|
The following CBME core competencies are covered in this chapter.
|
Facial Nerve Paralysis
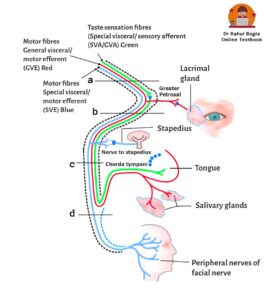
The facial nerve, the seventh cranial nerve, is an embryological derivative of the second branchial arch. It is a mixed nerve, containing both motor and sensory fibres. The large motor fibres control the muscles of facial expression, while a small sensory nerve (the nerve of Wrisberg, also known as Nervus Intermedius) carries secretomotor fibres to the lacrimal and salivary glands, as well as taste and general sensation fibres. The facial nerve has two motor fibre branches and two sensory fibre branches. The motor fibres originate from the facial nerve nucleus and superior salivatory nucleus in the central nervous system (CNS), while the sensory fibres branches are related to the nucleus of the tractus solitarius and the spinal nucleus of the trigeminal complex in the CNS.
NUCLEUS RELATED TO VIIth NERVE
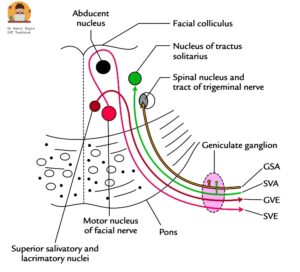
Diagram: Cross section through the pons, showing nuclei’s related to facial nerve
- Facial nerve nucleus (principle nucleus or branchiomotor nucleus). It contains motor fibres.
- Superior salivatory and lacrimatory nucleus. It contains motor fibres.
- Nucleus of tractus solitarus (gustatory nucleus). It contains sensory fibres and brings the taste sensations.
- Spinal nucleus of trigeminal system. It contains sensory fibres and brings touch pain temperature sensation of facial nerve.
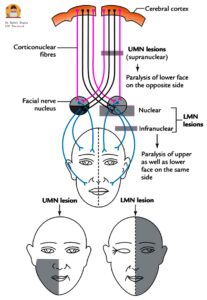
Diagram: Showing distribution of facial muscles paralysis following upper motor and lower motor facial nerve palsy
- Facial nerve nucleus (principle nucleus or branchiomotor nucleus). It is located in the lower part of the pons. It gives rise to motor fibres (Special visceral/ motor efferent(SVE)) of the facial nerve. It supplies all the muscles derived from the second branchial arch i.e. the muscles of facial expression, buccinator, stapedius, platysma, the posterior belly of digastric and stylohyoid. It is responsible for facial expression and elevation of hyoid bone. The supranuclear (upper) part of the nucleus receives fibres from both the cerebral hemispheres and innervates forehead muscles, while the infranuclear part (lower) gets only crossed fibres from one hemisphere. This explains why the function of the forehead is preserved in supranuclear lesions because of bilateral innervation from both cerebral hemispheres. The emotional expressions of the face like smiling and crying are preserved in supranuclear palsy due to thalamonuclear fibres supply to the facial nucleus.
- Superior salivatory and lacrimatory nucleus. It is located in the lower part of the pons. It gives rise to motor fibres (General visceral/ motor efferent (GVE)) of the facial nerve. It supplies the lacrimation glands, salivary glands (submandibular and sublingual glands) and the smaller secretory glands in the nasal mucosa and the palate. They are preganglionic parasympathetic fibres.
- Nucleus of tractus solitarus (gustatory nucleus) – It is located in the medulla oblongata. It receives sensory fibres (Special visceral/ sensory afferent (SVA/GVA)) of facial nerve. It brings taste sensation from anterior 2/3rd of the tongue via chorda tympani and soft and hard palate via greater superficial petrosal nerve.
- Spinal nucleus of trigeminal system (mesencephalic) – It is located in the medulla oblongata. It receives sensory fibres (General somatic/ sensory afferent(GSA)) of the facial nerve. It brings touch pain temperature sensations from the posterosuperior aspect of the external canal, concha and the tympanic membrane.
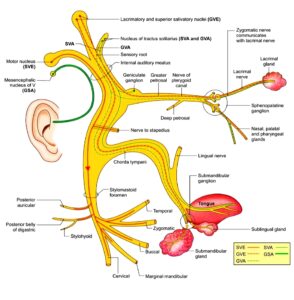
Diagram: Components of facial nerve
COURSE OF FACIAL NERVE.
The facial nerve follows a complex course which can be divided into three parts.
- Intracranial course also known as pontine or cisternal segment (24-25 mm). From origin of facial nerve from pons to internal acoustic meatus. Motor fibres of facial nerve originate from facial nerve nucleus which is located in the lower part of pons. Usually motor fibres of other nuclei’s moves forwards to exit from central nervous system. But motor fibres of facial nerve nucleus, first move backwards towards nucleus of VIth nerve, moves around or hooks around the nucleus of VIth (abducens) and then move forwards to exit the brainstem through cebellopontine angle. Rest of fibres (both motor & sensory) from other nuclei’s (Superior salivatory and lacrimatory nucleus, nucleus of tractus solitarus and Spinal nucleus of trigeminal system) also exit from the brainstem through cebellopontine angle. After the exit through cebellopontine angle, all four fibres are arranged in two bundles. First bundle contains the motor fibres of facial nerve nucleus, while the second bundle contains rest of the three, motor and sensory fibres of facial nerve. The second bundle is the sensory root of facial nerve ‘nervus intermedius’ (nerve to wrisberg) and it joins the first bundle to form the facial nerve. The facial nerve travels through posterior cranial fossa and then enters in the medial end (porus) of the internal acoustic meatus.
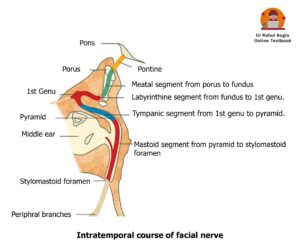
- Intratemporal course: The facial nerve travel through the internal acoustic meatus, enters the bony facial fallopian canal, traverses the middle ear and exits from the stylomastoid foramen. The intra-temporal part is further sub-divided into four segments :
- Meatal segment (8-10 mm) – From porus (medial end) to fundus (lateral end) of internal acoustic meatus. The internal acoustic meatus is present on the anterior wall of posterior cranial fossa which is formed by the posterior surface of petrous part of temporal bone. Facial nerve travels through internal meatus in the anterior-superior quadrant of the IAC. Vestibulocochlear nerve and internal auditory artery also pass through the IAC.
- Labyrinthine segment (4.0 mm) – From fundus to geniculate ganglion (1st genu). From fundus the facial nerve enters bony fallopian canal of facial nerve and move anteriorly to the geniculate ganglion (present on the anterosuperior part of medial wall of middle ear) where nerve takes a sharp ‘hairpin’ 75 degree turn posteriorly forming a first genu (anterior genu). Labyrinthine segment is the narrowest (0.61-0.68 mm), hence most vulnerable to get compressed by oedema or inflammation leading to paralysis. In-addition, the segment is susceptible to low-flow state and vascular compression as it lacks anastomosing arterial cascades. The labyrinthine segment is the shortest segment of the intratemporal course of the facial nerve.
- Tympanic segment (11 mm) – From 1st genu to pyramid. Facial nerve begins from the geniculate ganglion, courses posteroinferiorly to just above the pyramidal eminence. Facial nerve traverses medial to incus, runs posterior-superior to the processus cochlearformis, above the oval window and below the lateral semi-circular canal. Due to the high incidence of fallopian canal dehiscence in tympanic segment, it is the most common site of injury during middle ear surgery.
- Mastoid or vertical segment (13.0 mm) – From pyramid to stylomastoid foramen. Posterior to pyramidal process, the tympanic segment takes second turn inferiorly (forming second genu) to become the mastoid or vertical segment. The nerve continues vertically down the posterior wall of the middle ear and exits through stylomastoid foramen. The mastoid segment is the longest segment of the intratemporal course of the facial nerve. Second genu is the most common site of injury during mastoid surgery.
3. Extracranial course. From stylomastoid foramen to the termination of its peripheral branches. The facial nerve exits from stylomastoid foramen, travels anterior to the posterior belly of the digastric and lateral to the styloid process. Then it enters the parotid gland high up on its posteromedial surface and divides within the gland. It usually divides just behind and superficial to the retromandibular vein and external carotid artery (ECA). The length from stylomastoid foramen to initial intra-parotid bifurcation ranges between 8 -22 mm.
BRANCHES OF FACIAL NERVE
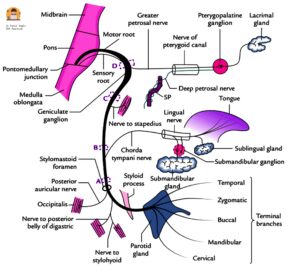
Diagram : Branches of facial nerve
From geniculate ganglion (1st Genu)
- Greater superficial petrosal nerve is the first branch of the facial nerve and carries secretomotor fibres to lacrimal gland and the glands of nasal mucosa and palate.
From mastoid segment
- Nerve to Stapedius arises at the level of 2nd genu and supplies the stapedius muscle.
- Chorda tympani arises from the middle of vertical segment, 5-6 mm above the stylomastoid foramen. It enters the middle ear through posterior canaliculus at the junction of the lateral and posterior walls of middle ear. It runs on the medial surface of the tympanic membrane between its mucosal and fibrous layers. On malleus, it runs medially just below the neck of malleus and above the attachment of tendon of tensor tympani. It further continue forwards and leave the middle ear through anterior canaliculus. It carries taste sensation from anterior two-thirds of tongue and supplies secretomotor fibres to the submaxillary and sublingual salivary glands.
At the stylomastoid foramen
- Posterior Auricular Nerve: After exiting the stylomastoid foramen, the facial nerve gives off a posterior auricular branch, which supplies auricular muscles (superior & posterior) and occipitalis muscle and communicates with auricular branch of vagus.
- Small Muscular Branches.
- Nerve to stylohyoid: It innervates the stylohyoid muscle (a suprahyoid muscle of the neck). It elevates the hyoid bone.
- Nerve to posterior belly of digastric: It innervates the posterior belly of the digastric muscle (a suprahyoid muscle of the neck). It elevates the hyoid bone.
Communicating Branch
It joins auricular branch of vagus and supplies the concha, posterior auricular groove, posterior meatus and the outer surface of tympanic membrane.
Peripheral Branches to the face.
It forms two divisions:
- Upper temporofacial part (further divided into temporal, zygomatic, upper buccal branch).
- Lower cervicofacial part (further divided into lower buccal, mandibular and cervical branches).
Both divisions together form pes anserinus (goose-foot). Muscles supplied by peripheral branches of facial nerve are:
- Temporal branches: supply the frontalis, orbicularis oculi and corrugator supercilli muscles.
- Zygomatic branches: supply the orbicularis oculi muscle.
- Buccal branches: supply the orbicularis oris, buccinator and zygomaticus muscles.
- Marginal mandibular branch: supplies the depressor labii inferioris, depressor anguli oris and mentalis muscles.
- Cervical branch: supplies the platysma muscle in the neck.
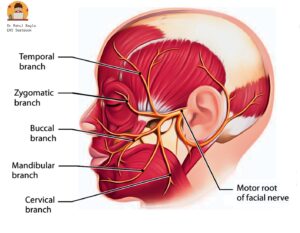
Diagram : Peripheral branches of facial nerve
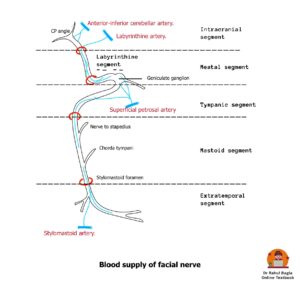
VASCULAR SUPPLY OF FACIAL NERVE
The three main arteries supplying the facial nerve are:
- Labyrinthine artery, a branch of the anterior inferior cerebellar artery.
- Superior petrosal artery, a branch of the middle meningeal artery.
- Stylomastoid artery, a branch of the postauricular artery.
| Area | Blood supply |
| Cerebellopontine angle | Supplied by anterior-inferior cerebellar artery. |
| Intracranial, meatal and labyrinthine parts | Supplied by labyrinthine artery. |
| Geniculate ganglion and adjacent areas | Supplied by the superficial petrosal artery branch of the middle meningeal artery. |
| Tympanic and mastoid segments | Supplied by the facial arch, formed by the superficial petrosal branch of the middle meningeal artery and stylomastoid branch of posterior auricular artery. |
| Stylomastoid foramen to the parotid gland | The posterior auricular and occipital arteries and their branches, including the stylomastoid artery. |
| The temporofacial and cervicofacial branches | Supplied by collaterals of the superficial temporal, transverse facial, facial and maxillary arteries. |
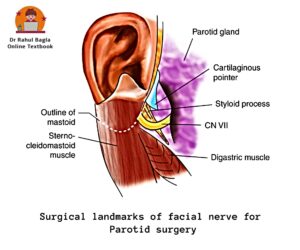
SURGICAL LANDMARKS OF FACIAL NERVE
For middle ear and mastoid surgery
- Processus cochleariformis. It demarcates the geniculate ganglion which lies just anterior to it. Tympanic segment of the nerve starts at this level.
- Oval window and horizontal canal. The facial nerve runs above the oval window (stapes) and below the horizontal canal.
- Short process of incus. Facial nerve lies medial to the short process of incus at the level of aditus.
- Pyramid. Nerve runs behind the pyramid and the posterior tympanic sulcus.
- Tympanomastoid suture. In vertical or mastoid segment, nerve runs behind this suture.
- Digastric ridge. The nerve leaves the mastoid at the anterior end of digastric ridge.
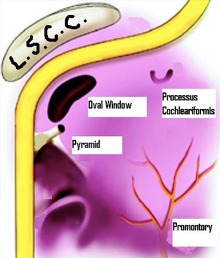
Surgical landmarks of the facial nerve in middle ear and mastoid surgery.
For parotid surgery
- Tragal pointer. The main trunk of nerve lies 1 cm medial and slightly antero-inferior to the pointer. Tragal pointer is a sharp triangular piece of pinna cartilage and it “points” to the nerve.
- Posterior belly of digastric. When retrograde dissection of this muscle is done along its upper border up to its attachment with the mastoid process, the facial nerve is seen passing between the mastoid and the styloid process.
- Tympano-mastoid suture. The trunk of the nerve can be identified 6–8mm below the inferior ‘drop off’ of the tympano-mastoid suture.
- Styloid process. The nerve passes laterally to the styloid process.
ANOMALIES OF FACIAL NERVE
Nerve anomalies are more common in congenitally malformed ears; hence the clinician should be careful while operating such ears.
- Bony dehiscence: The most common site of absence or dehiscence of bony cover is tympanic segment over the oval window . Other sites: near geniculate ganglion or in area of retrofacial mastoid cells. A dehiscent nerve is likely to be injured during surgery and infections of middle ear or mastoid.
- Prolapse of nerve: The dehiscent nerve may prolapse over the stapes creating difficulty in stapes surgery or ossicular reconstruction surgery.
- Hump: The nerve at times makes a hump posteriorly nearthe horizontal canal , hence vulnerable to injury while during mastoid surgery.
- Bifurcation and trifurcation. The vertical part offacial nerve bifurcates or trifurcates, each may occupy different canals and exiting through individual foramen.
- Bifurcation and enclosing the stapes. The nervebifurcates proximal to oval window—one of the branch passes above and the other below it and then both re-unite.
- Between oval and round windows. Just before ovalwindow the nerve crosses the middle ear between oval and round windows.

HISTOLOGY OF NERVE
A peripheral nerve fibre is covered by three layers of connective tissue. Each nerve fiber is surrounded by endoneurium. A group of many fibres form fascicle bound together by another connective tissue called perineurium .There is an outermost layer of additional connective tissue surrounding many fascicles, called as epineurium. The three connective tissue layers maintain tensile strength, preventing its deterioration by cholesteatoma or vestibular schwannomas. The main glial cells of peripheral nervous system are schwann cells which provide trophic support to neurons.
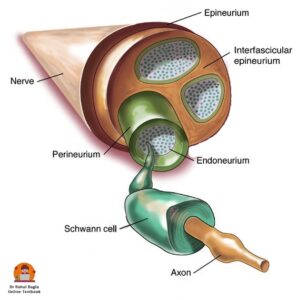
Diagram: Showing cross section structure of nerve
PATHOPHYSIOLOGY OF NERVE INJURY
In 1941, Seddon introduced a classification of nerve fibre injury based on types of nerve fibre injury and continuity of the nerve.
- Neuropraxia is the least severe form of injury caused due to disruption to blood supply (ischaemia) or compression of the nerve. Release of the pressure results in a rapid and complete recovery of function (6-8 weeks). There is no residual dysfunction and wallerian degeneration does not occur.
- Axonotmesis is a more severe form of crush injuryor sectioning of an axon with disruption of the axoplasmic flow but with intact epineurium. All three connective tissue layers are preserved. Wallerian degeneration occurs distal to the site of injury over a period of 72-96 hours following injury. Regeneration occurs over weeks to days of injury.
- Neurotmesis is the most severe form of nerve injury caused due to severe contusion , stretch or laceration. There is complete loss of sensory, motor function. Treatment involves some form of surgical intervention .
Sir Sydney Sunderland in 1951 described axonotmesis of Seddon’s classification in a more detailed fashion and his classification is now widely accepted.
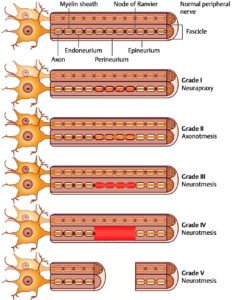
- 1° = Injury is reversible (as blockage to axoplasmic flow is partial) and full recovery is seen (Neurapraxia).
- 2° = Wallerian degeneration occurs. There is loss of axons with preserved endo-neural architecture. Recovery is good and usually complete (Axonotmesis).
- 3° = Disruption of endoneurium occurs. There is partial recovery, axons of one tube can grow into another. Synkinesis may occur (Neurotmesis).
- 4° = Disruption of perineurium in addition to above, only epineurium is intact. There is partial transection of nerve. Scarring will impair nerve regeneration of and poor recovery is seen.
- 5° = Disruption of epineurium in addition to above results in total disruption of nerve continuity (complete nerve transection); recovery requires surgical intervention.
1°, 2°,3° are seen in viral and inflammatory disorders while 4°and 5° are reported in surgical or accidental trauma and neoplasm.
EVALUATION OF FACIAL NERVE PALSY
- History. The diagnosis can be made on the basis of a thorough history, physical examination and diagnostic testing when required. The time of onset, duration and progression of the disease may indicate towards its aetiology and determine prognosis. The longer the duration of palsy, lesser the chances of spontaneous recovery. Recent H/o surgery, facial/ head trauma, ear complaints/ vertigo, headache must be taken. Concurrent medical conditions such as diabetes, pregnancy, autoimmune disorders and cancer should be noted.
- Bell’s palsy is mostly idiopathic, but following clinical presentations should raise a suspicion of an underlying neoplasm and needs to be investigated thoroughly.
- Progressive facial nerve palsy > 3 weeks
- Or an incomplete facial nerve palsy that does not start to recover after 3–6 weeks and
- Ipsilateral recurrent facial palsy.
- However, contralateral recurrence of facial nerve palsy is almost always benign.
- Physical examination. Full head, neck, otologic and cranial nerve examination. Signs of facial injury-laceration/ haematoma/ bruise. Attempt to localize exact site of lesion along the course of the facial nerve i.e. intracranial, intratemporal or extra-cranial.
- House-Brackmann grading system for facial palsy: Since the mid-1980s, the House-Brackmann system is widely used for grading of facial palsy. The degree of facial weakness should be recorded from the time of onset of facial palsy.
| Grade | Description | Characteristics |
| I | Normal | Normal facial function |
| II | Mild dysfunction | Slight weakness or synkinesis |
| III | Moderate dysfunction | Obvious asymmetry, but not disfiguring, synkinesis, contracture, or hemifacial spasm, complete closure with effort |
| IV | Moderately severe dysfunction | Obvious weakness or disfiguring asymmetry, normal symmetry and tone at rest, incomplete eye closure |
| V | Severe dysfunction | Barely perceptible motion, asymmetry at rest |
| VI | Total paralysis | No movement |
ELECTRODIAGNOSTIC TESTS. These tests utilize electrical stimulation to assess nerve function and are most commonly used. The electrophysiological test is able to demonstrate degeneration as early as 3 days after onset. This information is useful to detect the degree of dysfunction, time to do surgical decompression of the nerve and also, predict prognosis.
- Minimal Nerve Excitability Test. It compares amount of transcutaneous current threshold required to elicit minimal muscle contraction on normal versus paralysed sides. The nerve isexcited by steadily increasing intensity till facial twitch is just noticeable. A difference of 3.5 m amp or more is significant and indicates poor recovery. No difference is seen between the normal and paralyzed side in conduction block. In other injuries, where degeneration sets in, nerve excitability is gradually lost. Degeneration of fibres is detectable > 48–72 h of its onset.
- Maximal Stimulation Test: The intensity of current level required to achieve maximum facial movement is recorded and compared with the normal side. Reduced or absent response even with maximal stimulation is suggestive of nerve degeneration and the recovery is usually incomplete. The above two tests are rarely used due to limitations in terms of accuracy, reproducibility, inter-observer variation and does not carry any prognostic value.
- Electroneuronography (ENoG ) is the objective measure of facial nerve integrity and carries prognostic value. ENoG is most useful between 4 and 21 days of the onset of complete paralysis and has no role in first 3 days. A supra-maximal stimulus is delivered to the facial nerve trunk at the stylomastoid foramen. The stimulation electrode is located at the stylomastoid foramen and the recording electrode is located near the nasolabial fold to pick up evoked biphasic compound muscle action potential (CMAP). The action potential of paralysed side is compared with the normal side (which serves as a control).
- If the CMAP amplitude on the affected side is 10% of the normal side, then 90% degeneration of axons has been sustained.
- Degeneration of >90% occurring in the first 14 days of complete paralysis has a poor recovery rate
- Faster rate of degeneration occurring < 14 days has a still poorer prognosis.
- Electromyography (EMG). Electroneuronography (ENoG) and electromyography (EMG) are now most commonly used by ENT surgeons in clinical practice. EMG records active motor unit potentials of the orbicularis oculi muscles during rest and voluntary contraction. Electromyography is useful in planning reanimation procedures in long-standing cases of facial paralysis. It measures:
- Fibrillation potentials (evidence of Wallerian degeneration appears 2-3 weeks after denervation).
- Polyphasic innervation potentials (early signs of re-innervation appear 6–12 weeks prior to clinical evidence of facial function)
- Presence of normal or polyphasic potentials after 1 year of injury suggests ongoing re-innervation and there is no need for reanimation procedure. Follow-up is advocated.
- Presence of fibrillation potentials indicate lower motor neuron denervation, but intact motor end plates. Surgical exploration is needed to maintain nerve continuity, either by end-to-end anastomosis, interposition grafting, re-routing or re-innervation techniques.
- Electrical silence means atrophy of motor end plates and fibrous replacement of muscle. There is need for muscle transfer or transposition procedures rather than nerve substitution.
ENoG and EMG tests provide information about the facial nerve distal to the stylomastoid foramen. These tests are required to prognosticate in cases of facial paralysis and in deciding the procedure for reanimation, i.e. nerve substitution versus muscle transposition or sling operation.
- Transcranial magnetic stimulation. is used to stimulate the facialnerve within the cranium in exactly the same way as conventional electrostimulation.
LOCALIZATION OF SITE OF LESION
A. Central facial paralysis. Function of forehead is preserved because of bilateral innervation of frontalis muscle from both cerebral hemispheres. There is paralysis of only the lower half of face on the contralateral side. The emotional expressions of face like smiling and crying are also preserved. Central facial paralysis is caused by brain abscess, Pontine gliomas, Poliomyelitis, Multiple sclerosis and cerebrovascular accidents (e.g. haemorrhage, embolism).
B. Peripheral facial paralysis. All the muscles of the face on the involved side are paralyzed. Patient is unable to frown, close the eye, purse the lips or whistle.
| Site of lesion | Signs |
| Level of nucleus | Associated paralysis of VIth nerve. |
| Cerebellopontine angle | Identified by the presence of vestibular and auditory defects and involvement of other cranial nerves such as Vth, IXth, Xth and XIth. |
| Bony fallopian canal, from IAC to stylomastoid foramen | Localized by topo-diagnostic tests given above. |
| Extra-temporal segment in parotid gland | Affects only the motor functions of nerve. It may sometimes be incomplete as some branches of the nerve may not be involved in tumour or trauma. |
Topognosis tests. Topographic diagnosis of facial nerve lesions refers to the functional testing of an individual facial nerve to pinpoint the site of injury.
| Test | Nerve branch assessed | Technique considerations | Assessment/ Outcome |
| Schirmer’s test | Greater (superficial) petrosal nerve | Eye is gently dried of excess tears or use Local anaesthetic drops. A Strip of filter paper is placed in the inferior conjunctival fornix of each eye for 5 minutes and patient is asked to close eyes. The length of paper moistened is compared between eyes | A reduction of 25% or a total of less than 25 mm is abnormal and indicates lesion proximal to the geniculate ganglion. |
| Stapedial reflex | Nerve to stapedius muscle | Can be tested by tympanometry. | Reflex is lost when lesion is above the nerve to stapedius. |
| Electrogustometry | Chorda tympani | The tongue is stimulated electrically to produce a metallic taste and the two sides are compared. Or a drop of salt or sugar solution placed on one side of the protruded tongue | Threshold of the test is compared between sides. Impairment of taste indicates lesion above the chorda tympani. |
| Salivary flow testing | Chorda tympani | Polythene tubes are placed into both Wharton ducts and salivary flow (no. of drops) is measured over a minute following a gustatory stimulus (6% citric acid on anterior part of tongue) | A reduction of 25% or more indicates lesion above the chorda. |
Diagram: Topographical localization of the VIIth nerve lesions.
- Suprageniculate or transgeniculate lesion. Secretomotor fibres to the lacrimal gland leave at the geniculate ganglion and are interrupted in lesions situated at/or proximal to the geniculate ganglion.
- Suprastapedial lesions cause loss of stapedial reflex and taste but preserve lacrimation.
- Infrastapedial lesions cause loss of taste but preserve stapedial reflex and lacrimation.
- Infrachordal lesions cause loss of facial motor function alone.
SEQUELAE/ COMPLICATIONS OF FACIAL PARALYSIS
Peripheral facial paralysis due to any cause may result in any of the following complications:
1. Incomplete Recovery. Facial asymmetry completely not resolved.It results in persistent tears in affected eye due to incomplete eye closure, difficulty in speaking clearly, involuntary drooling of saliva and difficulty in drinking and eating leading to psychological and social stigma.
2. Exposure Keratitis. Due to incomplete closure of eye, tear film from the cornea evaporates causing dryness, foreign body sensation, blurring of vision, exposure keratitis and corneal ulcer. Treatment of exposure keratitis is:
- Frequent use of eye drops (containing hydroxypropyl cellulose, hydroxypropyl methylcellulose or polyvinyl) frequently during the daytime, whilst at night, eye should be taped closed after putting thicker ointments containing petroleum, mineral oil or lanolin.
- Corneal protection with lubrication and patching.
- Use of large-lens sunglasses.
- Patients having long-term facial nerve palsy are advised to close their eye manually using a finger as well as attempting to stretch the upper lid in order to prevent shortening caused by unopposed action of levator palpebrae superioris muscle.
- Temporary tarsorrhaphy may also be indicated. Eye closure can also be improved by using gold-weight implant sutured to the tarsal plate deep to levator palpebrae muscle.
3. Crocodile tears (Gustatory Lacrimation). During recovery from facial nerve paralysis, the regenerating parasympathetic fibres of the salivary gland undergo synkinesis and misdirectly starts supplying the lacrimal gland instead of supplying the salivary glands. Therefore while eating food, instead of developing salivation, patient develops paroxysmal ipsilateral shedding of tears (lacrimation). Treatment is sectioning of greater superficial petrosal nerve or tympanic neurectomy.
4. Frey’s Syndrome (Gustatory Sweating). It occurs following parotid or neck dissection surgery. The overlying sweat glands gets aberrant reinnervation from postganglionic parasympathetic neurons resulting in flushing and sweating over the parotid area, instead of salivation during mastication.
5. Synkinesis (Simultaneous movement). It occurs due to abnormal regeneration of facial nerve fibers, which cross innervate to another nerve group of fibres, causing unwanted facial movement. It usually occurs following surgery or surgical repair of facial nerve. Patient may experience eye closure during a smile and laugh or while closing the eye, there is twitching of the corner of mouth. Treatment options are physical therapy, botulinum toxin, surgery.
6. Tics and Spasms. These are involuntary twitching of the eye and facial muscles on one side of the face, occurs as a result of faulty regeneration of fibres. It usually seen in childhood.
7. Contractures. Due to prolonged facial palsy, the facial muscles gets contracted and become atrophic. Shortening of the facial muscles affects the movements of face. Usually no facial asymmetry is visible during rest position. But sometimes the affected side of the face may appear slightly lifted and eye may appear smaller as compared to the other eye.
———— End of the chapter ————
Download full PDF Link:
Facial Nerve Paralysis Best Lecture Notes Dr Rahul Bagla ENT Textbook
Reference Textbooks.
- Scott-Brown, Textbook of Otorhinolaryngology-Head and Neck Surgery.
- Glasscock-Shambaugh, Textbook of Surgery of the Ear.
- P L Dhingra, Textbook of Diseases of Ear, Nose and Throat.
- Hazarika P, Textbook of Ear Nose Throat And Head Neck Surgery Clinical Practical.
- Mohan Bansal, Textbook of Diseases of Ear, Nose and Throat Head and Neck surgery.
- W. Arnold, U. Ganzer, Textbook of Otorhinolaryngology, Head and Neck Surgery.
- Salah Mansour, Textbook of Comprehensive and Clinical Anatomy of the Middle Ear.
- Susan Standring, Gray’s Anatomy.
- Orlando Guntinas-Lichius, Textbook of Facial Nerve Disorders and Diseases: Diagnosis and Management.
Author:

Dr. Rahul Bagla
MBBS (MAMC, Delhi) MS ENT (UCMS, Delhi)
Fellow Rhinoplasty & Facial Plastic Surgery.
Renowned Teaching Faculty
Mail: msrahulbagla@gmail.com
India
———– Follow us on social media ————
- Follow our Facebook page: https://www.facebook.com/Dr.Rahul.Bagla.UCMS
- Follow our Instagram page: https://www.instagram.com/dr.rahulbagla/
- Subscribe to our Youtube channel: https://www.youtube.com/@Drrahulbagla
- Please read. Anatomy of External Ear. https://www.entlecture.com/anatomy-of-ear/
- Please read. Anatomy of Temporal Bone. https://www.entlecture.com/anatomy-of-temporal-bone/
- Please read. Stenger’s, Chimani Moos, Teal test. https://www.entlecture.com/special-tuning-fork-tests/
Keywords: Anatomy of facial nerve, Facial Nerve Branches, Facial Nerve Palsy, Facial Nerve Course, Facial nerve embryology, Components of facial nerve, Course of facial nerve, Bell’s palsy, Ramsay hunt syndrome, Fractures of temporal bone, Facial nerve grading systems, Understanding Facial Nerve Grading Systems: A Comprehensive Guide, House-Brackmann scale interpretation, How to Interpret the House-Brackmann Scale for Facial Paralysis, Facial nerve palsy ocular symptoms, Recognizing Ocular Symptoms in Facial Nerve Palsy, Facial nerve paralysis rehabilitation exercises, Effective Rehabilitation Exercises for Facial Nerve Paralysis, Facial nerve palsy differential diagnosis, Differential Diagnosis in Facial Nerve Palsy: What to Consider, Facial nerve paralysis grading scales, An Overview of Grading Scales for Facial Nerve Paralysis, Facial nerve palsy ocular complications, Managing Ocular Complications in Facial Nerve Palsy, Facial nerve paralysis treatment options, Exploring Treatment Options for Facial Nerve Paralysis, Facial nerve palsy recovery timeline, What to Expect: Recovery Timeline for Facial Nerve Palsy, Facial nerve anatomy clinical relevance, The Clinical Relevance of Facial Nerve Anatomy.

Wonderful
Thanks
Thank you sir—boon for both PG and MBBS Students.
Thanks
Wonderful job sir.
Thanks
Amazing content sir
Thanks
One thing, it was said that Facial Nerve branches stapedius nerve at 2nd genu, but I don’t see this 2nd genu mentioned anywhere else. What is it exactly?
Amazing notes, this website is my favorite ENT source!