Anatomy of the Labyrinth
A clear understanding of labyrinth anatomy is essential to understanding otosclerosis, as the disease primarily targets the bony capsule. Therefore, let’s review the three main components of the labyrinth.
- Otic (Membranous or Endolymphatic) Labyrinth
- It includes: utricle, saccule, cochlear duct, semicircular ducts, and the endolymphatic duct and sac.
- It is filled with endolymph, a specialised fluid that helps transmit sound vibrations (hearing) and maintain equilibrium (balance).
- Periotic Labyrinth (Perilymphatic Space)
- It surrounds the membranous labyrinth.
- It includes: vestibule, scala vestibuli and scala tympani, perilymphatic regions of the semicircular canals, and periotic duct.
- It is filled with perilymph, which acts as a protective cushion for the delicate structures inside.
- Otic Capsule (Bony Labyrinth).
- Endosteal layer (innermost layer, lining the inner surface).
- Enchondral layer. This middle layer originates from cartilage, which later ossifies into bone. Within this layer, small islands of cartilage may remain unossified, potentially contributing to the development of otosclerosis.
- Periosteal layer (outermost layer, covering the outer surface).
Key Embryology: Otic capsule ossifies from 14 centres, the first one appears in the area of the cochlea at around the 16th week of foetal development, and the last one appears in the posterior semicircular canal around the 20th week.
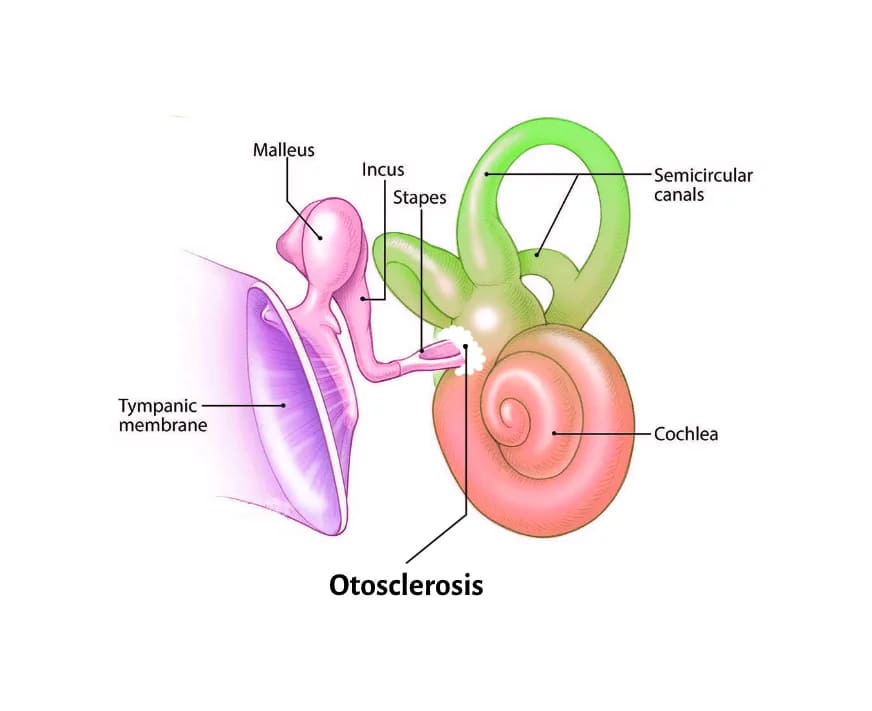
What is otosclerosis?
Otosclerosis, also known as otospongiosis, is a localised bone disorder that affects the enchondral layer of the bony labyrinth. Instead of maintaining its normal dense structure, the bone remodels abnormally into one or more foci of irregular spongy bone. These foci, due to some non-specified factors, are activated to form highly vascular new spongy bone. It usually involves the stapedio-vestibular joint, leading to fixation or ankylosis of the stapes footplate and resulting in conductive hearing loss. If the process reaches the cochlea, it may also lead to sensorineural hearing loss.
 Pathogenesis
Pathogenesis
Otosclerosis is a common hereditary disease of localised bone. Osteoclasts remove normal laminar bone and replace it is replaced by the unorganised spongy interwoven cancellous bone that is greater in thickness, vascularity, and cellularity.
Aetiology
Although the exact cause of otosclerosis remains unknown, several contributing factors have been proposed:
- Anatomical Factors: Otosclerosis often targets specific regions in the inner ear, especially around the oval window.
- Genetic Predisposition: 50% of all cases report a positive family history, suggesting a strong genetic component. The rest are sporadic. Otosclerosis is inherited in an autosomal dominant pattern.
- Viral Infection: Some studies suggest a viral trigger, particularly involving the measles virus. Evidence shows lower levels of anti-measles antibodies in the blood but higher concentrations in the inner ear fluid (perilymph). Given the similarities between otosclerosis and Paget’s disease- another condition thought to have a viral origin – this theory holds considerable weight.
- Autoimmune Mechanism: Elevated antibodies against Type II and Type IX collagen have been detected in patients with otosclerosis. This suggests that the immune system might mistakenly attack the body’s own tissues, contributing to bone changes in the ear.
- Gender: In India, otosclerosis appears more frequently in women (2:1), indicating a possible gender-related susceptibility.
- Race. White races are affected more than black Americans. It is common in Indians but rare among Chinese and Japanese.
- Age of Onset: Symptoms usually begin between the ages of 20 and 30, often starting with gradual hearing loss.
- Van der Hoeve Syndrome: This rare genetic condition presents a triad of features: osteogenesis imperfecta, otosclerosis, and blue-tinted sclera. It is associated with mutations in the gene that produces Type I collagen.
- Hormonal Influence: Hormonal changes during puberty, pregnancy, or menopause may worsen the condition. This further supports the idea that hormones play a role in the progression of otosclerosis.

Types of otosclerosis
Otosclerosis can be classified into three main types based on the areas it affects:
- Stapedial (Clinical) Otosclerosis: This is the most common type and affects the stapes bone and the stapedio-vestibular joint, causing conductive deafness.
These include:- Fissula ante fenestram, located in front of the oval window and it is the common site for stapedial otosclerosis.
- Fissula post fenestram, found behind it.
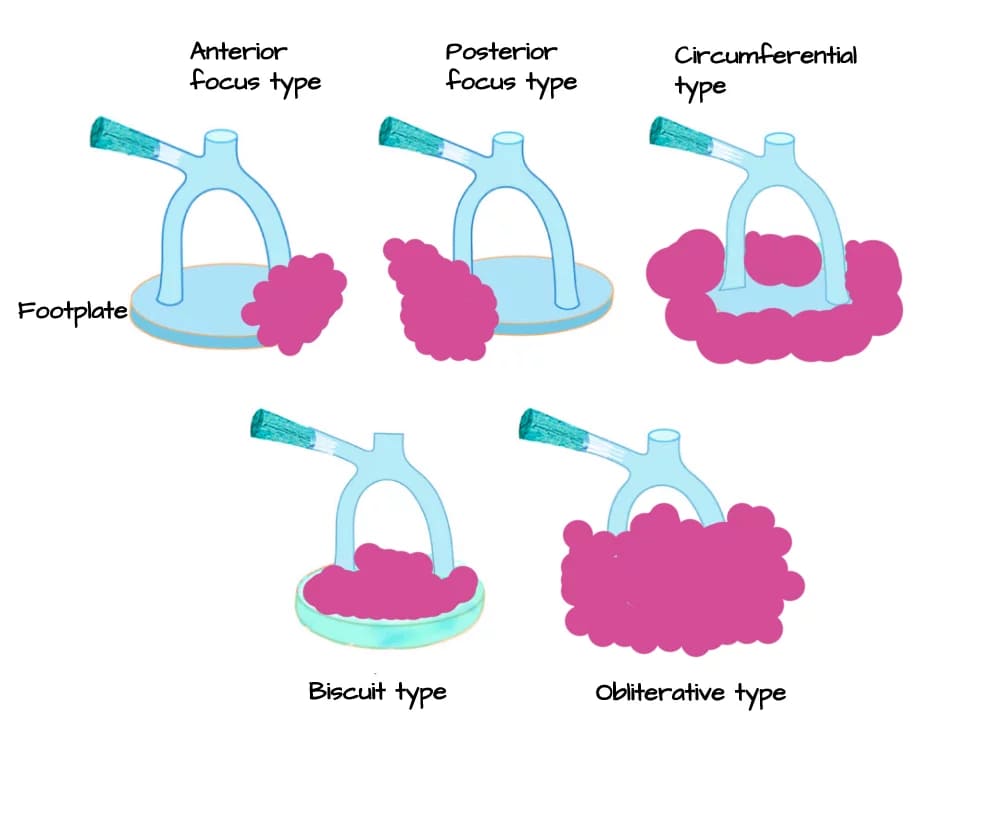
- In stapedial otosclerosis, the disease may involve the entire stapes footplate (circumferential type), spare the annular ligament while affecting the footplate (biscuit type), or block the oval window entirely (obliterative type).
- Cochlear Otosclerosis: In this type, the condition affects the bony layer lining the cochlea (called the cochlear endosteum) without affecting the stapes or the stapedio-vestibular joint, causing pure sensorineural hearing loss with no conductive element.
- Histologic Otosclerosis: This type causes microscopic changes in the bone but does not affect hearing, as neither the stapes nor the cochlear structures are involved. Since it produces no symptoms, it is usually discovered only during post-mortem examination. Despite being silent, it serves as the gold standard for determining the true incidence of otosclerosis in the population.
Diagram: Types of stapedial otosclerosis
Symptoms of Otosclerosis
1. Hearing Loss: One of the earliest and most common symptoms is slow, painless, and progressive hearing loss that typically begins in early adulthood (20–30 years). It can present in different forms:
- Conductive hearing loss occurs when sound is unable to pass efficiently through the middle ear. This may result from stapes fixation (especially at the back part of the annular ligament), fixation of the malleus bone, complete obliteration of the round window niche or cavitating otosclerosis (third window effect).
- Sensorineural hearing loss, though less common, may develop when toxic materials enter the inner ear. Damage to the cochlear endosteum can lead to atrophy and scarring (hyalinization) of the spiral ligament.
- Mixed hearing loss is also possible when both conductive and sensorineural components are involved.
- Paracusis Willisii: This is a characteristic symptom where the patient paradoxically feels they hear better in noisy environments. This happens because other people tend to speak louder in noisy environments, making it easier for the affected individual to follow conversations.
2. Speech Changes: Many patients develop a soft, well-modulated voice. This occurs because enhanced bone conduction makes their own voice sound louder to them, leading them to speak more quietly.
3. Tinnitus: Ringing or buzzing in the ears, known as tinnitus, is especially common in cochlear otosclerosis and during active phases of the disease.
4. Vertigo: While otosclerosis does not usually cause vertigo, some patients may experience it. In some cases, this may be due to an unrelated condition such as Meniere’s disease. However, if vertigo is triggered by loud noises or activities like the Valsalva manoeuvre (forceful exhalation), it may suggest the presence of a “third window” disorder, such as superior semi-circular canal dehiscence.
Signs
1. Tympanic Membrane: The tympanic membrane is quite normal and mobile.
2. Schwartze Sign (Flamingo Flush): This is an uncommon but classic sign where a reddish or flushed hue is visible on the promontory through the tympanic membrane. This sign is highly indicative of an active, highly vascular otospongiotic focus and is seen in approximately 10% of patients.

Schwartz sign/flamingo flush
Investigations
A variety of clinical tests and imaging studies help in diagnosing otosclerosis. These investigations evaluate both middle and inner ear function to determine the type and extent of hearing loss.
- Otoscopy: The eardrum usually appears normal and remains mobile. However, in some cases, a reddish or flushed area may be visible on the promontory through the tympanic membrane. This sign, known as Schwartze sign or flamingo flush, indicates increased blood flow to the area.
- Tuning fork tests
- Rinne Test: This test helps compare air conduction (AC) and bone conduction (BC). In otosclerosis, Rinne’s test becomes negative—meaning BC is greater than AC. Initially, this is observed with lower frequencies like 256 Hz and 512 Hz, but as stapes fixation progresses, it becomes evident at higher frequencies such as 1026 Hz.
- Weber Test: Sound from the tuning fork tends to be heard louder in the affected ear, so the result lateralizes to the worse ear in otosclerosis.
- Absolute Bone Conduction (ABC): In stapedial otosclerosis, ABC is usually normal. However, in cochlear otosclerosis, bone conduction levels are reduced due to inner ear involvement.
- Gelle’s Test: This test evaluates stapes mobility. In cases where the stapes footplate is fixed, the test result is negative, indicating abnormal middle ear mechanics.
- Speech Audiometry: Speech discrimination scores typically remain normal, except in cochlear otosclerosis, where inner ear involvement can reduce clarity.
- Tympanometry: While tympanometry can help rule out other middle ear conditions like otitis media with effusion, it also checks the integrity of the stapedial reflex. A missing stapedial reflex suggests stapes fixation.
- High-Resolution CT Scan (HRCT) of the Temporal Bone: HRCT can detect abnormal bone remodeling within the inner ear. One classic finding is the “double ring sign,” which appears as blurred and narrowed margins of the oval window. As the disease progresses, the oval window niche may become completely blocked. This sign is often seen in cochlear otospongiosis.
- Pure Tone Audiometry (PTA): PTA usually reveals a conductive hearing loss, more pronounced at lower frequencies. The air–bone gap is typically greatest at 500 Hz, 1 kHz, and 2 kHz. A distinctive feature called the Carhart notch may appear—a dip in the bone conduction curve, especially around 2000 Hz. Though first identified in otosclerosis, it can occur in any condition that causes conductive hearing loss.
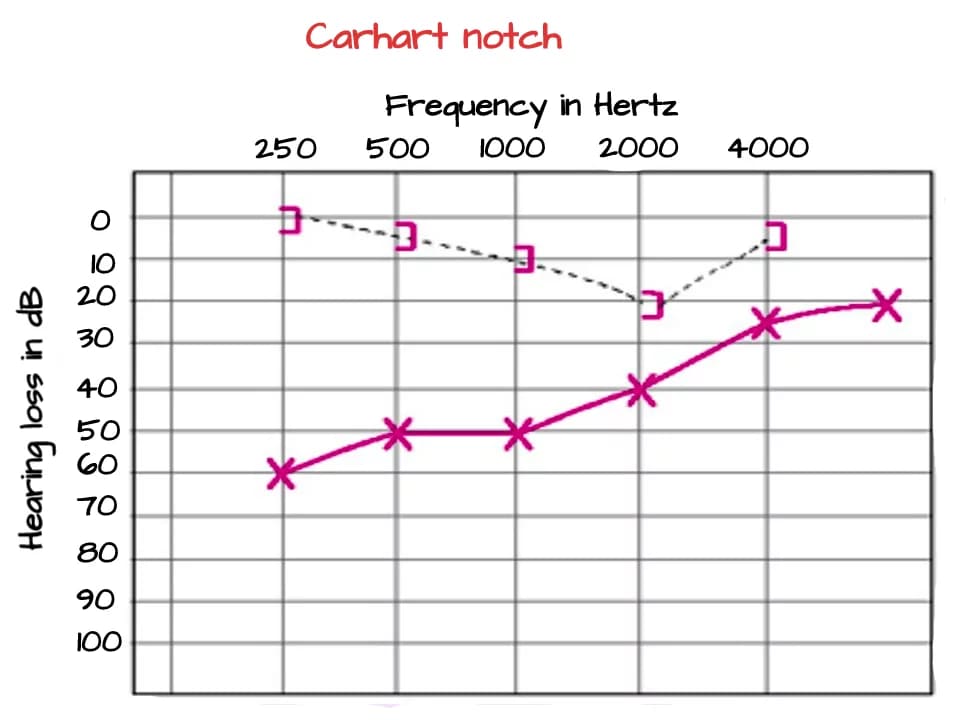
Carhart’s notch (otosclerosis)
Carhart Notch: Explanation
Bone-conducted sound reaches the cochlea through three pathways:
- Direct vibration of the skull
- Ossicular chain movement within the middle ear
- Vibrations entering the external ear canal, heard via air conduction
In otosclerosis, the second and third routes are compromised due to stapes fixation. This reduces bone conduction artificially by 5–15 dB, especially around 2 kHz, the resonant frequency of the ossicular chain. Fixation also limits perilymph movement, disturbing the inner ear’s response to sound. After successful surgery to free or replace the stapes, bone conduction levels often improve.
Occasionally, a “cookie bite” audiometric pattern may appear, especially in cases with mixed hearing loss. This pattern shows mid-frequency dips in both air and bone conduction curves, but it’s rare in otosclerosis.
Treatment
Treatment options for otosclerosis vary depending on the severity and type of hearing loss. These include medical therapy, hearing aids, and surgical intervention.
Medical Management
Medical therapy primarily targets the active (otospongiotic) phase of the disease to slow its progression, especially in cochlear otosclerosis.
- Sodium Fluoride Therapy: A daily combination of 40 mg sodium fluoride, 500 mg calcium gluconate, and 400 units of vitamin D for 12 to 24 months may stabilise bone metabolism and slow progressive hearing loss, particularly the sensorineural component.
- Third-Generation Bisphosphonates: These medications help reduce bone turnover and may slow down inner ear damage. They’re especially useful in patients with cochlear otosclerosis.
Hearing Aids
Hearing aids are a excellent, non-invasive option for many patients and are recommended in the following cases:
- Conservative Use: People who are not candidates for surgery, or who choose not to undergo it, may benefit from traditional air-conduction hearing aids.
- Far Advanced Otosclerosis (FAO): In cases where air conduction is worse than 85 dB and bone conduction is not measurable, conventional hearing aids may not be enough. Treatment options include:
- Stapedectomy with hearing aids
- Cochlear implants
- Direct Acoustic Cochlear Stimulation (DACS)
- Bone-Anchored Hearing Aids (BAHA): These are ideal for patients with otosclerosis in their only hearing ear or those with post-surgical cavities where traditional aids are ineffective. BAHA carry no risk of causing total hearing loss.
- DACS Device: DACS combines a middle ear implant with a prosthesis. It is suitable for patients with mixed hearing loss where surgery alone doesn’t provide enough benefit.
- Cochlear Implants: Used in cases of Far Advanced Otosclerosis or after a failed stapedotomy.
Pitfalls of cochlear implantation in otosclerosis are as a result of previous otosclerosis surgery, which are:
- Incus subluxation
- Middle ear adhesions
- Tympanic membrane vulnerable at site of bony curettage
- Ossification of Scala tympani from post-stapedectomy labyrinthitis
- As a result of the disease process
- Obliteration of round window by spongiotic bone
- Incomplete electrode placement
- ‘Looping’ of the electrode through soft spongiotic bone in the cochlea
- Facial nerve stimulation by the placement of electrodes in the cochlea
Surgical Management – Stapes Surgery
Stapes surgery is the most effective treatment for conductive hearing loss in otosclerosis. The goal is to restore the mobility of the oval window mechanism.
Types of Stapes Surgery are:
- Stapedectomy: The entire stapes bone is removed and replaced with a prosthesis (usually made of Teflon, titanium, or a combination of materials).
- Laser Stapedotomy (Preferred Technique): A tiny hole is created in the footplate of the stapes using a laser, and a prosthesis is inserted through it.
- Vein Graft Teflon Interposition Surgery
- Stapedotomy with Tendon Preservation: This technique preserves the stapedius tendon, which may reduce complications.
Selection of patient for stapes surgery:
- Patients with social hearing handicap (air conduction threshold ≥ 30 dB)
- Air-bone gap of at least 15 dB
- Rinne negative test results at 256 and 512 Hz
- Speech discrimination score ≥ 60%
Steps of Stapedectomy: The surgery is preferably done under local anaesthesia
- Flap Elevation: An incision is made in the ear canal, and the tympanomeatal flap is elevated.
- Exposure and Disconnection: The surgeon exposes the stapes, separates it from the incus, and cuts the stapedius tendon.
- Stapes Removal: The superstructure of the stapes is fractured and removed carefully, away from the facial nerve. However, it is better to first divide the posterior crus with laser/ crurotomy scissors to reduce the risk of mobilizing the footplate.
- Measurement: The distance between the incus and footplate is measured. The prosthesis selected to be 0.25 mm longer than the distance from the underside of the incus to the footplate.
- Fenestration: A small hole (fenestration) is made in the posterior third of the footplate (stapedotomy) or the removal of a part of the footplate (stapedectomy) using a laser or drill.
- Prosthesis Placement: A prosthesis, slightly longer than the measured distance, is inserted and secured.
- Flap Repositioning: The tympanomeatal flap is repositioned, and the surgery is complete.
Diagram: Steps of a Stapedotomy in a Right Ear

- Image 1: Elevation of Tympanomeatal Flap and Curetting of Scutum
The procedure begins with the elevation of the tympanomeatal flap. This is followed by curetting the scutum to ensure adequate exposure. The exposure is considered sufficient when the facial nerve, pyramidal process, and round window are clearly visualized. - Image 2: Measurement and Preparation
Next, the surgeon takes precise measurements from the medial aspect of the incus to the footplate. This is followed by the separation of the incudo-stapedial joint and the sectioning of the stapedial tendon. - Image 3 and 4: Drilling and Down-Fracturing
The surgeon then drills the posterior crura of the stapes, making the footplate visible. Following this, the remaining stapes superstructure is carefully down-fractured. During this step, it is crucial for the surgeon to monitor the footplate closely to prevent dislocation. - Image 5: Fenestration of the Footplate
Once the superstructure is removed, a fenestration (small opening) is created in the footplate. - Image 6: Insertion and Crimping of the Piston
Finally, a piston is inserted into the fenestration. The procedure concludes with crimping the piston to the incus, ensuring proper placement and function.
Complications of stapes surgery:
- Conductive Hearing Loss: This can result from prosthesis displacement, incus erosion, or new bone growth.
- Sensorineural Hearing Loss (SNHL): This may occur due to surgical trauma, barotrauma, or inflammation (labyrinthitis).
- Perilymph gusher: Abnormal communication with the cochlea or dehiscent cochlear aqueduct.
- Facial Nerve Injury: Caused by overheating from the drill or incorrect local anaesthesia.
- Vertigo: Often temporary and resolves within a week.
- Incus Dislocation: This can happen during surgery or later due to pressure changes or infections.
- Taste Disturbances and Dry Mouth: Due to injury to the chorda tympani nerve.
- Dead Ear: In rare cases, permanent total hearing loss may occur, often due to reparative granuloma after surgery.
Contraindications of stapes surgery:
- Otosclerosis in the only hearing ear.
- Age > 70 years.
- Young children- Recurrent eustachian tube dysfunction may displace the prosthesis or cause acute otitis media.
- Sportspersons, snorkelling, parachuting, construction workers at high altitudes, scuba divers and frequent air travellers have a risk of postoperative vertigo.
- Patients having occupational noise exposure are susceptible to sensorineural hearing loss after surgery.
- Pregnancy
Relative contraindications:
- Diabetes, active otosclerosis and eustachian tube dysfunction.
- Active infection in outer or middle ear, tympanic membrane perforation and exostosis.
———— End of the chapter ————
High-Yield Points & Quick Revision (NEET PG & VIVA)
- Pathognomonic Site: Fissula ante fenestram is the most common site of involvement.
- Histology: Otosclerosis affects the enchondral layer of the otic capsule.
- True Incidence: Determined by Histologic Otosclerosis (up to 10% in Caucasians).
- Classic Symptom: Paracusis Willisii (hearing better in noise).
- Classic Sign: Schwartze Sign (Flamingo Flush, indicates active focus).
- Key Audiometry Feature: Carhart Notch (artifactual 2000 Hz dip in BC).
- Key Tympanometry Feature: Absent stapedial reflex (most sensitive sign).
- Key Imaging Feature: Double Ring Sign on HRCT (cochlear otospongiosis).
- Treatment of Choice: Laser Stapedotomy for conductive hearing loss.
- Most Feared Complication: Dead Ear due to SNHL or Reparative Granuloma.
- CBME Competency: A PG student must be able to diagnose a case of CHL and confidently rule out chronic suppurative otitis media (CSOM) based on a normal tympanic membrane (in most cases) before advising surgery.
Frequently Asked Questions (FAQ Schema Optimised)
- What is the difference between otosclerosis and otospongiosis? Otosclerosis is the overall disease process; otospongiosis refers specifically to the active, highly vascular phase of bone resorption, which precedes the final, dense, sclerotic (otosclerosis) phase.
- Is otosclerosis hereditary? Yes, otosclerosis is hereditary in about 50% of cases, often following an autosomal dominant pattern with reduced penetrance.
- What is Carhart’s notch, and why does it occur? Carhart’s notch is an artifactual reduction in bone conduction at $2000$ Hz, which occurs because the fixed stapes disrupts the normal vibrational pathways of the ossicular chain and skull, not because of true cochlear damage.
- What is the best treatment for otosclerosis? The best treatment for conductive hearing loss is a surgical procedure called Laser Stapedotomy, while hearing aids are a non-invasive alternative.
- Can pregnancy worsen hearing loss in otosclerosis? Yes, hormonal changes during pregnancy are a known factor that may accelerate the progression and worsening of hearing loss in susceptible women with otosclerosis.
NEET PG/University Exam MCQs
- 1. A 28-year-old female presents with slowly progressive, bilateral hearing loss. She reports that she hears better in a noisy restaurant. Otoscopy is normal, and Rinne test is negative at $512$ Hz bilaterally. The most likely diagnosis is: A. Chronic Suppurative Otitis Media (CSOM) B. Meniere’s Disease C. Otosclerosis D. Superior Semicircular Canal Dehiscence
- 2. The pathological hallmark of otosclerosis is the involvement of which layer of the bony otic capsule? A. Periosteal layer B. Mucosal layer C. Enchondral layer D. Endosteal layer
- 3. Which clinical sign, if present, suggests an active otospongiotic focus and increased vascularity? A. Brown sign B. Schwartze sign C. House-Brackmann sign D. Fistula sign
- 4. The characteristic dip in the bone conduction curve at $2000$ Hz seen in otosclerosis is known as: A. Rosette phenomenon B. Carhart notch C. Gellé sign D. Paracusis Willisii
- 5. All of the following are typically observed in stapedial otosclerosis EXCEPT: A. Absent Stapedial Reflex on Tympanometry B. Paracusis Willisii C. Reduced Speech Discrimination Score (SDS) D. Negative Rinne Test
- 6. The most common site of an otosclerotic focus is the: A. Fissula post fenestram B. Round window niche C. Fissula ante fenestram D. Area around the semicircular canals
- 7. Which of the following is considered an absolute contraindication for stapes surgery? A. Age over 60 years B. Positive Schwartze sign C. Otosclerosis in the only hearing ear D. Family history of otosclerosis
- 8. The incidence of otosclerosis is highest in which population group? A. Chinese and Japanese B. African Americans C. Caucasians and individuals of Indian descent D. Native Americans
- 9. The primary mechanism leading to conductive hearing loss in stapedial otosclerosis is: A. Tympanic membrane perforation B. Ossicular chain erosion C. Stapes footplate fixation D. Obliteration of the Eustachian tube
- 10. A rare, late post-stapedotomy complication presenting with progressive sensorineural hearing loss and resulting in a dead ear is: A. Incus dislocation B. Facial nerve paralysis C. Reparative granuloma D. Temporary vertigo
MCQ Answers and Explanations
- C. Otosclerosis. The triad of progressive, bilateral hearing loss with a normal drum, negative Rinne test (CHL), and Paracusis Willisii (hearing better in noise) is classic for otosclerosis.
- C. Enchondral layer. Otosclerosis is a bone disorder of the otic capsule, specifically replacing the normal dense bone in the enchondral layer with spongy bone.
- B. Schwartze sign. The reddish hue (flamingo flush) on the promontory is the visible sign of an active, highly vascular otospongiotic focus.
- B. Carhart notch. This is the pathognomonic audiometric finding, representing an artifactual drop in bone conduction around the resonant frequency of the ossicular chain ($2000$ Hz).
- C. Reduced Speech Discrimination Score (SDS). Pure conductive hearing loss does not typically affect the cochlea, so speech understanding (SDS) remains normal. SDS is reduced in SNHL or profound mixed loss.
- C. Fissula ante fenestram. This is the site of predilection and the most common initial focus for stapedial otosclerosis.
- C. Otosclerosis in the only hearing ear. The risk of a “dead ear” complication is unacceptable in the patient’s only hearing ear.
- C. Caucasians and individuals of Indian descent. Statistical data shows a significantly higher prevalence in these groups compared to Asian (Chinese/Japanese) and African populations.
- C. Stapes footplate fixation. The ankylosis of the stapes footplate at the oval window is the direct cause of the conductive hearing loss.
- C. Reparative granuloma. This is a rare, but severe, late complication that requires immediate surgical re-exploration and steroid treatment to try and preserve any remaining hearing.
Clinical Scenarios & VIVA Questions
Clinical Scenario 1: Unilateral Hearing Loss. A 35-year-old male presents with unilateral, gradually progressive hearing loss for five years. He also reports occasional tinnitus in the same ear. His wife mentions he often misses her whispers. Otoscopy is completely normal. Pure Tone Audiometry reveals a moderate conductive hearing loss in the affected ear with an Air-Bone Gap of 25% dB.
-
“What is your immediate differential diagnosis, given the normal otoscopy and CHL?” Answer: My primary differentials are Otosclerosis, Ossicular Chain Disruption (e.g., post-traumatic), Congenital Stapes Fixation, and less commonly, malleus head fixation or tympanosclerosis.
-
“How would you use tuning fork tests to confirm your suspicion of otosclerosis?” Answer: I would perform a Rinne test, expecting it to be negative (BC > AC). I would also perform a Weber test, expecting it to lateralize to the affected ear (the one with the CHL). I would also do the Gellé test, expecting it to be negative (no change in hearing with applied pressure).
-
“What is the next definitive investigation, and what are you specifically looking for in the report?” Answer: The next definitive non-invasive investigation is Tympanometry/Acoustic Reflexometry. I would be looking for a Type A curve with an absent Stapedial Reflex, which is highly suggestive of stapes fixation.
Clinical Scenario 2: Post-Surgical Complication. A 40-year-old female successfully underwent a right laser stapedotomy for otosclerosis six months ago, with her hearing returning to near-normal. She now presents with a sudden onset of profound dizziness (vertigo), accompanied by total hearing loss (dead ear) in the operated ear, after a severe episode of flu a few days ago.
-
“What is the most likely cause for this dramatic presentation?” Answer: The most critical diagnosis to rule out is Perilymphatic Fistula (PLF), possibly precipitated by the severe coughing from the flu, causing inner ear fluid leak and sudden sensorineural hearing loss (SNHL) and vertigo. Another possibility is a delayed post-operative Labyrinthitis.
-
“Describe the management principle for this complication.” Answer: This is an otological emergency. Management involves immediate bed rest with the head of the bed elevated, and potentially high-dose steroids to manage inflammation. If a PLF is strongly suspected, or if symptoms do not resolve rapidly, the patient needs urgent surgical exploration of the middle ear and oval window to repair the fistula.
-
“What advice would you give this patient regarding flying or sports moving forward?” Answer: I would strongly advise against activities that involve significant or rapid pressure changes, such as scuba diving, parachuting, or high-altitude flying, as these activities carry a high risk of pressure-related injury to the oval window and recurrence of perilymphatic fistula.
———— End ————
Download the full PDF Link:
Otosclerosis Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Anirban Biswas, Textbook of Clinical Audio-vestibulometry.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Gordon B. Hughes, Myles L. Pensak, H. B. Broidy. Textbook of Clinical Otology.
- Mario Sanna. Textbook of Color Atlas of Endo-Otoscopy Examination–Diagnosis–Treatment.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Master Otosclerosis for MBBS & ENT PG exams. This ultimate CBME-aligned guide covers aetiology, Carhart Notch, Stapedotomy steps, and high-yield MCQs. Download quick revision notes now, Carhart’s notch, Flamingo, Schwatrz sign, fissula ante fenestram, Stapedectomy, Far Advanced Otosclerosis, Oral flourides, Otosclerosis, Otosclerosis notes, Otosclerosis symptoms, Otosclerosis treatment, Otosclerosis MCQs, Carhart’s notch explained, Stapedotomy procedure, Otosclerosis etiology, Otosclerosis pathology, Otosclerosis viva questions, Otosclerosis summary, Otosclerosis ppt, Otosclerosis prognosis, Otosclerosis surgery, What is otosclerosis and its treatment, How to perform stapedotomy steps, Otosclerosis causes and symptoms in adults, Differential diagnosis of conductive hearing loss with normal TM, Otosclerosis CBME exam guide, NEET PG high-yield ENT otosclerosis topics, Carhart’s notch, Flamingo, schwartz sign in otosclerosis, otosclerosis ppt, pathophysiology, radiology, cochlear otosclerosis, stapedial otosclerosis, Otosclerosis natural treatment options, Early signs of otosclerosis, Otosclerosis and tinnitus management, Otosclerosis hearing aids effectiveness, Stapedectomy success rates in otosclerosis patients, Exploring Natural Treatment Options for Otosclerosis, Recognizing the Early Signs of Otosclerosis: A Comprehensive Guide, Managing Tinnitus in Otosclerosis Patients: Effective Strategies, Evaluating the Effectiveness of Hearing Aids for Otosclerosis, Understanding Stapedectomy Success Rates in Otosclerosis Treatment

It’s good for conceptual clarity