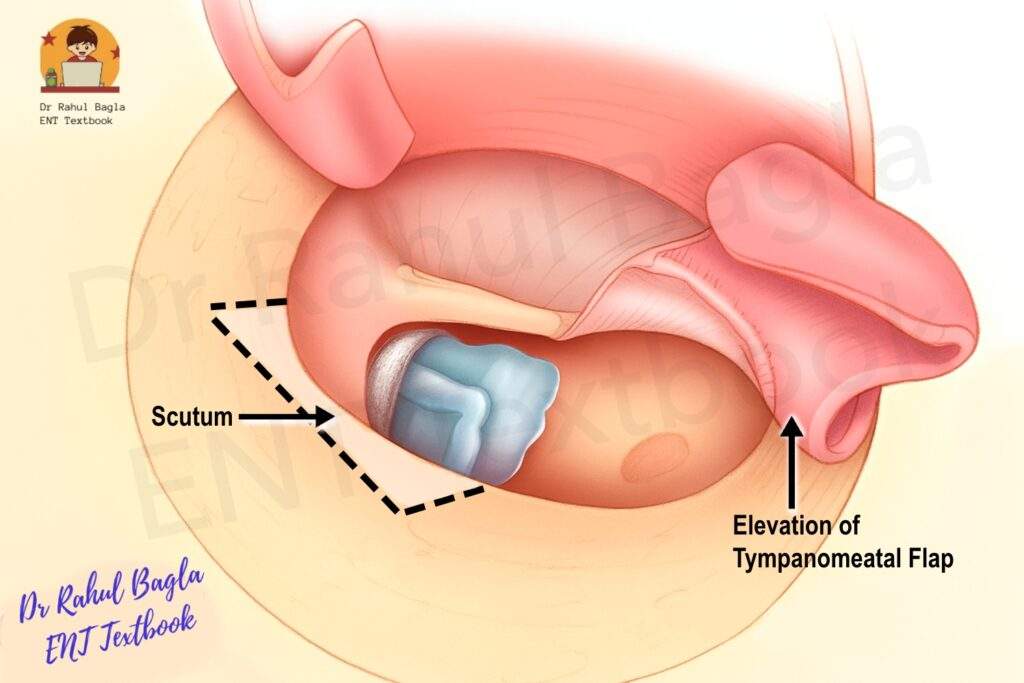
2. Elevation of the tympanomeatal flap. A flap composed of the tympanic membrane and canal wall skin is elevated to expose the middle ear.
3. Removal of scutum. The lateral attic wall (scutum) is removed to ensure complete exposure of the ossicular chain, an area frequently involved in cholesteatoma
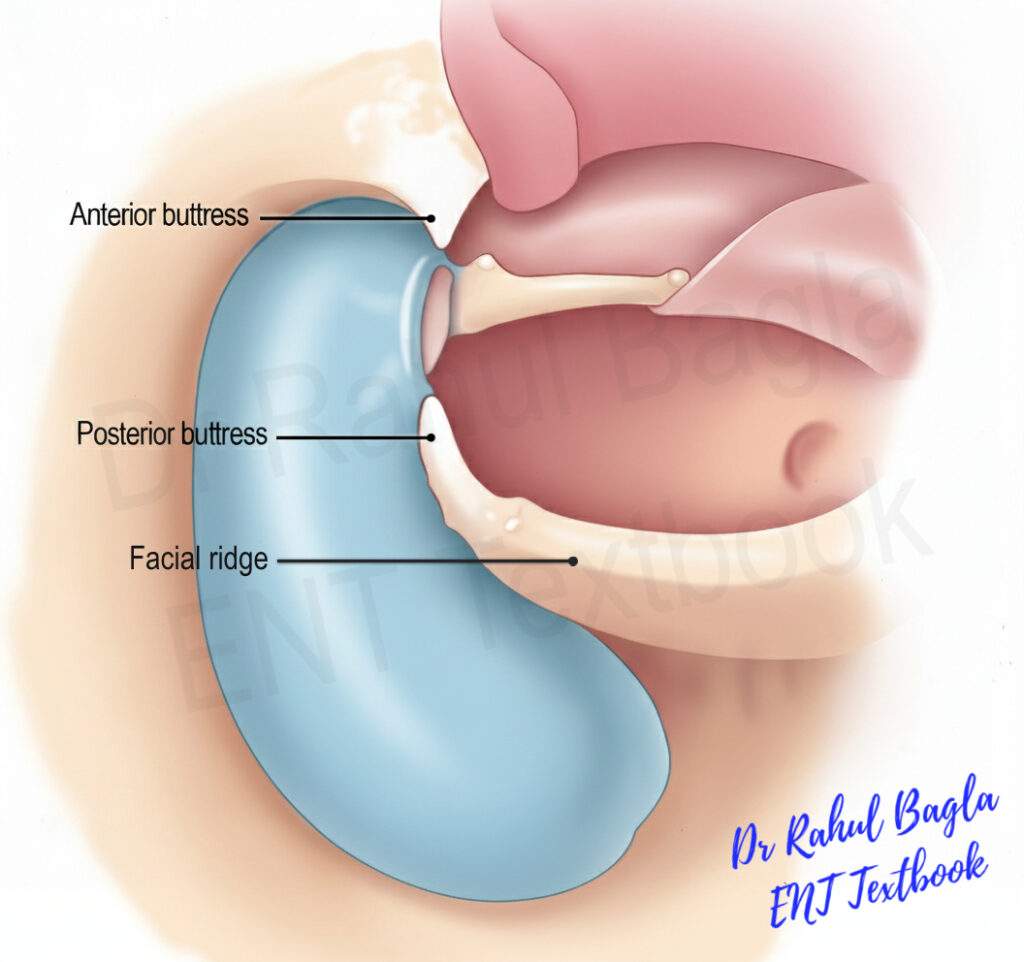
4. The bridge is broken. The bridge is the bony arch overlying the epitympanum (between the anterior and posterior buttresses), is systematically removed using a cutting burr with suction-irrigation, taking care to protect the underlying ossicles.
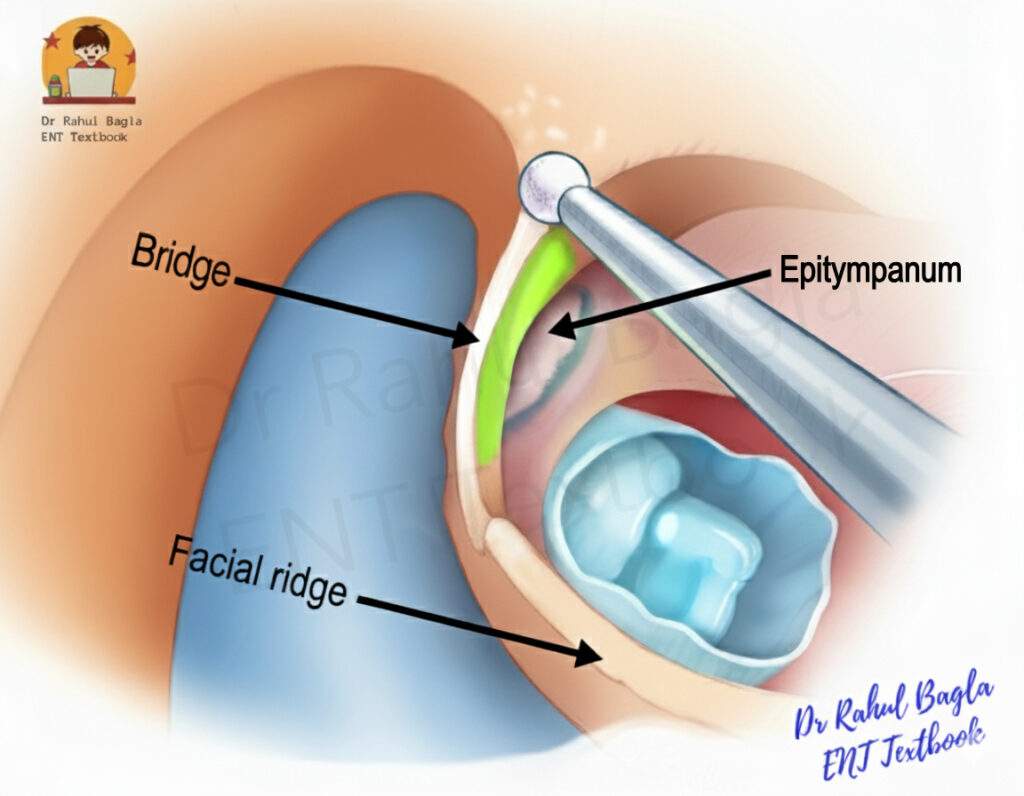
5. Removal of Buttresses: Both the anterior (projection of bone at the junction of the anterior bony meatal wall and epitympanic tegmen) and posterior (projection of bone at the junction of the posterior wall and the floor of the meatus) buttresses are removed to create a smooth transition from the mastoid to the external auditory canal.
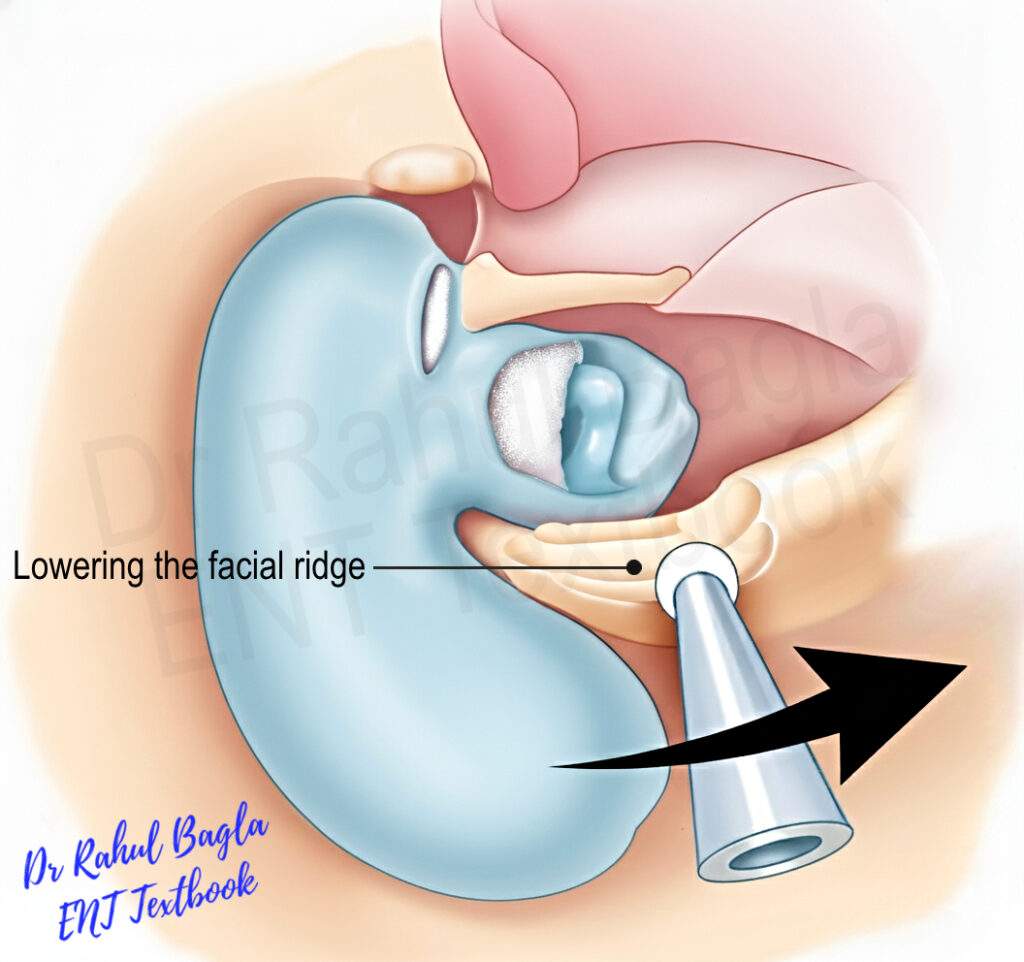
6. Facial Ridge is Lowered: This is the defining and most critical step. The facial ridge (posterior canal wall, lateral to the mastoid segment of the facial nerve) is meticulously lowered with suction irrigation using a cutting burr initially and a diamond burr later, always working parallel to the fallopian canal. Avoid excessive drilling that may expose or injure the facial nerve (the most common site of injury during mastoid surgeries is this mastoid segment, specifically the second genu area). Lower the facial ridge up to the level of the lateral semicircular canal and external auditory canal floor. Concomitantly, the chorda tympani nerve is sacrificed along with the posterior wall, which results in a temporary or permanent change in taste on that side of the tongue.
7. Formation of the mastoid cavity: Adequate lowering (removal of the posterior canal wall) ensures a common cavity between the mastoid antrum and middle ear. It helps to obtain a smooth, saucerized, reverse pyramid shape cavity with no overhanging ridges. It provides adequate exposure of the middle ear structures for disease clearance. However, the downside is that a larger cavity, known as a mastoid cavity, is left behind, which can lead to long-term problems such as debris, wax, or discharge buildup.
8. Disease Clearance: All residual pathological tissue is meticulously removed from every recess of the middle ear cleft, including the epitympanum, mesotympanum, protympanum, retrotympanum, and hypotympanum. Particular attention is directed toward hidden regions such as the sino-dural angle (Citelli’s angle), sinus tympani, and facial recess. This often necessitates the use of a Buckingham mirror or an angled endoscope.
9. Reconstruction of hearing mechanism. After clearing the disease, focus on restoring the patient’s hearing. Pars tensa of the tympanic membrane and the middle ear, if healthy, are left undisturbed. If the disease extends into the middle ear, only the irreversible tissues are removed. Ossicles may be removed if diseased or partially necrosed, or if the cholesteatoma is going medial to the ossicles. In these cases, it’s impossible to clear the disease without taking out the ossicles. Reconstruction of the hearing mechanism is done. Ossiculoplasty may be done in the same sitting or as a second-stage (better results) procedure. The second stage of surgery is done after 6 to 9 months.
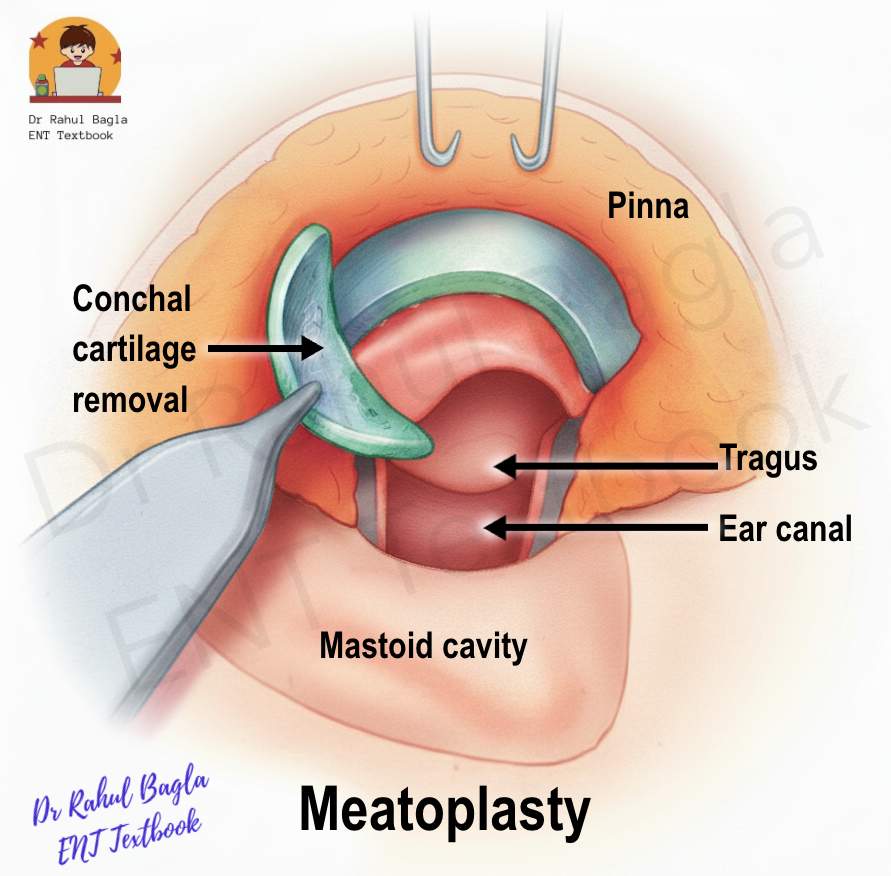
10. Meatoplasty: It is mandatory for all canal wall down procedures. The large mastoid cavity formed is then exteriorised by performing meatoplasty. It involves enlarging the external auditory meatus to allow for proper ventilation, drainage, and easy postoperative cleaning. A skin flap based laterally at the concha is raised from the posterior and superior ear canal walls. They then turn this flap back into the mastoid cavity to cover the area of the facial ridge, which helps in epithelization of the cavity. Sometimes, a small piece of conchal cartilage can be removed to further enlarge the opening, making it even easier to access the cavity.
 11. Closure of the wound in layers is done.
11. Closure of the wound in layers is done.
12. These entire steps of surgery are typically a “back-to-front” (posterior-to-anterior) approach. In cases with less extensive disease, a “front-to-back” (anterior-to-posterior or atticotomy) approach may be used to create a smaller cavity, which reduces the post-operative cavity problems.
Complications of MRM:
- Facial nerve injury: Facial nerve injury occurs in about 1–2% of MRM cases, most commonly at the second genu. If paralysis appears postoperatively, wait 4 hours if local anaesthesia was used. If the surgeon is not sure about the facial nerve injury during surgery, first remove the ear pack (which may be compressing the fallopian canal). If paralysis persists, immediately explore the fallopian canal for decompression, end-to-end anastomosis or cable grafting (using greater auricular, lateral femoral cutaneous, or sural nerve). If the surgeon is confident there is no intraoperative injury, give steroids and observe for 2 weeks.
- Horizontal semicircular canal injury: Injury to the lateral semicircular canal can occur while drilling the dural plate. Bone dust is placed over the defect, and a facial covering is placed over it.
- Cavity problems: 20% of patients have problems of discharging mastoid cavity, which is due to either infection, high facial ridge, tympanic membrane perforation, residual disease or recurrence.
- Sensorineural hearing loss
- Perichondritis of pinna
- Injury to dura
- Injury to sigmoid sinus
- Wound infection.
2. Radical Mastoidectomy
Radical mastoidectomy (RM) is the most extensive canal-wall-down surgery aimed at completely removing disease from the middle ear and mastoid. As the name implies, this surgery is radical in that it involves the removal of all structures—both healthy and diseased. This includes the entire tympanic membrane, middle ear mucosa, and ossicles (except the stapes footplate), and sealing the Eustachian tube to prevent future ingrowth of mucosa or infections from the nasopharynx. The Eustachian Tube (ET) is sealed using septal cartilage, ossicles, bone chips, muscle or fascia.
The mastoid, middle ear, and EAC are converted into a single large cavity that remains permanently exteriorised via the external auditory meatus for inspection and cleaning. The goal is safety—achieving a safe, dry, and easily inspectable cavity—rather than preserving or improving hearing. Unlike Modified radical mastoidectomy (MRM), Radical mastoidectomy does not involve reconstruction of hearing or grafting and is now rarely performed.
Indications for Radical Mastoidectomy. Presently, indications for the procedure are limited.
- Extensive/Unresectable disease: Cholesteatoma invading the eustachian tube, round window niche, perilabyrinthine or hypotympanic cells.
- Revision surgery: If previous attempts to eradicate chronic inflammatory disease or cholesteatoma have failed.
- Preoperative dead ear with non-serviceable hearing (e.g., >90 dB HL) in an elderly patient.
- Carcinoma of the external and middle ear. Often followed by radiotherapy, offering a robust alternative to partial temporal bone resection.
- As an approach to the petrous apex.
- Removal of a glomus tumour.
- A cochlear promontory fistula.
Steps of Radical Mastoidectomy
- Canal wall down procedure: Initial steps are similar to modified radical mastoidectomy.
- Removal of ossicles: Disarticulate the incudostapedial joint first and cut the tensor tympani muscle tendon. Then remove the malleus and incus using alligator forceps. Retain the stapes footplate to prevent perilymphatic leakage and inner ear damage.
- Removal of the Middle ear mucosa and TM: Remove the entire TM and annulus. Strip all mucosal remnants from the protympanum, hypotympanum floor, and promontory.
- Hypotympanum: Remove the inferior bony annulus to make the floor of the EAC and the hypotympanum cavity at the same level.
- Seal the Eustachian Tube: Curette the mucosa around the ET orifice to prevent epithelial ingrowth. Then, permanently seal (obliterate) the opening using autologous materials like a piece of muscle (temporalis fascia), cartilage chips (tragal or septal), or bone chips. This blocks the primary route for recurrent infection from the nasopharynx.
- Cavity formation and meatoplasty: Create a smooth, self-cleaning surface with no overhanging edges to avoid epithelial pearl formation and debris accumulation. Perform a wide meatoplasty to allow easy post-operative cleaning and inspection.
- Dressing and Closure: Pack the cavity with absorbable material (e.g., Gelfoam or antibiotic-impregnated gauze) and close the post-aural wound in two layers.
Differences between Radical Mastoidectomy (RM) vs. Modified Radical Mastoidectomy (MRM)
| Feature | Radical Mastoidectomy (RM) | Modified Radical Mastoidectomy (MRM) |
|---|---|---|
| Middle Ear Mucosa | Completely Exenterated. | Preserved in the mesotympanum/hypotympanum. |
| Tympanic Membrane | Totally Removed (No Grafting). | Preserved (Grafted if perforated - Tympanoplasty). |
| Ossicles | Stapes footplate only retained. | Preserved if healthy; reconstructive options employed. |
| Eustachian Tube | Permanently Obliterated. | Usually preserved (unless disease necessitates closure). |
| Hearing | Sacrificed/Unimproved (Focus on safety). | Preserved/Improved (Aim for serviceability). |
3. Atticotomy and Atticoantrostomy
These are the most conservative CWD procedures, aiming to create a smaller cavity and reduce postoperative problems.
Atticotomy is done to remove cholesteatoma (disease) limited to the attic (epitympanic space) region of the middle ear. It is generally sufficient for small lesions situated lateral to the incus body and malleus head. The procedure requires removal of the outer attic wall (scutum) and a portion of the posterosuperior canal wall. This procedure can be done with an endaural, postauricular, or transcanal endoscopic approach. After the disease is cleared, an atticoplasty is performed to repair the scutum. This involves using a cartilage (tragal or conchal), which is supported by any remaining ossicular heads or abundant gelfoam to prevent its medialization.

The extent of the surgery depends on the disease’s invasion depth:
- Atticotomy Alone: Used for limited disease.
- Anterior Atticotomy: The attic opened first, then extended to the antrum and mastoid cells.
- Posterior Approach: Mastoidectomy is done first, then attic is reached via the mastoid cavity.
Overall, atticotomy is considered a reliable treatment offering good morphological and functional results for epitympanic cholesteatoma. The decision to perform atticotomy alone or combine it with a mastoidectomy is based on preoperative findings (CT scans and tympanic membrane examination) and operative findings.
Atticoantrostomy: Atticoantrostomy is a surgical extension of an atticotomy, representing a relatively conservative technique used when ear disease has spread from the middle ear attic into the mastoid antrum. It is typically performed in the posterior direction (from attic to antrum) through the transmeatal route (through the ear canal) to establish better drainage and ventilation for the upper middle ear and mastoid region. The walls of the lateral attic and aditus are removed. The procedure then involves gradually removing the posterosuperior bony ear canal wall to widen the access into the antrum. In a sclerotic mastoid (characterised by dense bone and poor air cell development) and a small antrum, the atticoantrotomy creates a small cavity with smooth walls. In contrast, in a well-developed, large cell system (characterised by good pneumatization), the procedure results in a larger cavity.
A few terminologies associated with the atticoantrotomy are:
- Bondy’s Operation: This term refers to an atticoantrotomy performed without entering the middle ear space. It is highly conservative, aiming solely at the disease in the attic and antrum while preserving the middle ear structures.
- Atticoantrostomy (Conservative Radical Operation): This term is used when the middle ear is entered during the surgery. It represents a slightly less conservative approach necessary for more widespread disease, but still aims to retain functional middle ear structures where possible.
Comparison to Tympanomastoidectomy
When the ear disease is widespread and has extended beyond the antrum into multiple mastoid air cells, a more extensive tympanomastoidectomy is required. This larger surgery effectively encompasses all the major steps of a Modified Radical Mastoidectomy (MRM), which include:
- Lowering the facial ridge
- Removing the anterior and posterior buttresses.
- Thoroughly inspecting all hidden areas of the middle ear cleft.
- Performing a wide meatoplasty (enlarging the ear canal opening).
The extensive bone removal in a tympanomastoidectomy creates a larger, single surgical cavity, and its associated complication risks are comparable to those of an MRM.
Transcanal Endoscopic Mastoidectomy
A significant recent development is the Transcanal Endoscopic Mastoidectomy for managing active squamous COM. This technique uses small, high-definition rigid endoscopes (0 and 30-degree scopes) inserted through the ear canal. The surgical approach is similar to the “inside-out” or anterior-to-posterior technique performed under a microscope.
The advantages are:
- The resulting cavity is much smaller, as less bone is removed.
- The angled endoscopes provide superior visualisation of notoriously hidden areas, such as the sinus tympani, protympanum, and hypotympanum, ensuring complete disease removal.
However, it is a single-handed technique (one hand holds the scope, the other operates), making it relatively challenging and requiring a steep learning curve.
Managing Postoperative Mastoid Cavity
A mastoid cavity is the open space left in the temporal bone after a Canal Wall Down (CWD) surgery (like a Modified Radical Mastoidectomy). While necessary for clearing the disease, it can lead to various complications, both immediately after surgery and throughout the patient’s life.
The Discharging Mastoid Cavity: When a mastoid cavity continues to produce discharge for more than 6–12 weeks post-operation, it is termed a discharging mastoid cavity. Several factors contribute to this persistent problem:
- Surgical: High facial ridge (not lowered enough), Inadequate meatoplasty (ear canal opening is too small, causing poor ventilation/drainage), or Residual disease left behind during the operation.
- Anatomical: A large mastoid cavity (greater than 3 cc) and a perforation in the tympanic membrane (eardrum) increase the risk.
Lifelong Issues: The 5 D’s of the Mastoid Cavity: Even when the cavity is successfully kept dry, the physical changes are permanent and lead to a set of chronic, lifelong issues known as the 5 D’s:
- Debris: The skin lining the new cavity does not shed and clean itself properly, leading to the collection of squamous debris (dead skin flakes).
- Discharge: The debris often gets infected when water enters the cavity (during swimming or bathing) or when the ear is exposed to extensive moisture (like during monsoon season), causing the cavity to start discharging.
- Dependence: Patients must regularly visit for cleaning of the cavity, particularly to remove built-up wax and debris.
- Deafness: The removal of the bony posterior canal wall increases the volume of the middle ear space, which can contribute to conductive hearing loss.
- Dizziness: Since the protective bony covering over the lateral semicircular canal (a balance organ) may be exposed, sudden temperature changes (e.g., cold air, cold water) entering the cavity can stimulate the canal (caloric stimulation), causing temporary feelings of dizziness.
Strategies to Reduce Cavity Problems: Preventing long-term issues is a crucial part of the surgery and follow-up. Problems with the mastoid cavity can be significantly reduced through both improved surgical technique and reconstructive procedures:
- Optimising Surgical Technique: The best defence is performing a “good” operation, which includes complete disease removal, saucerization (creating smooth, rounded walls), performing an adequate meatoplasty, and sufficiently lowering the facial ridge.
- Minimally Invasive Techniques: Using techniques like inside-out mastoidectomy or transcanal endoscopic mastoidectomy results in smaller cavities (due to less bone removal), which heal faster and have a lower rate of long-term problems.
- Mastoid Cavity Obliteration: For large cavities that are highly prone to discharge, the space can be filled in (obliterated) to reduce its size. This is achieved using various grafting materials:
- Pedicled Flaps: Tissues that remain attached to their original blood supply, such as the temporalis muscle flap (Rambo’s) or musculo-periosteal flap (Palva’s).
- Free Grafts: Pieces of tissue or synthetic materials like hydroxyapatite, bone, or cartilage.
- Posterior Canal Wall Reconstruction: Instead of leaving an open cavity, the removed posterior canal wall can be rebuilt using cartilage or prosthetic materials (e.g., porous hydroxyapatite, ceramic). This converts the CWD procedure back into a Canal Wall Up configuration, eliminating the cavity entirely.
———End of Chapter———-
High-Yield Points for Quick Revision (NEET PG MCQs)
- The facial recess is a triangular space bounded by the facial nerve (medially), chorda tympani (laterally), and fossa incudis (superiorly).
- Combined Approach Tympanoplasty (CAT) preserves the canal wall and uses a posterior tympanotomy via the facial recess.
- Modified Radical Mastoidectomy (MRM) is the most common surgery for cholesteatoma. Its goal is safe ear + hearing preservation/reconstruction.
- The Facial Ridge Lowering is the defining step of MRM. Injury most commonly occurs at the second genu of the facial nerve.
- Meatoplasty is mandatory for all Canal Wall Down procedures to ensure drainage, ventilation, and cleaning.
- Radical Mastoidectomy (RM) prioritises a safe, dry ear at the expense of hearing. The Eustachian tube is permanently obliterated.
- Atticotomy is for cholesteatoma limited to the attic; it involves removing the scutum.
- Bondy’s Operation is an atticoantrotomy without entering the middle ear.
- The 5 D’s describe the lifelong challenges of an open mastoid cavity.
Clinical Scenarios and Viva Voce
Scenario 1: Case Presentation and Management
A 35-year-old male presents with a right-sided, foul-smelling ear discharge for 5 years and progressively decreasing hearing. Otoscopy shows a posterosuperior marginal perforation with white, cheesy discharge. Audiometry reveals a moderate conductive hearing loss with a bone conduction threshold of 20 dB. CT scan shows an expansile soft tissue mass in the attic and mastoid antrum.
Viva Questions and Answers:
- Q: What is your diagnosis?
- A: Chronic Otitis Media (COM), Squamous type (Atticoantral disease) with cholesteatoma.
- Q: What is the definitive management plan?
- A: Modified Radical Mastoidectomy (MRM) with ossicular chain reconstruction (Tympanoplasty type III or IV) because he has a good cochlear reserve (20 dB BC). Alternatively, a CWU procedure like CAT could be considered; however, MRM offers better disease clearance for extensive cholesteatoma.
- Q: Why do you prefer MRM over RM in this case?
- A: We prefer MRM because the patient has serviceable hearing (BC 20 dB), and MRM preserves and reconstructs healthy middle ear structures, unlike RM, which sacrifices them.
Scenario 2: Postoperative Complication
A patient undergoes an MRM for cholesteatoma. On the first postoperative day, the patient had complete ipsilateral facial paralysis.
Viva Questions and Answers:
- Q: What is the most likely cause and location of the injury?
- A: Intraoperative facial nerve injury, most likely at the second genu during the crucial step of facial ridge lowering.
- Q: What is your immediate course of action?
- A: If local anaesthesia was used, wait for up to 4 hours. If paralysis persists or if general anaesthesia was used, immediately explore the operative field. If the surgeon is confident the nerve was cut or exposed, perform facial nerve decompression and immediate repair (e.g., end-to-end anastomosis or cable grafting).
Multiple Choice Questions (MCQs) for NEET PG
- Which of the following structures is preserved in a standard Modified Radical Mastoidectomy (MRM)? A. Entire middle ear mucosa B. Stapes superstructure C. Stapes footplate D. Entire tympanic membrane
- The most common site of injury to the facial nerve during mastoidectomy is the: A. Labyrinthine segment B. Tympanic segment C. Second genu/Mastoid segment D. Exit at the stylomastoid foramen
- Which surgical step is mandatory in all Canal Wall Down procedures? A. Ossiculoplasty B. Tympanoplasty C. Facial ridge reconstruction D. Meatoplasty
- In Radical Mastoidectomy, the Eustachian tube is obliterated primarily to prevent: A. Hearing loss B. Facial nerve injury C. Recurrent infection from the nasopharynx D. CSF leak
- The facial recess is bounded laterally by the: A. Facial nerve B. Chorda tympani nerve C. Fossa incudis D. Lateral semicircular canal
- The term “Bondy’s Operation” is a type of: A. Radical Mastoidectomy B. Simple Mastoidectomy C. Atticoantrotomy without middle ear entry D. Combined Approach Tympanoplasty
- The primary advantage of Canal Wall Up surgery is: A. Lower recurrence rate B. Avoidance of a mastoid cavity C. Superior access to hidden areas D. Elimination of the need for tympanoplasty
- Which of the following is NOT one of the 5 D’s of a mastoid cavity? A. Debris B. Dizziness C. Delay D. Dependence
- A high facial ridge in a postoperative mastoid cavity primarily predisposes the patient to: A. Labyrinthine fistula B. Sensorineural hearing loss C. Discharging mastoid cavity D. Sigmoid sinus thrombosis
- The most significant development aiding visualisation of the sinus tympani and hypotympanum in contemporary mastoidectomy is the use of: A. High-power microscope B. Operating loupes C. Angled endoscopes D. Surgical lasers
Answers and Explanations:
- C. In RM, all structures are removed except the stapes footplate. In MRM, more is preserved.
- C. The facial ridge lowering step involves drilling around the mastoid segment and second genu.
- D. Meatoplasty is essential for ventilation and cleaning of the newly created cavity.
- C. The nasopharynx is a source of infection via the Eustachian tube.
- B. Facial nerve (medial), Chorda tympani (lateral), Fossa incudis (superior).
- C. Bondy’s is the most conservative CWD procedure, focused on the attic/antrum only.
- B. The main appeal of CWU is the preservation of normal anatomy, avoiding the open cavity.
- C. The 5 D’s are Debris, Discharge, Dependence, Deafness, and Dizziness.
- C. A high facial ridge creates an overhanging edge that hinders drainage and self-cleansing, leading to discharge.
- C. Angled endoscopes provide a panoramic view of “hidden” recesses that the straight view of the microscope cannot reach.
Frequently Asked Questions in Viva
- What is the main difference between Canal Wall Up and Canal Wall Down mastoidectomy? Canal Wall Up preserves the bony posterior ear canal wall, while Canal Wall Down removes it, creating a mastoid cavity.
- What is the most crucial step in a Modified Radical Mastoidectomy (MRM)? Lowering the facial ridge is the most critical and defining step, done to create a smooth, self-cleansing cavity.
- Why is a second-look surgery often required after a Canal Wall Up procedure? A second-look surgery is necessary to check for and remove any residual cholesteatoma because the canal wall preservation hinders complete visualisation of all hidden areas during the initial surgery.
- What are the 5 D’s of the mastoid cavity? The 5 D’s are Debris, Discharge, Dependence, Deafness, and Dizziness, which are chronic issues associated with an open mastoid cavity.
- When is Radical Mastoidectomy performed instead of Modified Radical Mastoidectomy? Radical Mastoidectomy is reserved for extensive, non-resectable disease (like cholesteatoma invading the Eustachian tube or for carcinoma), where the primary goal is safety over hearing preservation.
———–End————-
Download the full PDF Link:
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Mastoidectomy, Canal Wall Down (CWD), Canal Wall Up (CWU), Modified Radical Mastoidectomy (MRM), Cortical Mastoidectomy, Pathology, Cholesteatoma (High Volume), Chronic Otitis Media (COM) Surgery, Mastoiditis, Atticoantral Disease, Mastoid Antrum, Macewen’s Triangle, Sinodural Angle, Trautmann’s Triangle, Facial Nerve in Mastoidectomy, Mastoid Surgery Indications, Mastoidectomy PG MCQ, Post-op care after mastoidectomy, Complications of Mastoidectomy, Related Surgery, Tympanomastoidectomy, Tympanoplasty Type V, Mastoid Obliteration Techniques, ENT topics for NEET PG, mastoidectomy surgery, MBBS ENT notes, ENT viva questions, canal wall up vs canal wall down mastoidectomy, cortical mastoidectomy steps, modified radical mastoidectomy notes, ENT PG preparation, otology surgery guide, mastoid cavity problems, Canal Wall Down vs Canal Wall Up mastoidectomy, Complications of mastoidectomy, Mastoid cavity 5 D’s, Radical Mastoidectomy indications, CBME curriculum ENT surgery
