Tympanoplasty
Tympanoplasty is a surgical procedure aimed at (i) eradicating disease from the middle ear and (ii) reconstructing the hearing mechanism. This operation may be performed with or without mastoid surgery and may or may not involve tympanic membrane grafting.
Defining the Terminology: Myringoplasty vs. Ossiculoplasty vs. Tympanoplasty
Students often confuse these terms; however, the distinctions are clear and frequently tested.
- Myringoplasty: This refers specifically when the procedure is limited to the repair of the tympanic membrane perforation. It focuses solely on closing the defect, without addressing the ossicles.
- Ossiculoplasty: Conversely, when the focus is solely on the reconstruction of the ossicular chain (malleus, incus, stapes) to restore sound conduction, it is termed ossiculoplasty.
- Tympanoplasty: This is a comprehensive term. When myringoplasty and ossiculoplasty are performed together in the same operation, it is correctly termed tympanoplasty. Furthermore, tympanoplasty can be combined with either an intact canal wall (ICW) or a canal-wall-down (CWD) mastoidectomy to effectively eradicate disease from the mastoid air cells.
Effects of Tympanic Membrane Perforation on Hearing
Tympanic membrane perforation significantly impacts auditory function through several mechanisms:
- Loss of Transformer Mechanism: The intact TM provides an area ratio advantage (TM area vs. stapes footplate area ~ 55:1). A perforation dissipates sound pressure, reducing this ratio. The presence of a perforation disrupts the transformer mechanism of the ear. The larger the size of the perforation, the greater the transformer ratio. Total perforation can result in a hearing loss of approximately 40 to 45 dB.
- Loss of Sound Phase Protection (Round Window Baffle Effect): Normally, the intact TM protects the round window, directing sound waves preferentially to the oval window. A perforation removes the protective barrier of the tympanic membrane over the round window, allowing sound to reach both the oval and round windows simultaneously. This can lead to the cancellation of resultant movements of the perilymph.
- Effect of Interrupted Ossicular Chain: An interrupted ossicular chain has a minimal effect on hearing in cases of large perforations. However, an interrupted ossicular chain behind an intact tympanic membrane can lead to a maximum conductive hearing loss of 60 dB. This is due to the inability of vibrations from the ossicular chain to reach the oval window, as well as the protection provided to both the oval and round windows by the intact tympanic membrane.
Aim of Tympanoplasty
The primary objectives of tympanoplasty are to restore and achieve the following:
- To create a dry, safe ear by eradicating disease.
- To restore the transformer mechanism by grafting the TM and connecting it to the oval window via an intact/reconstructed ossicle chain.
- To re-establish the round window baffle effect by creating a closed, air-containing middle ear space.
Indications of Tympanoplasty.
- Chronic TM perforation (dry or inactive)
- Conductive hearing loss due to TM perforation with or without ossicular pathology
- Tympanosclerosis (selected cases)
- As part of surgery for cholesteatoma or chronic otitis media

Contraindications of Tympanoplasty.
The following conditions contraindicate tympanoplasty:
- Acute suppurative otitis media (ASOM)
- Malignant tumors of the outer or middle ear
- Uncontrolled cholesteatoma
- Uncontrolled systemic disease (e.g., diabetes)
- Only hearing ear
- Eustachian tube dysfunction
- Actively discharging ear
- Otitis externa
- Complicated chronic suppurative otitis media (CSOM)
- Unusual infections, such as malignant otitis externa
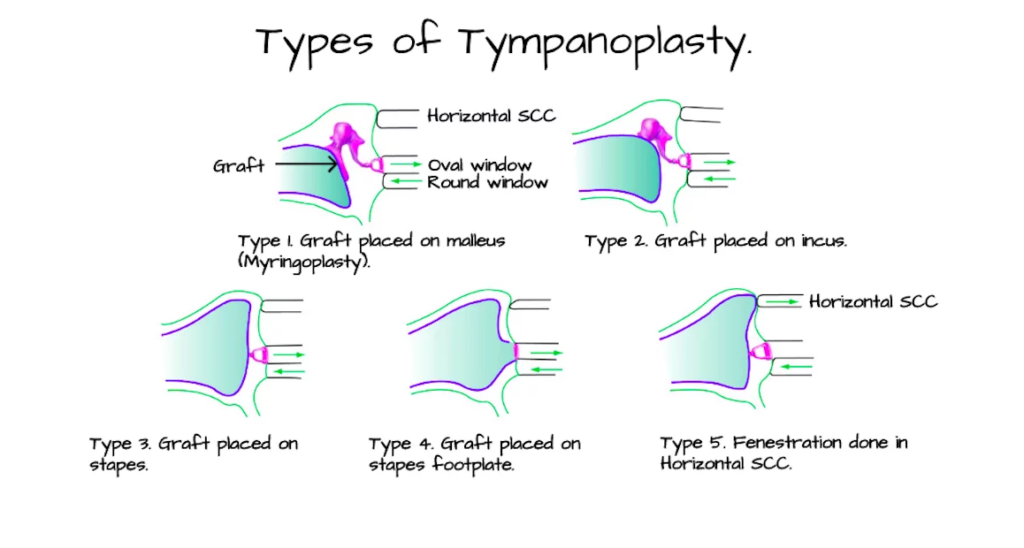
Types of Tympanoplasty.
Wullstein classified tympanoplasty into five types.
|
Type I: |
There is only a perforation of the tympanic membrane and it is repaired. This is similar to myringoplasty except that the ossicular chain is intact on middle ear inspection. |
|
Type II: |
There is a perforation of the tympanic membrane along with erosion of the malleus. The graft is placed over the remnant of malleus or incus. |
|
Type III: |
Here both malleus and incus have been eroded or removed to clear the disease. The graft is placed over the head of the stapes. It is also called myringostapediopexy or columella tympanoplasty. |
|
Type IV: |
Malleus, incus and suprastructure of stapes are completely eroded or have been removed to clear the disease and only footplate of stapes is present. The stapes footplate is left exposed and the graft is placed over the round window area in continuation with Eustachian tube to create a small cavity called the cavum minor (Round window baffle effect). This leads to the sound waves directly striking the oval window. |
|
Type V: |
The stapes footplate is fixed. A second window is created by drilling the dome of horizontal semicircular canal bone and the procedure is called fenestration operation. Graft is also placed over this newly created second window. This is an obsolete procedure and no longer done nowadays. |
Anaesthesia. General anaesthesia is preferred for all chronic ear surgery procedures.
Tympanoplasty Approaches.
Tympanoplasty is a surgical procedure aimed at repairing the tympanic membrane (eardrum) and the middle ear structures. Various approaches are utilised depending on the specific clinical scenario, including the size and location of the perforation, the condition of the ear canal, and the presence of any associated pathology. The following sections outline the primary tympanoplasty approaches, their indications, procedural steps, and associated considerations.
1. Postaural (Wilde’s) Incision. The postaural incision is the preferred approach for large perforations, particularly those located anteriorly or in cases where the ear canal is small. The incision begins at the highest attachment of the pinna, follows the curve of the retroauricular groove approximately 1 cm posterior to it, and terminates at the mastoid tip. In infants and children under two years of age, the incision is adjusted to avoid the lower part of the mastoid due to the proximity of the facial nerve.
Indications: The postaural approach is utilised for:
- Cortical mastoidectomy
- Modified radical and radical mastoidectomy
- Tympanoplasty, especially when the perforation extends anterior to the handle of the malleus
- Exposure of cranial nerve VII in the vertical segment
- Surgery of the endolymphatic sac
Procedural Steps:
- EUM: Examination under the microscope is done to confirm the clinical findings.

- For local anaesthesia, 2% xylocaine with adrenaline is injected in the postaural region (from the root of the helix to the mastoid tip) and the external auditory canal.

- Wilde’s incision: A postaural incision is given from the root of the helix to the mastoid tip.


- Temporalis fascia graft is harvested.

- The margins of the perforation are freshened.

- A tympanomeatal flap, consisting of the posterior meatal canal skin, is elevated, which is made in continuity with the tympanic membrane after dislocating the annulus from the sulcus.

- The incision is given in the middle ear mucosa below the annulus and the tympanomeatal flap is elevated.

- The handle of the malleus is denuded.

- The middle ear and ossicular chain are inspected and repaired as necessary.
- Any posterosuperior overhang of the bony meatus, if present, is removed to enhance the visibility of the ossicles.
- The middle ear is packed with gelfoam.

- The graft is placed medial to the tympanic membrane remnant or tympanic annulus and lateral to the manubrium of the malleus.
- The tympanomeatal flap is returned to its original position, and the medial aspect of the ear canal is packed with gelfoam impregnated with antibiotic ointment.
2. Endomeatal or Transcanal Approach. The endomeatal or transcanal approach is indicated for small posterior perforations and is particularly suitable when the ear canal is sufficiently large. This approach offers the advantage of avoiding a postauricular incision scar and the need for mastoid dressing during the postoperative period. Common indications for this approach include:
- Exploratory tympanotomy to identify the cause of conductive hearing loss
- Inlay myringoplasty
- Ossicular reconstruction
Procedural Steps:
- The margins of the perforation are denuded.
- A tympanomeatal flap, consisting of the posterior meatal canal skin, is elevated using Rosen’s incision, which is made in continuity with the tympanic membrane after dislocating the annulus from the sulcus.
- The middle ear and ossicular chain are inspected and repaired as necessary.
- Any posterosuperior overhang of the bony meatus, if present, is removed to enhance visibility of the stapes.
- The middle ear is packed with gelfoam.
- The graft is placed medial to the tympanic membrane remnant or tympanic annulus, and the manubrium of the malleus.
- The tympanomeatal flap is returned to its original position, and the medial aspect of the ear canal is packed with gelfoam impregnated with antibiotic ointment.

Rosen’s Incision: Rosen’s incision consists of two components:
- A small vertical incision at the 12 o’clock position near the annulus.
- A curvilinear incision that begins at the 6 o’clock position and meets the first incision in the posterosuperior region of the canal, approximately 5–7 mm away from the annulus.
3. Endaural Approach. The endaural approach is less commonly employed today due to concerns regarding scar visibility and limited posterior exposure. However, it is indicated for specific conditions, including:
- Excision of osteomas or exostoses of the ear canal
- Large tympanic membrane perforations
- Attic cholesteatomas with limited extension into the antrum
- Modified radical mastoidectomy when the disease is confined to the attic, antrum, and part of the mastoid
Procedural Steps: The endaural approach is characterised by two incisions:
- Lempert 1st Incision: A semi-circumferential incision made along the posterior half of the ear canal at the bony-cartilaginous junction, extending from the 12 o’clock to the 6 o’clock position.
- Lempert 2nd Incision: This incision begins at the 12 o’clock position of the first incision and ascends vertically in a curvilinear manner between the tragus and the root of the helix, passing through the incisura terminalis to avoid cutting the cartilage.

Complications of Tympanoplasty.
Potential complications associated with tympanoplasty include:
- Intraoperative bleeding, particularly from an uncovered jugular bulb
- Facial nerve palsy
- Wound infection or perichondritis
- Wound hematoma
- Injury to the chorda tympani nerve
- Graft failure
- Sensorineural hearing loss or dizziness
Grafting Materials
The most commonly used graft materials in myringoplasty include the temporalis fascia or perichondrium (tragal or conchal) harvested from the patient.
- Temporalis fascia is the most commonly used graft for all perforations, given its availability, the abundance of tissue and ease of use.
- Tragal perichondrium is preferred for the permeatal approach. Cartilage from the tragus or concha is becoming increasingly popular as a reliable material for repairing tympanic membrane perforations. One effective technique for smaller perforations, those less than 6mm, involves creating a cartilage “butterfly.” In this method, a cartilage disc is circumferentially incised by 1mm. This groove is then fitted into the perforation rim, stabilising the graft and ensuring a secure fit.
- Homografts (Historical). Occasionally, homografts such as dura mater, vein, fascia, or cadaver tympanic membrane may be utilised.
Graft Placement Techniques
There are two primary grafting techniques in tympanoplasty: underlay and overlay. Both techniques can yield excellent outcomes when performed by experienced surgeons.
- Underlay Technique: The graft is positioned medial to the inner mucosal layer of the tympanic membrane remnant and hence over the fibrous annulus, stabilised by gelfoam in the middle ear. The underlay technique is considered superior for several reasons. It offers technical ease during the procedure, results in a shorter post-operative healing time, has fewer complications, and provides better hearing gain for patients. This technique is relatively straightforward but may lead to graft medialization and reduced middle ear space. It is essential to avoid nitrous oxide gas during graft placement, as it can diffuse into the middle ear and displace the graft.
- Overlay Technique: The graft is placed lateral to the middle fibrous layer of the tympanic membrane remnant and hence over the fibrous annulus. This technique requires careful removal of the outer epithelial layer of the tympanic membrane remnant. Although the overlay technique can provide good results, it is associated with a higher incidence of complications, including the formation of epithelial pearls, anterior sulcus blunting, granulation tissue formation, and graft lateralisation. It is considered a more technically demanding procedure.
——– End of the chapter ——–
High-Yield Points for Quick Revision (NEET PG & University Exams)
- Myringoplasty = Type I Tympanoplasty.
- Total TM perforation causes ~40-45 dB CHL. Ossicular discontinuity behind intact TM causes up to ~60 dB CHL.
- Most common graft material: Temporalis fascia.
- Most common grafting technique: Underlay.
- Wullstein Type III is Myringostapediopexy (graft on stapes head).
- Wullstein Type IV creates a cavum minor with a mobile stapes footplate.
- Key contraindication: Actively discharging ear (must be dry for >3 months ideally).
- Major complication of the overlay technique: Epithelial pearl.
- Eustachian tube function is the most critical prognostic factor for success.
- Cartilage grafts are increasingly used for their stability, especially in revision surgery.
Frequently Asked Questions (FAQs) in Viva
- Q: What is the difference between myringoplasty and tympanoplasty? A: Myringoplasty is the repair of the tympanic membrane only, which is classified as a Type I tympanoplasty. Tympanoplasty is a broader term that can include both eardrum repair (myringoplasty) and ossicular chain reconstruction (ossiculoplasty).
- Q: What is the most important factor for successful tympanoplasty? A: Adequate Eustachian tube function is the single most important prognostic factor. A non-functioning tube leads to graft failure, atelectasis, or recurrent effusion.
- Q: Which graft material is best for tympanoplasty? A: There’s no single “best” material. Temporalis fascia is the most commonly used due to its ease of harvest and reliability. However, tragal cartilage-perichondrium is superior for preventing re-perforation in high-risk cases (e.g., large perforations, revision surgery).
- Q: How long should an ear be dry before tympanoplasty? A: Ideally, the ear should be dry and infection-free for a minimum of 3 to 6 months prior to surgery, as this indicates a period of stability and better tubal function.
- Q: What is a common late complication of the overlay grafting technique? A: The formation of an “epithelial pearl” or iatrogenic cholesteatoma is a classic late complication of the overlay technique, caused by trapped squamous epithelium under the graft.
- Q: What is Wullstein Type IV tympanoplasty? A: In Type IV, only a mobile stapes footplate remains. The graft seals the middle ear, creating a small air space (cavum minor) over the footplate, while the round window is shielded to maintain phase difference.
- Q: Can tympanoplasty be done under local anesthesia? A: Yes, for cooperative adults and simple myringoplasty, local anesthesia (with sedation) is a viable option. However, for lengthy procedures or anxious patients, general anesthesia is preferred.
MCQs (NEET PG Style)
- A 30-year-old male with a large central tympanic membrane perforation has a hearing loss of 42 dB. Ossicular chain is intact. What is the main mechanism of his hearing loss? A. Disrupted ossicular chain lever mechanism B. Loss of round window protection C. Reduced hydraulic ratio of tympanic membrane D. Cochlear hair cell damage
- Which of the following is a Type III tympanoplasty according to Wullstein’s classification? A. Myringoplasty B. Graft placed on incus C. Myringostapediopexy D. Cavum minor formation
- The most critical prognostic factor for the success of tympanoplasty is: A. Size of the perforation B. Skill of the surgeon C. Eustachian tube function D. Type of graft used
- A patient develops a pearly white cyst behind the tympanic membrane 2 years after an overlay myringoplasty. What is the most likely diagnosis? A. Tympanosclerosis B. Otitis media with effusion C. Epithelial pearl D. Graft lateralization
- Which surgical approach is MOST suitable for a large anterior tympanic membrane perforation in a patient with a narrow ear canal? A. Transcanal B. Endaural C. Postaural D. All are equally suitable
- What is the expected maximum conductive hearing loss in a patient with an intact tympanic membrane but complete ossicular discontinuity? A. 20-30 dB B. 40-45 dB C. 60 dB D. 80 dB
- Which material is most commonly used as a graft in myringoplasty? A. Vein graft B. Temporalis fascia C. Fat plug D. Skin graft
- All of the following are absolute contraindications for tympanoplasty, EXCEPT: A. Active mucopurulent otorrhea B. Only hearing ear C. Tympanosclerosis D. Malignancy of the middle ear
- In Wullstein classification, creation of a “cavum minor” is characteristic of which type? A. Type II B. Type III C. Type IV D. Type V
- The underlay technique of grafting is associated with all of the following, EXCEPT: A. Shorter healing time B. Lower risk of epithelial pearls C. Risk of graft medialization D. Requires extensive epithelial peeling
Answers & Explanations:
- C. Large perforation reduces the effective area ratio (hydraulic mechanism), causing ~40-45 dB loss. The ossicular chain is intact (A is wrong). B contributes but is not the primary mechanism for this degree of loss.
- C. Type III is direct placement of the graft onto the stapes head (myringostapediopexy). A is Type I. B is Type II. D is Type IV.
- C. Eustachian tube function is paramount for maintaining aeration and health of the middle ear post-operatively.
- C. Epithelial pearl is a classic delayed complication of the overlay technique due to entrapped squamous epithelium.
- C. Postaural approach provides the best exposure for large anterior perforations and narrow canals.
- C. Ossicular discontinuity behind an intact TM causes maximal CHL of ~60 dB due to loss of both transformer mechanism and phase protection.
- B. Temporalis fascia is the most common autograft due to accessibility and reliability.
- C. Tympanosclerosis is an indication for surgery if it causes fixation or hearing loss. A, B, and D are strong contraindications.
- C. In Type IV, the graft creates a small middle ear space (cavum minor) over the mobile stapes footplate.
- D. Extensive epithelial peeling is a hallmark of the overlay technique, not the underlay.
Clinical Case Scenarios for Viva Voce
Case 1: A 25-year-old female presents with a 5-year history of right ear discharge and hearing loss. The ear has been dry for 4 months. Otoscopy shows a large, subtotal central perforation. Audiometry reveals a 45 dB conductive hearing loss. Tuning fork tests show Rinne negative and Weber lateralized to the right ear.
- What is your diagnosis? Inactive Chronic Suppurative Otitis Media (CSOM) with a large TM perforation and conductive hearing loss.
- What surgery will you advise? Tympanoplasty (Type I myringoplasty) to close the perforation and improve hearing.
- Which approach and graft would you choose? Given the large size, a postaural approach with an underlay temporalis fascia graft is a standard choice. Consider cartilage if the middle ear mucosa is poor.
Case 2: A 40-year-old male, post-canal wall down mastoidectomy for cholesteatoma 10 years ago, now has a completely intact TM but a 55 dB conductive hearing loss. CT scan shows an absent incus.
- What is the cause of his hearing loss? Ossicular discontinuity (missing incus) behind an intact TM.
- What procedure is needed? Ossiculoplasty. The TM does not need repair.
- What are his ossiculoplasty options? Use of an autograft (remodeled incus/malleus) or a synthetic prosthesis (e.g., PORP – Partial Ossicular Replacement Prosthesis) to connect the malleus/neotympanum to the stapes head.
Case 3: During a postaural tympanoplasty, you find that the malleus and incus are absent, but the stapes superstructure is intact and mobile.
- According to Wullstein, what type of tympanoplasty will you perform? Type III Tympanoplasty (Myringostapediopexy).
- How will you reconstruct? Place the graft (fascia/cartilage) directly onto the head of the stapes.
——– End ——–
Download the full PDF Link:
Tympanoplasty Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck Surgery
- Hans Behrbohm, Textbook of Ear, Nose, and Throat Diseases With Head and Neck Surgery.
- Salah Mansour, Middle Ear Diseases – Advances in Diagnosis and Management.
- Logan Turner, Textbook of Diseases of The Nose, Throat and Ear Head And Neck Surgery.
- Rob and smith, Textbook of Operative surgery.
- Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Aim of Tympanoplasty, Endomeatal or Transcanal Approach, Postaural (Wilde’s) Incision,Endaural Approach, Underlay Technique, Overlay Technique, Tympanoplasty, Myringoplasty, Ossiculoplasty, Wullstein classification, Type I tympanoplasty, Type III tympanoplasty, Myringostapediopexy, Underlay vs overlay graft, Temporalis fascia graft, Tragal cartilage graft, Tympanoplasty complications, Epithelial pearl, Tympanoplasty indications, Tympanoplasty contraindications, Tympanoplasty steps, Postaural approach, Permeatal approach, ENT surgery notes, CBME ENT, NEET PG ENT high yield, ENT exam MCQs, ENT viva questions, Conductive hearing loss surgery, How to repair eardrum, Tympanic membrane perforation surgery, Eustachian tube function tympanoplasty, ENT practical exam cases, MBBS ENT notes, ENT PG entrance exam.

Sir pdf of this and various other lectures ais not available
Dear Dr Shailendra,
Thank you sincerely for taking the time to read my book. It’s truly an honor to know that a colleague in the medical profession has engaged with my work. It’s encouraging to know the content may have contributed to your clinical or academic interests. You can find the tympanoplasty pdf now. If you have any feedback—whether it’s about the clarity, relevance, or usefulness of the material—I would be deeply grateful to hear your thoughts.
With warm regards,
Dr Rahul Bagla
Just scrubbed my first tympanoplasty (RN) this was a great read to better understand the procedure! Much appreciated. 🙂
I just had a myringoplasty performed on myself. Your document helped me picture what the surgeon did.
Thank you for your help to all ORL-HNS
Thank you for your kind help for ORL-HNS
Thanks